Abstract
Neuroethics, a recently modernized field at the intersection of bioethics and neuroscience, is founded on centuries of discussion of the ethical issues associated with mind and behavior. Broadly defined, neuroethics is concerned with ethical, legal and social policy implications of neuroscience, and with aspects of neuroscience research itself. Advances in neuroscience increasingly challenge long-held views of the self and the individual's relationship to society. Neuroscience also has led to innovations in clinical medicine that have not only therapeutic but also non-therapeutic dimensions that extend well beyond previously charted boundaries. The exponential increase in cross-disciplinary research, the commercialization of cognitive neuroscience, the impetus for training in ethics, and the increased attention being paid to public understanding of science all illuminate the important role of neuroethics in neuroscience.
Introduction
Although questions about the nature and origins of human identity and behavior have been the focus of philosophical discussions dating back to antiquity, it is only in the past few centuries that scientists have sought to understand the intricacies of the structure and function of the nervous system and, more recently, the nature of mind and brain [1]. Although there is a widespread notion that scientific research and especially new technologies bring new ethical problems, ethical concerns reflect the values of the society. New technologies and scientific findings create the circumstances in which ethical issues pose new challenges.
Bioethics is a broad field that links the biological sciences with ethical concerns [2]. Biomedical ethics, as a subfield of bioethics, focuses on issues related to basic and clinical research. Like medical ethics, which deals with issues in the healthcare setting, one of the core tenets of biomedical ethics is respect for the individual. The opportunity for and elements of making an informed decision regarding participation in research exemplifies the issues central to the field. The emergence of biomedical ethics has led to landmark changes in current approaches to the ethics of human experimentation and respect for autonomy. New ethical issues build on this legacy. Neuroethics intersects with biomedical ethics in that, broadly defined, neuroethics is concerned with ethical, legal and social implications of neuroscience research findings, and with the nature of the research itself [3].
The term ‘neuroethics’ has been used to refer to ethical issues associated with child-rearing [4], technological advances [5], and the neurological basis of ethical thought and behavior [6]. With more and more studies touching upon personal and societal phenomena [7], neuroethics and the terrain it covers are continuously expanding. Our goal here is to explore the foundations of ethics in neuroscience and to situate the evolving field of neuroethics within this history and rich precedent. To achieve this goal, we review past discussions of ethical issues related to neuroscience, the formation of professional organizations and their ethics priorities, and then focus on various facets of the field.
Ethics in neuroscience
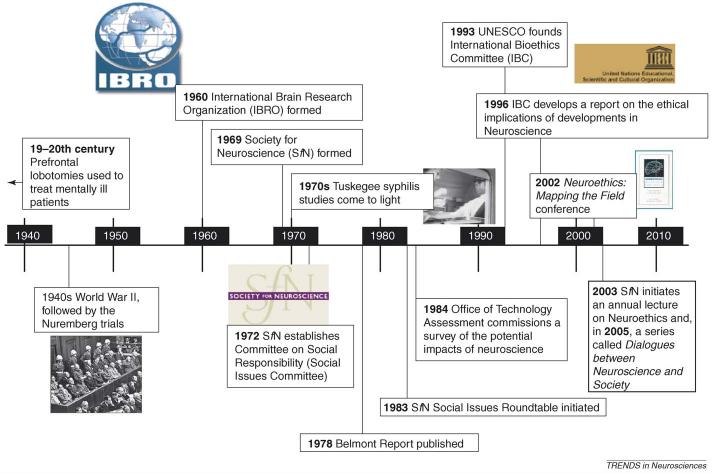
Perhaps no other event has shaped biomedical ethics more than the medical research and practice carried out by the Third Reich during World War II (Figure 1). Whereas considerable attention has been devoted to this topic in the biomedical ethics literature, little appears in contemporary neuroscience and neuroethics publications. At a DANA Foundation meeting during the 2005 annual meeting of the Society for Neuroscience (SfN, http://sfn.org), Eric Kandel spoke about this important past (Box 1) [8-10].
Figure 1.
Milestones in the history of ethics in neuroscience. From left to right: prefrontal lobotomies were introduced for treatment of mentally ill patients in the late 19th and early 20th centuries; human experimentation during the 1930s and 1940s led to the Nuremberg trials; two major professional neuroscience organizations were established in the 1960s, and committees and roundtables devoted to social issues were created within these organizations in the 1970s and 1980s; revelations of the Tuskegee studies and other human subject violations in research led to the publication of the Belmont Report, also in the 1970s; the Office of Technology Assessment surveyed the potential impact of neuroscience in 1984; UNESCO founded the International Bioethics Committee (IBC) in 1993, and the IBC developed an independent report on the ethical implications of developments in neuroscience in 1996; the Dana Foundation hosted a meeting called ‘Neuroethics: Mapping the Field’ in San Francisco (CA, USA) in 2002; and the Society for Neuroscience extended its commitment to discussions about social issues in neuroscience, formally begun in 1983, to an annual lecture on Neuroethics in 2003 and a ‘Dialogues between Neuroscience and Society’ series in 2005.
Box 1. Ethical values in science.
When thinking about ethical values in science, one is tempted to assume that these values are obvious; they are implicit in what we do. We believe that scientists who are well trained and serious about their work bring with them ethical values that allow them to think through, on their own, the social implications of their work and its consequences for others.
It was in this context that I was reminded recently, in writing about my personal and professional life, that this has not always been so. Even scientists who appear to themselves to be well intentioned, and may at times even appear to be so to others, can start out on a course of action that imperceptibly – to them – becomes completely unethical.
I was born in Vienna and came to the USA at the age of nine, one year after Hitler marched into Austria. I later went to medical school and trained in psychiatry. Subsequently I became a molecular geneticist interested in learning and memory. The specific personal example that reminded me of the critical importance of ethical deliberations came from my reading about the scientific origins of the Holocaust. This frightening example came uncomfortably close to home, not only because of my origins but also because of my later professional experiences.
Let me begin by putting this example into the larger context of 20th century psychiatry and genetics. As has been emphasized by Daniel Kevles (1985) [8], at the beginning of the 20th century, almost all geneticists, including some of the most serious and best intentioned, were eugenicists. In 1883 Darwin's cousin, Francis Galton, first advanced the idea that one should strengthen biological groups based on hereditary worth. Following Galton, a common belief emerged among geneticists that one of the functions of genetics was to make the human race better by discouraging the reproductive capability of those who are genetically inferior, and encouraging the reproductive capability of those who are healthy, vigorous, and genetically superior. Although a European invention, this eugenic view was advocated by geneticists throughout the world and it had a particularly strong representation in the USA.
Eugenics was soon transformed from a belief into a pattern of action. The first people to carry out this transformation were psychiatrists, physicians to whom people entrusted the care of the ill. In Germany, psychiatrists were responsible for the care of patients with mental retardation, congenital syphilis, infantile dementias, as well as other forms of mental illness. In the 1920s, they began discussing among themselves the social burden that institutionalized, mentally retarded children and adults placed on society. At first, these were only discussions. The Weimar Constitution of post World War I Germany prevented the use of the vasectomy technique and thereby prevented German psychiatrists from carrying out routine sterilizations. Paradoxically, in the USA and in England where this discussion also was going on, and where the eugenics movement was as strong as in Germany, vasectomy was not prohibited. But while the more mature and transparent political systems in America and England allowed open criticisms which prohibited sterilization from being carried out as a national policy, the fragile Weimar democracy, lacking these political safeguards, repealed their anti-vasectomy laws because physicians argued that without a radical eugenics program, the German State would suffer economic and social harm. As a result, psychiatrists who initially only entertained the idea now began to act upon it and sterilized people who were severely mentally retarded. They then began to extend this practice to schizophrenic patients and since this was a heritable disease, sterilization was recommended for first-degree relatives. With time the discussions moved to sterilization of the mentally retarded and turned to euthanasia. For several Germans, widespread compulsory sterilization became an important mission that led them later to embrace National Socialism because Hitler picked up this theme and developed it in Mein Kampf, where he described the sacred myth of sterilization as a modern medical means for insuring the purity of the race.
As a result, by the time Hitler came to power in 1933, aspects of the German psychiatric community and the medical community at large, as well as biologists interested in eugenics, had become comfortable with the idea that systematic sterilization and euthanasia were acceptable social practices designed to purify the race – first the mentally retarded, then the mentally ill, and then the others, burdens to society, the Jews and the gypsies. This phase of German psychiatry has been well documented by Robert Lifton and independently by Benno Muller-Hill. Recently this historical effort was dramatized in the Holocaust Museum in Washington, DC in its exhibit entitled The Scientific Origins of the Holocaust. As Muller-Hill points out, in Germany between 1933 and 1945, physicians substituted ideology for philosophy, and Lifton traces in detail how physicians were transformed from healers to killers. Thus, one of the roads which led to the Holocaust was paved by what were originally presumably well-intentioned, reasonable people acting in what they thought was a reasonable way, but without exposing their vision to the open criticism of a stable democratic society where a larger philosophical discussion about its ethical relevance could be undertaken. Later, interviewing some of those people involved in the eugenics program, both Lifton and Muller-Hill were struck by the fact that most represented what Hannah Arendt has called the banality of evil. They were not devils or conscious killers but middle class people blind to certain ethical dilemmas.
Thus, ethics in science is important because it is essential that the issues we confront in dealing with the mind be considered not only by the few narrow groups of individuals originally involved in delineating them, but by the larger group who can much better evaluate the ethical significance of these issues for society. I am here tempted to paraphrase in the context of ethics what Reinhold Niebuhr, the great Columbia theologian said about democracy: the people's capability for doing good makes biological ethics desirable; their capability for evil makes biological ethics necessary.
– Eric Kandel (November 2005)
Coincident with the birth of the eugenics movement that led to the experiments perpetrated during World War II was another significant event: the popularization of psychosurgery for the treatment of mentally ill patients [11,12]. During the late 19th century, the clinicopathological correlations between brain, thought and behavior became apparent, and through much of the first half of the 20th century surgeries involving the prefrontal lobes brought relief to patients who had treatment-resistant disease. However, these procedures also dramatically changed the personalities of patients and raised significant concerns about efficacy and the personal cost of therapy [11]. Yet well into the 1960s, when there was considerable social unrest in major cities in the USA, researchers still proposed psychosurgery as an effective treatment for violent behavior. The outcry of those opposed to this modern application of neuroscience – updated to surgeries involving limbic structures – raised awareness of the potential for misuse, indeed abusive use, of neuroscience findings and methods to address social problems that have complex causes [13-15].
Ever-increasing research on brain and behavior in a wide range of disciplines prompted the establishment of the International Brain Research Organization (IBRO, http://www.ibro.org) in 1960 under the auspices of United Nations Educational, Scientific and Cultural Organization (UNESCO, http://portal.unesco.org). Other regional societies focusing on neuroscience followed, including the SfN in the USA in 1969. The primary focus of these professional societies was to advance neuroscience research. Little attention was paid to its social implications. However, in 1972, the SfN created a Committee on Social Responsibility (which later became the Social Issues Committee, SIC) specifically for the purpose of informing the membership and the public about the social implications of the field.
The committee was a voice of protest against political repression of neuroscientists in countries around the world, and it addressed the development of regulations for the use of laboratory animals in research, especially primates. In 1983, the SIC initiated an annual Social Issues Roundtable, the first of which was a symposium on sexual differences in the brain. In subsequent years, these Roundtables focused on various topics including cognitive enhancement, when ‘brain life’ begins, brain death, neurotoxicity of food additives, and the use of fetal tissue for treating neurological disease. In 2003, the SfN initiated an annual special lecture on neuroethics and, in 2005, the society launched a series called ‘Dialogues between Neuroscience and Society’. The 2005 decommissioning of the SIC hopefully suggests that there has been a transition of neuroethics issues, from a special interest of the society to a fully integrated part of the society's mission.
In the early 1980s, the US Congressional Office of Technology Assessment (OTA) commissioned a survey of the potential impact of neuroscience as part of a project examining the implications of technology for aging [16]. This report highlighted diverse medical benefits of neuroscience research, not only for neurological, psychiatric and genetic brain diseases, but also for other non-neurological conditions such as cardiovascular and parasitic disease. In addition, the OTA report considered the implications of then new technologies including recombinant DNA technologies, brain grafting and imaging. This report also explicitly examined the potential impact of neuroscience in the workplace, the criminal justice system, and the classroom with regard to shift-work, stress, neurotoxins, drug abuse, learning disabilities and sex differences.
In 1995, UNESCO's International Bioethics Committee (IBC; founded in 1993) developed a similar study to explore ethics and the neurosciences [17]. The report highlighted the challenges of behavioral research involving deception and manipulation, and of research involving patients, children and captive populations who might have limited capacity to make informed and voluntary decisions about participation. The IBC report also noted the particular difficulty of disseminating neuroscience findings to the public, citing possible misunderstanding of behavioral genetics results as an example.
Overall, an unprecedented level of attention to the ethical implications of biomedical research in the late 1900s and advances in molecular biology combined to have an important role in shaping ethics in neuroscience. Following World War II, the Nuremberg Code, the International Code of Medical Ethics, the Code of the British Medical Association, and the World Medical Association's Declaration of Helsinki all laid out ethical principles regarding research with human subjects. In the early 1970s, the Tuskegee Syphilis studies came to light, revealing forty years (1932–1972) of research conducted by the US Public Health Service on poor black men who has syphilis in rural Alabama. What began as a small treatment program became the longest non-therapeutic observational study in medical history. Patients were denied access to treatment even after penicillin was found to cure the disease. The goal was not to cure the men but to collect data from their autopsies once they succumbed [18].In response, the US Congress created a commission to identify and articulate ethical principles to guide the acceptable use of human volunteers and subjects in biomedical research. The commission's Belmont Report [19], together with setting up of institutional review boards to implement the principles outlined in the report, prompted new attention to ethical conduct in both biomedical research and medical practice.
At the same time that advances in molecular biology were leading to the rapid identification of genes and genetic markers, discussion grew regarding the implications of molecular genetics, including the possibility of genetic testing for hereditary diseases such as Down's syndrome, Tay Sachs disease and Huntington's disease. The rise of genetic testing brought with it concern about the potential misuse of test results in the diagnosis and prediction of disease, employment and access to health insurance. Advances in molecular genetics also led to initiation of the Human Genome Project (HGP), jointly sponsored by the US Department of Energy and the National Institutes of Health. Especially noteworthy is the fact that 3–5% of HGP funds were designated for support of studies of the ethical, legal and social issues (ELSI) of research. This was an unprecedented step, and the establishment of ELSI funding can be viewed as an acknowledgement of both the larger societal impact of science and the responsibility that the scientific community bears in considering ethical implications of science in depth. A natural consequence of the cross-fertilization of all these activities was a growing awareness of the ethical implications of neuroscience research, with articles written both by neuroscientists and ethicists [20] and an explosion of activity in the field that has come to be known as neuroethics.
Neuroethics
Drawing on the history of ethics in neuroscience, and on the fast pace at which neuroscience has been advancing, modern neuroethics encompasses theoretical, empirical, practical and policy issues at the intersection of neuroscience and bioethics. One way to group these issues is into the four major areas highlighted at a 2002 meeting called Neuroethics – Mapping the Field [21]: (i) the implications of neuroscience for notions of the self, agency and responsibility; (ii) social policy applications that make new resources such as healthcare and education available to society; (iii) therapeutic intervention through advances in clinical practice; and (iv) public discourse and training.
Neuroscience of the self, agency and responsibility
Current research studies prompt discussion of human nature and the individual's place in society. Specifically, they raise questions about the biological basis of personality and social behavior, and the role of neurobiology in decision-making. Exploration of the self is thus the most unifying theme of the four as the concept of self inextricably intersects with the other three areas.
Antonio Damasio's studies, both of the disinhibited behaviors of patients with ventromedial frontal pathology and of the role of emotion in gauging context-appropriate behavior, provide a strong foundation for current explorations of the self and agency in neuropathology [22]. Drawing on this work, Kenneth Schaffner has argued that brain circuits do not prima facie generate moral decisions. Rather, in what Schaffner calls creeping or partial reductionism, the self is formed through the aggregate of an initial set of conditions and subsequent states and choices might or might not be predictable based on diverse factors, from a person's neurophysiology to personal experience [23]. At the same time, Stephen Morse warns that that colorful images of the brain such as those produced by functional magnetic resonance imaging (fMRI) might blind people to the fundamental legal assumption that ‘people are conscious, intentional and potentially rational agents’ and therefore responsible for their actions. He cautions about the use of neuroscientific evidence either in assessing responsibility or in determining punishment for criminals acts [24].
Recent fMRI studies demonstrate the possibility of obtaining measurements of biological correlates of complex human processes such as existential thought and decision-making [25], moral and non-moral social judgment [26,27], love and altruism [28], personality [29], and human competition [30]. Do these studies demonstrate a definitive neural basis of morality or consciousness? Certainly not. Rather, they emphasize the complex and closely interrelated mechanisms that underlie emotion, values and thought. Research findings that identify physiological links between functional genetic polymorphisms and information processing through imaging genomics further highlight the complexity of and close links between thought and emotion [31,32].
In Buddhism, scientific knowledge about the nature of the self is said to be embraced flexibly [33] and teachings modified accordingly. When queried about ethics and the neuroscience of the self at the first SfN ‘Dialogues’ event, the Dalai Lama defined ethics in the context of the pursuit of experience and human happiness. When asked whether neuroscience – especially when it touches upon personhood and personal thought – should remain untouched by scientific investigation, he responded that with respect for life and purity of motivation, moral acceptability is boundless. Indeed, whereas some consider the pursuit of knowledge about human nature and the mind praiseworthy, others can consider the intimacy of the human mind to be outside the province of science. Beyond purity of motivation as a justification, such consternation about forbidden knowledge might be allayed with openness to understanding the limits of research [34] – what research can deliver, and what it simply cannot. Not surprisingly, in a study begun in 2003, neuroscience professionals and other stakeholders were found to be most concerned about the perceived non-clinical applications of neurotechnology, and they called for greater attention to ethical ramifications of research on the part of individual investigators to prevent misunderstandings and misuse of scientific results [35]. Examples of implied responsibilities include experimental reproducibility of potentially complex data, civic involvement in promoting public understanding of neuroscience findings, and leadership in democratic debate regarding the appropriate use of research results [36] – considerations that factor into the role of neuroscience in social policy.
Social policy
For a relatively young discipline, a surprisingly large number of neuroethics topics are the focus of social policy issues. Three that have garnered substantial attention in the peer-reviewed literature and the popular press are (i) brain imaging for lie detection, (ii) cognitive enhancement, and (ii) direct-to-consumer marketing of brain products and services.
Lie detection
Despite the disputed uses of polygraphy and other methods for extracting information from humans, pursuing a method for detecting deception has been an enduring focus of scientific endeavor in the neurobehavioral sciences [37]. Whether this interest is driven by human curiosity, an urge to find a telltale sign of a lie, or the perceived practical usefulness of such results to society is unclear. It is certainly not being pursued for ease of use, given the many layers of difficulty in capturing data with real-world validity [38]. However, it is clear that as new neurotechnologies emerge, their application to this domain, appropriate or not, is likely to be rapid. For example, in one recent paper using fMRI, F. Andrew Kozel and colleagues reported >90% accuracy in identifying neural patterns in individuals that they attribute to lying [39]. In the same paper, the authors disclose licensing of the technology by Cephos Corporation (http://www.cephoscorp.com/). The policy questions are numerous. Even if a scan could accurately determine that a person is actually lying, providing the answer to the inevitable ‘what’ question (i.e. what is the person lying about) will be far more elusive. In this case, usefulness is limited, at best. At worst, the risk of false positives is enormous, because even a low false-positive rate could have important consequences for an individual accused of criminal intent. Other related policy issues also surface: will accused individuals be compelled or coerced to undergo scans? Will victims be equally compelled to be tested [40]? To transfer good science into the real-world setting before these ethical issues are adequately addressed raises formidable risks for the credibility of the science.
Cognitive enhancement
If society worries about whether testimony is truthful, it must also worry about the authenticity of behavior. No other neuroscience topic challenges the question of authenticity more than that of cognitive enhancement. Whether the capacity for memory and attention is augmented using drugs [e.g. that modulate AMPA receptors to facilitate depolarization, thereby increasing levels of cAMP-response-element binding protein (CREB), which in turn activates genes to produce proteins that strengthen the synapse [41], or memories are suppressed using β blockers [42], the goal is roughly the same: pharmacological control over neurocognitive function [43]. Such intervention can have a measurable impact in enabling an individual to interact more effectively in the environment in ways that might or might not be achieved by hard work, good work habits, and the sheer dedication of the human mind to a problem. Little if any controversy exists over attempts to ameliorate frank pathology. The ethical and policy questions are primarily concerned with subclinical or nonclinical uses of pharmacological intervention [44]. With implantable neural devices on the horizon further raising ethical considerations (e.g. Ref. [45], http://roboethics.Stanford.edu), such discussions have clearly only just begun.
Direct-to-consumer advertising (DTCA)
At the intersection of personal autonomy and the corporate world lies the relatively new phenomenon of directly marketing products and health care services to consumers. The billion dollar nutritional supplement market for memory is one example. Advertisements encourage consumers to request prescription drugs such as Ritalin and Modafinil from their physicians. A comparative analysis of internet-based advertising for ‘neuroproducts’ – pharmaceuticals, imaging and natural products – shows that existing mechanisms for monitoring the promotion of prescription drugs are being put to the test and, as technology develops, the information that regulatory bodies will need to be able to oversee will only further challenge their already fragile oversight mechanisms [46].
Clinical practice
Given the rapid pace of neuroscience innovation and expanded applications both within and outside of academic medicine [47], researchers must partner more closely than ever with physicians in many spheres of immediate importance. Some examples are:
Technology transfer
It will be important to ensure that health benefits outweigh risks, and that fair access to new or re-emerging technologies (e.g. transcranial magnetic stimulation, TMS [48,49], or electroconvulsive therapy, ECT) are balanced against the pull from society for new innovation and the push from academia for technology transfer.
Incidental findings
Guidelines are needed for managing abnormalities of potential clinical significance that are detected unexpectedly in research [50].
Regenerative medicine
There should be critical evaluation of the promises, risks and implications of molecular and transplant medicine, and functional imaging, in regenerative medicine (J. Illes, ‘Flowers for Algernon and other ethical challenges in stem cells and neuroscience', speaking at Stanford University, 20 January 2006).
Prediction
Appropriate cautions should be applied in the use of neuroscience methods such as brain and gene mapping when predicting, for example, diseases of the CNS in the absence of treatment [51], the potential for recovery from diminished states of consciousness [52], and poor developmental outcome in children [53].
Self-referred brain imaging
It will be important to ensure that there is quality control and good consumer education in the growing industry of functional brainimaging services that use MRI, single-photon emission computed tomography (SPECT) and other neuroimaging technologies [54,55].
Public discourse and training
The gate at Pearson Airport in Toronto, Canada that services passengers en route to Reagan Airport in Washington DC,USA,has special security. After passing the usual screening, each person is frisked and bags undergo an extra hand-checking. Standing in a long line awaiting this procedure, one of us (J.I.) overheard one passenger say to another, who seemed to be even more annoyed than the first: ‘This is the gate where you get your brain scanned.’
This narrative highlights the importance of accurate dissemination of information from the scientific world to the public, most often with the media as the intermediary. Neuroscience research garners substantial public attention, and news coverage is an important channel in the transfer of neuroscience knowledge to the public. The history of neuroscience shows that popular depiction of science in print media has an important role in shaping ethics debates and public acceptance of biomedical innovation [56]. At the same time, communicating science to the public raises a host of ethical issues [57,58].
A recent study examined press coverage of frontier neurotechnology [e.g. electroencephalograms (EEG), positron-emission tomography (PET), neurostimulation and neurogenetic testing] for ethical content and reporting practices in 1995–2004 [46]. With the exception of neurogenetic testing, coverage in major newspapers in the USA and UK was overwhelmingly optimistic. However, articles on neurogenetic testing featured three times as many ethical, legal and social issues (e.g. discrimination, privacy and confidentiality) than any of the other neurotechnologies. Combined with the finding that technical capabilities and limitations of the technologies go largely unnoted, there is a clear imperative for better balance in neuroscience reporting and improved public understanding.
Beyond the importance of more effective communication between neuroscientists, the media and the public, on both a local and an international scale [59], neuroethics scholars and neuroscientists who have specific neuroethics interests have an important role in teaching ethical awareness to young trainees, and in the application of critical ethical thinking to the scientific process. This is essential not only to the longevity of neuroethics but to the vitality that newlyminted neuroethicists will bring to ethics in neuroscience.
Concluding remarks
In 1597, Sir Francis Bacon wrote ‘Knowledge is power’ (‘Ipsa scientia potestas est’) [60]. The potential of new neuroscience knowledge is almost beyond comprehension and we have only sampled it here. With this knowledge comes the responsibility to prevent its misuse and abuse. This effort begins with continued, interactive cooperation with others across disciplines to articulate and examine assumptions that underlie the professional and cultural values inherent in neuroscience. Understanding the historical foundations of ethics in neuroscience, its connections to other areas of modern science and bioethics, and the vital role that neuroethics must have, are key to illuminating its future.
Acknowledgements
Supported by NIH/NINDS RO1#045831 (J.I.). We thank Dr Eric Kandel for his contribution. We also wish to acknowledge TINS reviewers, Dr Jen McCormick and Dr Eric Racine for helpful comments, and Katie Alton for graphic design.
References
- 1.Zimmer C. Soul Made Flesh: The Discovery of the Brain – and How it Changed the World. Free Press; 2004. [Google Scholar]
- 2.Potter VR. Bioethics: Bridge to the Future. Prentice-Hall; 1971. [Google Scholar]
- 3.Bird SJ. Neuroethics. In: Mitcham C, editor. Encyclopedia of Science, Technology, and Ethics. Macmillan Reference; 2005. pp. 1310–1316. [Google Scholar]
- 4.Pontius AA. Neuroethics vs neurophysiologically and neuropsychologically uninformed influences in child-rearing and education. Psychol. Rep. 1993;72:451–458. doi: 10.2466/pr0.1993.72.2.451. [DOI] [PubMed] [Google Scholar]
- 5.Farah MJ, Wolpe PR. Neuroethics: toward broader discussion. Hastings Cent. Rep. 2004;34:35–45. [Google Scholar]
- 6.Roskies A. Neuroethics for the new millennium. Neuron. 2002;35:21–23. doi: 10.1016/s0896-6273(02)00763-8. [DOI] [PubMed] [Google Scholar]
- 7.Illes J, et al. From neuroimaging to neuroethics. Nat. Neurosci. 2003;6:205. doi: 10.1038/nn0303-205. [DOI] [PubMed] [Google Scholar]
- 8.Keveles DJ. In the Name of Eugenics: Genetics and the Uses of Human Heredity. Alfred Knopf; 1985. [Google Scholar]
- 9.Muller-Hill B. Murderous Science: Elimination by Scientific Selection of Jews, Gypsies, and Others, Germany 1933–1945. Oxford University Press; 1988. [Google Scholar]
- 10.Lifton R. The Nazi Doctors: Medical Killings and the Psychology of Genocide. Basic Books; 2000. [Google Scholar]
- 11.Valenstein ES. Great and Desperate Cures: The Rise and Decline of Pyschosurgery and Other Radical Treatments for Mental Illness. Basic Books; 1986. [Google Scholar]
- 12.Mashour GA, et al. Psychosurgery: past, present, and future. Brain Res. Rev. 2005;48:409–419. doi: 10.1016/j.brainresrev.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Chorover SL. From Genesis to Genocide. MIT Press; 1979. [Google Scholar]
- 14.Valenstein ES, editor. The Psychosurgery Debate. W.H. Freeman; 1980. [Google Scholar]
- 15.Gaylin W, et al. Violence and the Politics of Research. Plenum Press; 1981. [Google Scholar]
- 16.Congress of the US, Office of Technology Assessment Impacts of Neuroscience. 1984 http://www.wws.princeton.edu/ota/ns20/year_f.html.
- 17.Vincent J-D. In Proceedings. Third Session. International Bioethics Committee of UNESCO; 1995. Ethics and neurosciences; pp. 1–8. [Google Scholar]
- 18.Jackson FLC. Tuskegee Experiment. In: Mitcham C, editor. Encyclopedia of Science, Technology, and Ethics. Macmillan Reference; 2005. pp. 1986–1988. [Google Scholar]
- 19.National Commission for the Protection of Human Subjects . The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research. Government Printing Office; 1978. [Google Scholar]
- 20.Pfaff DW, editor. Ethical Questions in Brain and Behavior: Problems and Opportunities. Springer-Verlag; 1983. [Google Scholar]
- 21.Marcus S, editor. Neuroethics: Mapping the Field. The Dana Foundation Press; 2002. [Google Scholar]
- 22.Damasio AR. The neural basis of social behavior: ethical implications. In: Marcus SJ, editor. Neuroethics: Mapping the Field. The Dana Foundation Press; 2002. pp. 14–19. [Google Scholar]
- 23.Schaffner KF. Neuroethics: reductionism, emergence, and decision-making capacities. In: Marcus SJ, editor. Neuroethics: Mapping the Field. The Dana Foundation Press; 2002. pp. 27–33. [Google Scholar]
- 24.Morse SJ. Moral and legal responsibility and the new neuroscience. In: Illes J, editor. Neuroethics: Defining the Issues in Theory, Practice and Policy. Oxford University Press; 2006. pp. 33–50. [Google Scholar]
- 25.Greene JD, et al. An fMRI investigation of emotional engagement in moral judgment. Science. 2001;293:2105–2108. doi: 10.1126/science.1062872. [DOI] [PubMed] [Google Scholar]
- 26.Moll J, et al. The neural correlates of moral sensitivity: a functional magnetic resonance imaging investigation of basic and moral emotions. J. Neurosci. 2002;22:2730–2736. doi: 10.1523/JNEUROSCI.22-07-02730.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moll J, et al. Functional networks in emotional and nonmoral social judgments. NeuroImage. 2002;16:696–703. doi: 10.1006/nimg.2002.1118. [DOI] [PubMed] [Google Scholar]
- 28.Bartels A, Zeki S. The neural correlates of maternal and romantic love. NeuroImage. 2004;21:1155–1166. doi: 10.1016/j.neuroimage.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Canli T, et al. Amygdala response to happy faces as a function of extraversion. Science. 2002;296:2191. doi: 10.1126/science.1068749. [DOI] [PubMed] [Google Scholar]
- 30.Decety J, et al. The neural bases of cooperation and competition: An fMRI investigation. NeuroImage. 2004;23:744–751. doi: 10.1016/j.neuroimage.2004.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hariri AR, Weinberger DR. Imaging genomics. Br. Med. Bull. 2003;65:259–270. doi: 10.1093/bmb/65.1.259. [DOI] [PubMed] [Google Scholar]
- 32.Meyer-Lindenberg A, et al. Neural mechanisms of genetic risk for impulsivity and violence in humans. Proc. Natl. Acad. Sci. U. S. A. 2006;103:6269–6274. doi: 10.1073/pnas.0511311103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ricard M, Thuan TX. The Quantum and the Lotus: A Journey to the Frontiers Where Science and Buddhism Meet Three Rivers. Three Rivers Press; 2001. [Google Scholar]
- 34.Illes J, Racine E. Imaging or imagining? A neuroethics challenge informed by genetics. Am. J. Bioeth. 2005;5:5–18. doi: 10.1080/15265160590923358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Illes J, et al. ELSI issues in advanced neuroimaging. Am. J. Bioeth. 2006;6:W24–W31. doi: 10.1080/15265160500506274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Illes J, et al. A picture is worth 1000 words, but which 1000? In: Illes J, editor. Neuroethics: Defining the Issues in Theory, Practice, Policy. Oxford University Press; 2006. pp. 149–168. [Google Scholar]
- 37.Cacioppo JT, Berntson GG. Social Neuroscience. Psychology Press; 2005. [Google Scholar]
- 38.Illes J. Cerebrum: Special Issue on Neuroethics. The Dana Foundation Press; 2004. A fish story: brain maps, lie detection and personhood; pp. 73–80. [PubMed] [Google Scholar]
- 39.Kozel FA, et al. Detecting deception using functional magnetic resonance imaging. Biol. Psychiatry. 2005;58:605–613. doi: 10.1016/j.biopsych.2005.07.040. [DOI] [PubMed] [Google Scholar]
- 40.Schacter DL, et al. Memory, consciousness and neuroimaging. Philos. Trans. R. Soc. Lond. 1998:1861–1978. doi: 10.1098/rstb.1998.0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Farah MJ, et al. Neurocognitive enhancement: what can we do and what should we do? Nat. Rev. Neurosci. 2004;5:421–425. doi: 10.1038/nrn1390. [DOI] [PubMed] [Google Scholar]
- 42.Pitman RK, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol. Biol. Psychiatry. 2002;51:189–192. doi: 10.1016/s0006-3223(01)01279-3. [DOI] [PubMed] [Google Scholar]
- 43.Chatterjee A. Cosmetic neurology: the controversy over enhancing movement, mentation, and mood. Neurology. 2004;63:968–974. doi: 10.1212/01.wnl.0000138438.88589.7c. [DOI] [PubMed] [Google Scholar]
- 44.Evers K. Perspectives on memory manipulation: Using beta-blockers to cure post-traumatic stress disorder. Camb. Q. Healthc. Ethics. doi: 10.1017/s0963180107070168. in press. [DOI] [PubMed] [Google Scholar]
- 45.Foster KR. Engineering the brain. In: Illes J, editor. Neuroethics: Defining the Issues in Theory, Practice and Policy. Oxford University Press; 2006. pp. 185–199. [Google Scholar]
- 46.Racine E, et al. Internet marketing of neuroproducts: New practices and healthcare policy challenges. Camb. Q. Healthc. Ethics. doi: 10.1017/s096318010707020x. in press. [DOI] [PubMed] [Google Scholar]
- 47.Illes J, Kirschen MP. New prospects and ethical challenges for neuroimaging within and outside the health care system. Am. J. Neuroradiol. 2003;24:1932–1934. [PMC free article] [PubMed] [Google Scholar]
- 48.Couturier JL. Efficacy of rapid-rate repetitive transcranial magnetic stimulation in the treatment of depression: a systematic review and meta-analysis. J. Psychiatry Neurosci. 2005;30:83–90. [PMC free article] [PubMed] [Google Scholar]
- 49.Fregni F, Pascual-Leone A. Repetitive transcranial magnetic stimulation for the treatment of depression. J. Psychiatry Neurosci. 2005;30:434–435. [PMC free article] [PubMed] [Google Scholar]
- 50.Illes J, et al. Incidental findings in brain imaging research. Science. 2006;311:783–784. doi: 10.1126/science.1124665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cummings JL. Treatment of Alzheimer's disease: current and future therapeutic approaches. Rev. Neurol. Dis. 2004;1:60–69. [PubMed] [Google Scholar]
- 52.Schiff ND, et al. MRI reveals large-scale network activation in minimally conscious patients. Neurology. 2005;64:514–523. doi: 10.1212/01.WNL.0000150883.10285.44. [DOI] [PubMed] [Google Scholar]
- 53.Moseley M, et al. Diffusion tensor imaging of cognitive function. Brain Cogn. 2002;50:396–413. doi: 10.1016/s0278-2626(02)00524-9. [DOI] [PubMed] [Google Scholar]
- 54.Cho MK. Conflicts of interest in magnetic resonance imaging: issues in clinical practice and research. Top. Magn. Reson. Imaging. 2002;13:73–78. doi: 10.1097/00002142-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 55.Illes J, et al. Advertising, patient decision-making, and self-referral to CT and MR imaging. Arch. Intern. Med. 2004;164:2415–2419. doi: 10.1001/archinte.164.22.2415. [DOI] [PubMed] [Google Scholar]
- 56.Diefenbach GJ, et al. Portrayal of lobotomy in the popular press: 1935–1960. J. Hist. Neurosci. 1999;8:60–69. doi: 10.1076/jhin.8.1.60.1766. [DOI] [PubMed] [Google Scholar]
- 57.Garrett JM, Bird SJ. Ethical issues in communicating science. Sci. Eng. Ethics. 2000;6:435–442. doi: 10.1007/s11948-000-0001-7. [DOI] [PubMed] [Google Scholar]
- 58.Bird SJ. Communicating scientific advice to the public. The IPTS Report 72. 2003 Accessed 12 January 2006 http://www.jrc.es/home/report/english/articles/vol72/SCI3E726.htm.
- 59.Illes J, et al. Neuroethics: International perspectives on engaging the public. Nat. Rev. Neurosci. 2005;6:977–982. doi: 10.1038/nrn1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bacon F. Meditationes Sacræ. De Hæresibus. 1597 [Google Scholar]