Abstract
Influenza virus-specific CD8+ T cells generally recognize peptides derived from conserved, internal proteins that are not subject to antibody-mediated selection pressure. Prior exposure to any one influenza A virus (H1N1) can prime for a secondary CD8+ T cell response to a serologically different influenza A virus (H3N2). The protection afforded by this recall of established CD8+ T cell memory, although limited, is not negligible. Key characteristics of primary and secondary influenza-specific host responses are probed here with recombinant viruses expressing modified nucleoprotein (NP) and acid polymerase (PA) genes. Point mutations were introduced into the epitopes derived from the NP and PA such that they no longer bound the presenting H2Db MHC class I glycoprotein, and reassortant H1N1 and H3N2 viruses were made by reverse genetics. Conventional (C57BL/6J, H2b, and Ig+/+) and Ig-/- (μMT) mice were more susceptible to challenge with the single NP [HKx31 influenza A virus (HK)-NP] and PA (HK-PA) mutants, but unlike the Ig-/- mice, Ig+/+ mice were surprisingly resistant to the HK-NP/-PA double mutant. This virus was found to promote an enhanced IgG response resulting, perhaps, from the delayed elimination of antigen-presenting cells. Antigen persistence also could explain the increase in size of the minor KbPB1703 CD8+ T cell population in mice infected with the mutant viruses. The extent of such compensation was always partial, giving the impression that any virus-specific CD8+ T cell response operates within constrained limits. It seems that the relationship between protective humoral and cellular immunity is neither simple nor readily predicted.
The CD8+ T cell response of C57BL/6J (B6, H2b) mice to the influenza A viruses is directed against at least six viral peptides (1–3). The most prominent (2, 4) are derived from the viral nucleoprotein (NP366–374) and acid polymerase (PA224–236), both of which are presented by the H2Db MHC class I glycoprotein. Both epitopes exhibit the (XXXXNXXM/L/I) H2Db binding motif (5). The asparagine in position five binds to a pocket within the MHC groove, acting as the primary anchor residue (6), and mutations in this position result in decreased peptide affinity for H2Db (7, 8).
Mice infected intranasally (i.n.) with the H3N2 HKx31 influenza A virus (HK) virus or i.p. with the H1N1 A/PR/8/34 (PR) virus develop primary responses to the DbNP366 and DbPA224 epitopes that look to be broadly comparable. However, although the sizes of the resultant CD8+ memory T cell populations are also equivalent for DbNP366 and DbPA224, the recall response in H1N1-primed mice challenged i.n. with the H3N2 virus is ≈10 times greater in magnitude for DbNP366 than for DbPA224 (2, 9, 10). Other, earlier experiments indicate that CD8+ T cell-mediated virus clearance in this influenza model is mediated principally by cytotoxic T lymphocytes operating via either the perforin/granzyme or Fas/Fas ligand pathways (11). Assaying for in vitro cytotoxic T lymphocyte activity established that, although activated CD8+ DbNP366+ and CD8+DbPA224+ T cells both mediate potent lysis of peptide-pulsed, syngeneic targets, only the CD8+ DbNP366+ set shows evidence of strong cytotoxicity when assayed on virus-infected cells (2). This implies that influenza infection alone does not induce substantial expression of the DbPA224 epitope and suggests the possibility that much (if not all) of the response to DbPA224 may be induced as a consequence of protein reprocessing (12–14) in professional antigen-presenting cells. If this is the case, are the CD8+DbPA224+ T cells beneficial, or do they function to diminish the protective virus-specific T cell response by selectively eliminating antigen-presenting dendritic cells while ignoring virus-infected lung epithelium? Such “red-herring” responses are a formal possibility that could, for example, be a problem for experimental cancer therapies based on dendritic cell cross-presentation of peptides processed from apoptosed tumor cells (15, 16).
On the other hand, vaccination strategies directed at priming the DbNP366-specific set have generally given somewhat disappointing levels of protection (17–19). Clearly it is important from a vaccine viewpoint to establish just what constitutes a protective epitope. The present experiments used both HK and PR influenza viruses that had been modified (20–22) by site-directed mutagenesis to generate variant NP366–374 and/or PA224–236 peptides that no longer bind to H2Db. The studies focused principally on patterns of virus clearance and survival and on the nature of the CD8+ T cell-response profiles after primary and secondary challenge (23) with these disrupted viruses.
Materials and Methods
Mice and Infection. Female B6 and BALB/c mice were purchased from The Jackson Laboratory, and the congenic Ig-/- (μMT) mice (24) were bred at Charles River Breeding Laboratories. All mice were held under specific pathogen-free conditions at St. Jude Children's Research Hospital. Naive mice, or mice that had been primed 4–8 weeks earlier by i.p. inoculation with 108 50% egg infective dose (eID50) of the appropriate PR-mutant viruses (23), were anesthetized by i.p. injection of avertin (2,2,2-tribromoethanol) before i.n. challenge (30 μl) with graded doses of virus (25).
Generation of Recombinant Viruses. The recombinant viruses were produced by using an established eight-plasmid reverse-genetics system (20). The PR plasmids have been described (20), and the HK variants were generated from six of the PR plasmids and hemagglutinin and neuraminidase genes cloned from the A/ Aichi/2/68, H3N2 virus into pHW2000. Single amino acid mutations were introduced into the plasmids encoding the PR NP and PA genes by using PCR. Briefly, segment-specific fragments were amplified by using the universal primers described by Hoffman et al. (22) and internal primers designed with altered nucleotide sequences and terminal BsmB1 sites (New England Biolabs). The primer sequences are available on request. These mutations resulted in the position-five asparagine of both epitopes being substituted for glutamine. Purified PCR products were cleaved with BsmB1 and ligated into pHW2000. Individual mutations from rescued viruses were confirmed by sequencing as described (22). The viruses with modified NP and PA segments are referred to as PR-NP and HK-NP and PR-PA and HK-PA, respectively. The double mutants are identified as PR-NP/-PA and HK-NP/-PA. The reconstituted wild-type (wt) viruses were designated PR-RG and HK-RG.
In Vitro Growth Kinetics, Tissue Sampling, and Viral Titration. The growth kinetics of wt and mutant viruses were determined by Madin–Darby canine kidney (MDCK) cell culture. Near confluent 25-cm2 monolayers of MDCK cells were infected with 1 ml of virus at a multiplicity of infection of 0.01 for 1 h at 37°C. Cells were washed with PBS, 5 ml of MEM containing 1 mg/ml L-1-tosylamido-2-phenylethyl chloromethyl ketone-treated trypsin (Worthington) was added, and cultures were incubated at 37°C, 5% CO2. Viral titers were determined at 12-h intervals by plaque assay on MDCK cells. At the time of sampling, infected mice were anaesthetized and exsanguinated by section of the axillary artery. The spleens were removed, and inflammatory cell populations were recovered from the infected respiratory tract (26) by bronchoalveolar lavage (BAL). The lungs then were taken for fixation and subsequent histopathology analysis or fresh-frozen for later virus titration. Lung homogenates were titrated in embryonated hen's eggs, and virus titers are expressed as log10 eID50 per lung. To determine influenza-specific antibody responses after infection, mice were warmed with an infrared lamp, and the lateral tail vein was cut. Approximately 100 μl of blood was collected, and serum was separated by centrifugation.
Flow-Cytometric Analysis. The kinetics and magnitude of the virus-specific CD8+ T cell responses were analyzed by flow cytometry. The spleens were disrupted and enriched for CD8+ T cells (26) by incubation with mAbs to CD4 (GK1.5) and MHC class II glycoprotein (M5/114.15.2), followed by anti-rat and anti-mouse IgG-coated magnetic beads (Dynal, Oslo). Lymphocytes were isolated from the pneumonic lung by BAL, and macrophages were removed by incubating on plastic for 1 h at 37°C. The DbNP366 and DbPA224 tetramers (27) were made by complexing H2Db with the immunogenic NP366 (ASNEN-METM) (4) or PA224 (SSLENFRAYV) (2) peptides or H2Kb with the polymerase 1 (PB1703, SSYRRVPGI) peptide (3). Lymphocytes were incubated for 60 min at room temperature with the phycoerythrin-conjugated tetramers in PBS/BSA/ azide (23) followed by staining with anti-CD8α-PerCPCy5.5 (PharMingen). All data were acquired on a Becton Dickinson FACScan and then analyzed by using CELLQUEST software (Becton Dickinson Immunocytometry Systems).
Measuring the IgG Response. Microtiter plates (Nalge Nunc International, Rochester, NY) were coated overnight at 4°C with purified whole influenza HKx31, A/Aichi/68 (H3N2) virus (Charles River Breeding Laboratories) in PBS. The virus was diluted 1/10 in lysis buffer (0.05 M Tris, pH 7.5/0.5% Triton X-100/0.6 M KCl) in PBS, adjusted to 10 μg/ml and aliquoted at 50 μl per well. The plates were washed with 0.05% Tween 20 (Sigma) and blocked with 1% BSA in PBS. After 1 h at room temperature, the plates were washed again, and diluted serum samples were added and incubated for 2 h at room temperature. After washing, influenza-specific IgG was detected (1 h at room temperature) with a goat anti-mouse IgG alkaline-phosphatase conjugate (Southern Biotechnology Associates) diluted 1:1,000 in 1% BSA. After three final washes substrate (p-nitrophenyl phosphate, Sigma) was added, and plates were incubated for 60 min at room temperature for color development. ODs were determined at 405 nm in an ELISA reader (Molecular Devices). Titers were presented as the highest dilution that yielded an OD three times higher than that for a 1:100 dilution of preimmune serum.
Results
The experimental strategy used in most of these experiments was to challenge age-matched, naive, or previously primed PR-immune B6 mice i.n. with the homologous HK mutants (23). The antibody responses to the PR and HK viruses are distinct to the extent that there is no evidence of cross-neutralization either in vitro or in vivo (28). The interval between the two infections was at least 4–8 weeks to allow the establishment of stable T cell memory. Because the primary focus was to analyze how disrupting the response to one epitope might influence the response to another, the first step was to establish a safe virus dose (Fig. 1) such that mice would survive to develop effective immunity. The viruses were not first adapted by serial passage through mice, a step that is commonly followed with influenza A viruses that are freshly isolated from nature, because we did not wish to introduce further variables. As it turned out (Fig. 1), the dose of the HK viruses that we used for i.n. challenge was what we normally employ with the standard laboratory strain of the HK virus (2, 3, 23).
Fig. 1.
The in vitro growth characteristics (A) and profiles of weight loss (B) and survival (C–F) are shown for the HK-RG (triangles), HK-NP (squares), HK-PA (diamonds), and HK-NP/-PA (circles) viruses. (A) Madin–Darby canine cells were infected with a multiplicity of infection of 0.01, and viral titers from culture supernatants were measured by plaque assay at various time points after infection. (B) Groups of five B6 mice were infected i.n. with 106.3 eID50 of the wt and mutant viruses and weighed at daily intervals together with uninfected controls (inverted triangles). The termination of the data set on day 7 reflects that evidence of severe morbidity was apparent in the groups given the mutant viruses. Survival profiles are shown for B6 (C and D), BALB/c (E), and μMT (F) mice infected i.n. with 106.0 (C and E) or 105.0 (D and F) eID50 of the HK-variants.
Susceptibility, Virus Growth, and Lung Damage. The in vitro growth curves were identical for the reconstituted viruses, and the results for the HK variants are shown in Fig. 1 A. Naive B6 mice infected i.n. with 106.3 eID50 of the HK viruses showed a pattern of progressive weight loss from 24 h after exposure and evidence of substantial mortality from day 6 in every group (Fig. 1B). Naive B6 mice survived i.n. challenge with 106.0 (Fig. 1C) or 105.0 (Fig. 1D) eID50 of HK-RG, although some still succumbed after exposure to the mutants. As would be expected, these variants that were engineered to disrupt only the NP and PA peptides that bind H2Db did not cause enhanced mortality (relative to wt) in BALB/c (H2d) mice (Fig. 1E). Furthermore, mutating the NP366 and PA224 epitopes did not significantly modify the percentage of CD8+ T cells specific for the H2KdNP147 epitope detected in the BALB/c mice (data not shown) by using intracellular cytokine staining (2).
What was surprising was that the B6 mice seemed more likely to succumb after i.n. challenge with the HK-NP or HK-PA viruses than with the HK-NP/-PA double mutant (Fig. 1C). Early experiments with MHC class I-deficient β2-microglobulin (β2m)-/- mice showed that, although they were much more susceptible than β2m+/+ controls to challenge with HK, this influenza A virus can be cleared more slowly by a CD4+ T cell-dependent process. Later analysis with bone marrow radiation chimeras established that the CD4+ T cell-mediated protective effect operated via the provision of T help for the virus-specific B cell/antibody response (29–31). We thus asked whether μMT mice that make no antibody (24) but are able to generate both CD4+ and CD8+ effector T cells (31–33) show the same susceptibility profile as B6 mice. Intranasal infection of μMT mice with 105.0 eID50 of the HK-NP, HK-PA, or HK-NP/-PA viruses led to increased mortality when compared with the HK-RG virus (Fig. 1F). The highest mortality in μMT mice was found for the HK-NP and HK-NP/-PA mutants. A further experiment with H2I-Ab-/- (34) mice that lack both CD4+ T cells and a class-switched Ig response also showed a profile of greatest susceptibility to HK-NP/-PA (data not shown).
The HK-RG and mutant viruses were cleared progressively from the lungs of mice given 105.0 eID50, with the HK-NP variant still being recovered from three of five that were sampled on day 10 (Fig. 2). Lungs were taken for histopathology on days 5 and 10 (five per group) after i.n. infection of naive mice with 105.2 eID50 of the HK variants. The findings for both time points indicated that the severity of lung parenchymal damage was on the order of HK-NP > HK-PA > HK-NP/-PA > HK-RG. By this and other criteria examined (data not shown), the mice infected with the HK-RG virus showed evidence of less severe lung pathology.
Fig. 2.
Naive mice were infected i.n. with 105 eID50 of the HK-RG (open bars), HK-NP (filled bars), HK-PA (striped bars), or HK-NP/-PA (diamond bars) viruses. Lungs were sampled on days 3, 5, 7, 8, and 10, and then after infection they were frozen (-70°C) and later homogenized for virus titration by allantoic inoculation in embryonated hen's eggs. Virus titers are expressed as log10 eID50 per lung.
Consequences for the Virus-Specific CD8+ T Cell Response. Analysis of splenocytes isolated from naive mice 10 days after infection with the HK variants (105 eID50) demonstrated that disruption of the antigenic epitope led to the loss of the cognate virus-specific CD8+ T cell response measured by tetramer staining (data not shown). The results of primary infection experiments, however, were somewhat variable, thus the data set presented here concentrates on the much larger recall response.
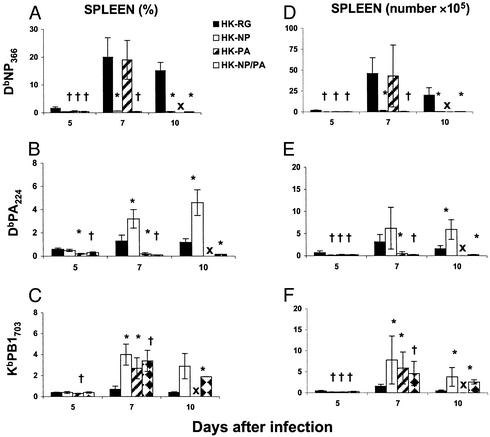
Mice primed with the PR mutants were infected i.n. with the homologous HK-viruses (106.3 eID50) and both the percentage values and the cell counts for epitope-specific CD8+ T cells in the spleens were analyzed at various time points after challenge. When compared with HK-RG infection, the DbNP366-specific response was essentially absent from mice on days 7 and 10 after infection with HK-NP (P < 0.05) or HK-NP/-PA (day 7, P < 0.01; day 10, P < 0.05) mutants (Fig. 3 A and D). A similar result was observed for the DbPA224-specific response after challenge with HK-PA (Fig. 3 B and E), although by day 10 the HK-PA-challenged mice had succumbed to infection. Interestingly, there was a significant enhancement of the DbPA224-specific response on days 7 and 10 in mice that were challenged with the HK-NP mutant (Fig. 3 B and E, P < 0.05). Furthermore, the response to KbPB1703 was enhanced significantly from day 7 in the groups that were primed (PR i.p.) and challenged with the NP and PA single (P < 0.05) and double (P < 0.01) mutants (Fig. 3 C and F). The same trends were seen in pooled BAL samples (data not shown).
Fig. 3.
Mice primed i.p. 8 weeks previously with 108 eID50 of the PR-RG and mutant viruses were challenged i.n. with 106.3 eID50 of the homologous HK variants. At various time points after infection, the splenic CD8+ T cell response was measured by staining with the DbNP366 (A and D), DbPA224 (B and E), and KbPB1703 (C and F) tetramers. The results are expressed as the percentage of cells staining (A–C) and the numbers of epitope-specific cells (D–F) that were calculated from the percentage values and the total cell counts (data not shown). The results are expressed as mean ± SD, and significant differences from the HK-RG are shown as * (P < 0.05) and † (P < 0.01). X denotes 100% death.
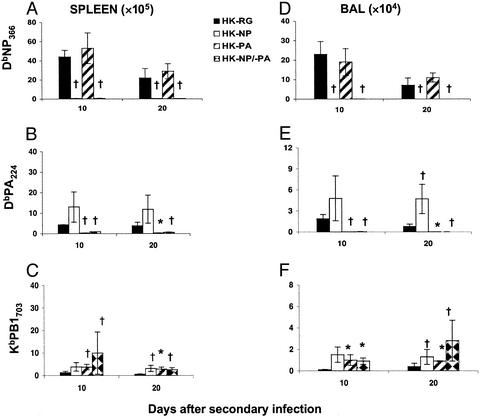
The prime-and-challenge study was repeated, giving a much lower i.n. dose (105.0 eID50) to minimize mortality (Fig. 4). Again, the response to KbPB1703 measured as epitope-specific CD8+ T cell numbers was increased significantly in both the spleen and BAL (Fig. 4 C and F) on day 10 in the mice that were infected with the HK-PA and HK-NP/PA viruses and on day 20 in those given all three mutants. Such enhancement was much less consistent for the DbPA224-specific response and was statistically significant for only the day 20 BAL population in mice that were immunized and challenged with the NP variants (Fig. 4 B and E). None of these prime/boost experiments showed any pattern of significant augmentation for the DbNP366-specific response in mice infected with the PR-PA and HK-PA variants (Figs. 3 A and D and 4 A and D and data not shown).
Fig. 4.
Mice previously primed with PR-RG and mutant viruses were challenged i.n. with 105.0 eID50 of the homologous viruses. The virus-specific CD8+ T cell counts (see Fig. 3 legend) were measured for the spleen (A–C) and BAL (D–F) populations at various time points after challenge. The results are expressed as mean ± SD, and significant differences from the HK-RG are shown as * (P < 0.05) and † (P < 0.01).
The susceptibility profiles shown in Fig. 1C would suggest that a compensatory response to KbPB1703 is not sufficient to protect mice after primary exposure to the HK-NP and HK-PA viruses. Similar trends were seen after secondary challenge (data not shown). In a parallel virus isolation study with the experiment shown in Fig. 3, virus was recovered on day 7 from the lungs of two of four and three of three of the homologous PR-mutant-primed mice challenged with HK-NP and HK-PA, respectively, whereas the HK-RG and HK-NP/-PA infections had been cleared by this time point. However, the enhanced survival of the HK-NP/-PA group cannot be attributed solely to an augmented KbPB1703 response, because the μMT mice were fully susceptible to infection with this virus (Fig. 1F).
Recovery and the Antibody Response. The fact that conventional Ig+/+ mice are relatively protected against infection with the HK-NP/-PA virus (Fig. 1 C and D), whereas this is not the case for μMT mice (Fig. 1F), suggests a possible role for antibody. The influenza-specific IgG reponse was thus measured in naive Ig+/+ mice infected i.n. with the HK-mutant viruses (Fig. 5). When compared with the consequences of infection with the HK-RG, HK-NP, and HK-PA viruses (Fig. 5), it was obvious that the HK-NP/-PA double mutant induced a significantly higher (P < 0.01) antibody response on day 7 (Fig. 5A). This same trend was also observed on days 6 (Fig. 5B) and 9 (Fig. 5C) after infection but was not statistically significant.
Fig. 5.
Groups of seven naive B6 mice were infected i.n. with 106.0 eID50 of the HK-RG (open bars), HK-NP (filled bars), HK-PA (striped bars), or HK-NP/-PA (diamond bars), and virus-specific IgG titers were determined by ELISA for serum samples taken on days 6 (A), 7 (B), and 9 (C) after infection. Titers are presented as the highest dilution that yielded an OD three times greater than that for a 1:100 dilution of preimmune sera. The results are expressed as mean ± SD, and significant differences from the HK-RG are shown as * (P < 0.01). The histograms are labeled as described in the Fig. 2 legend.
Discussion
Evidence of a compensatory response to the “minor” KbPB1703 epitope (3) can be detected in mice given viruses with disrupted NP366 or PA224 peptides. However, even with the magnifying effect associated with the recall of immunity in mice primed and boosted with PR and HK variants that share the same defect, the numbers of CD8+ KbPB1703+ T cells never increase to levels that are in any way comparable to the size of the total epitope-specific CD8+ T cell response induced by unmanipulated (PR-RG and HK-RG) viruses. This profile of “limited compensation” was also seen for the CD8+DbPA224+ response in PR-NP-immune mice after a high-dose HK-NP challenge. Thus, although removing the predominant effector population might be expected to both delay the elimination of virus-infected antigen-presenting cells and enhance the possibility that new antigen-presenting cells could continue to enter the pool of potential stimulator cells, these “minor” T cell populations are not able to sustain levels of in vivo clonal expansion equivalent to those associated with the “major” DbNP366-specific response (35). The results overall are compatible with the general view that any virus-specific CD8+ T cell response has an inherent limit that is modified only partially by eliminating other sets of effector T cells.
It is very clear from these (and our unpublished) experiments that the absence of either a functional DbNP366 or DbPA224 epitope both delays virus clearance and increases morbidity in B6 (H2b) but not in BALB/c (H2d) mice. The NP366 effect was expected, because mice transgenic for a DbNP366-specific T cell receptor generate mutant viruses that are ultimately lethal in the absence of any compensatory T cell- or antibody-mediated response (8). Activated CD8+DbNP366+ effectors are highly lytic for influenza virus-infected targets (25), and protection in vivo (36, 37) is thought to reflect perforin or Fas-mediated mechanisms that require epitope-specific recognition of influenza virus-infected respiratory epithelial cells (11). By contrast, the minimal level of cytotoxicity found for virus-infected, syngeneic cell lines exposed to CD8+DbPA224-specific effectors had raised doubts concerning the in vivo role of these T cells (2).
Even so, CD8+DbPA224+ effector and memory T cells make higher levels of both IFN-γ and tumor necrosis factor α than the corresponding CD8+DbNP366+ sets after in vitro stimulation with cognate peptides (3). Recent experiments with extremely virulent H5N1 influenza viruses established that enhanced susceptibility is associated with viral resistance to protective mechanisms associated with IFN-γ and tumor necrosis factor α (38), whereas earlier studies showed that neutralizing IFN-γ by in vivo mAb treatment delayed clearance of the HK virus from CD8+ T cell-deficient β2m-/- mice (39). This protective effect was not seen in β2m+/+ mice with a disrupted IFN-γ receptor (40). The key question in the present context is whether DbPA224 is expressed on the respiratory epithelial cells that are producing infectious influenza virus. Although early experiments seemed to exclude the possibility that influenza-specific CD8+ T cells can function in some “bystander” mode (41, 42) to limit infection in cells that are not expressing the appropriate epitope, this may need to be looked at again with newer assay systems.
Given that B6 mice show enhanced susceptibility to infection with the HK-NP and HK-PA variants, reflecting delayed clearance relative to the unmodified HK-RG virus, it was surprising that the HK-NP/-PA double mutant was more similar to the wt in both respects. The HK-NP/-PA virus grew as well as the other variants in cell culture, was found at equivalent titer in the lungs of mice sampled 5 days after primary or secondary i.n. challenge, caused comparable weight loss after high-dose i.n. exposure, and induced a pattern of lung pathology that was intermediate between that caused by the wt HK-RG and the mutant HK-NP and HK-PA viruses. A formal possibility is that the diminution in severity of disease associated with the HK-NP/-PA virus reflects the development of a more effective, although minor in terms of magnitude, response in the absence of the DbNP366 and DbPA224 epitopes. The CD8+ KbPB1703+ effectors mediate potent lysis of peptide-pulsed target cells, are strong IFN-γ and tumor necrosis factor α producers (3), and are found at increased prevalence in PR-NP/-PA-primed mice challenged with the HK-NP/-PA virus. The proposal that an augmented CD8+KbPB1703+ response provides better protection in the absence of the CD8+DbPA224+ and CD8+DbNP366+ effectors, however, is essentially negated by the fact that the μMT mice were highly susceptible to infection with the HK-NP/-PA virus. The μMT mice have been shown previously to make effective, influenza-specific CD4+ and CD8+ T cell responses (31, 33).
The enhanced antibody response in naive mice infected i.n. with the HK-NP/-PA double mutant is associated with greater survival than that found afer challenge with the HK-NP and HK-PA single variants. In the influenza model, neutralizing antibody provides the main mechanism for protection against reinfection of immune mice (43). Although naive μMT and CD4+ T cell-deficient mice can deal with influenza virus in the absence of antibody (33, 35, 44), CD8+ T cell-depleted mice also survive challenge with the relatively mild HK virus (45–47). A likely mechanism is that neutralizing Ig diminishes the severity of pathology by preventing the spread of virus from cell to cell (43). The effectiveness of this process will be enhanced by the destruction of infected respiratory epithelium by the CD8+ effectors (48).
A possible explanation for the greater resistance to the HK-NP/-PA (compared with HK-NP or HK-PA) challenge is that the absence of both the CD8+DbPA224+ and CD8+DbNP366+ effector sets prolongs antigen-presenting cell survival (9, 49, 50) in the lymph nodes and spleen, allowing greater CD4+ T cell and B cell stimulation. Continuing exposure to antigen would also explain the increased size of the minor CD8+KbPB1703+ population, which implies that the fine-tuning of humoral and cell-mediated immunity can lead to variable outcomes. Mice infected with the wt HK-RG virus were least susceptible and those given the HK-NP virus were most likely to succumb, whereas the HK-NP/-PA virus was of intermediate virulence in Ig+/+ (but not μMT) mice. The relationship between the protective effects of cell-mediated immunity and antibody is neither simple nor readily predicted.
Acknowledgments
We thank Gabriela Diaz and Astrid Gutierrez for excellent technical assistance. We also thank Vicki Henderson for help with the manuscript. This work was supported by U.S. Public Health Service Grants AI29579 and AI95357, an F. M. Burnet Fellowship of the Australian National Health and Medical Research Council (to P.C.D.), and the American Lebanese Syrian Associated Charities.
Abbreviations: NP, influenza nucleoprotein; PA, influenza acid polymerase; i.n., intranasal(ly); HK, HKx31 influenza A virus; PR, A/PR/8/34 influenza A virus; Db, H2Db class I MHC glycoprotein; DbNP366, DbPA224, and KbPB1703, antigenic epitopes and tetramer staining reagents bound by influenza-specific T cells; μMT, Ig-/-; eID50, 50% egg infective dose; wt, wild type; RG, reverse genetics-derived wt virus; BAL, bronchoalveolar lavage; PB1, influenza polymerase 1; β2m, β2-microglobulin.
References
- 1.Yewdell, J. W. & Bennink, J. R. (1999) Annu. Rev. Immunol. 17, 51-88. [DOI] [PubMed] [Google Scholar]
- 2.Belz, G. T., Xie, W., Altman, J. D. & Doherty, P. C. (2000) J. Virol. 74, 3486-3493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Belz, G. T., Xie, W. & Doherty, P. C. (2001) J. Immunol. 166, 4627-4633. [DOI] [PubMed] [Google Scholar]
- 4.Townsend, A. R., Rothbard, J., Gotch, F. M., Bahadur, G., Wraith, D. & McMichael, A. J. (1986) Cell 44, 959-968. [DOI] [PubMed] [Google Scholar]
- 5.Falk, K., Rotzschke, O., Stevanovic, S., Jung, G. & Rammensee, H.-G. (1991) Nature 351, 290-296. [DOI] [PubMed] [Google Scholar]
- 6.Young, A. C., Zhang, W., Sacchenttini, J. C. & Nathenson, S. G. (1994) Cell 76, 39-50. [DOI] [PubMed] [Google Scholar]
- 7.Sigal, L. J. & Wylie, D. E. (1996) Mol. Immunol. 33, 1323-1333. [DOI] [PubMed] [Google Scholar]
- 8.Price, G. E., Ou, R., Jiang, H., Huang, L. & Moskophidis, D. (2000) J. Exp. Med. 191, 1853-1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Belz, G. T., Stevenson, P. G. & Doherty, P. C. (2000) J. Immunol. 165, 2404-2409. [DOI] [PubMed] [Google Scholar]
- 10.Wiley, J. A., Hogan, R. J., Woodland, D. L. & Harmsen, A. G. (2001) J. Immunol. 167, 3293-3299. [DOI] [PubMed] [Google Scholar]
- 11.Topham, D. J., Tripp, R. A. & Doherty, P. C. (1997) J. Immunol. 159, 5197-5200. [PubMed] [Google Scholar]
- 12.Sigal, L. J. & Rock, K. L. (2000) J. Exp. Med. 192, 1143-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heath, W. R. & Carbone, F. R. (2001) Nat. Rev. Immunol. 1, 126-134. [DOI] [PubMed] [Google Scholar]
- 14.Shen, X., Wong, S. B., Buck, C. B., Zhang, J. & Siliciano, R. F. (2002) J. Immunol. 169, 4222-4229. [DOI] [PubMed] [Google Scholar]
- 15.Berard, F., Blanco, P., Davoust, J., Neidhart-Berard, E. M., Nouri-Shirazi, M., Taquet, N., Rimoldi, D., Cerottini, J. C., Banchereau, J. & Palucka, A. K. (2000) J. Exp. Med. 192, 1535-1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Banchereau, J., Schuler-Thurner, B., Palucka, A. K. & Schuler, G. (2001) Cell 106, 271-274. [DOI] [PubMed] [Google Scholar]
- 17.Andrew, M. E., Coupar, B. E., Boyle, D. B. & Ada, G. L. (1987) Scand. J. Immunol. 25, 21-28. [DOI] [PubMed] [Google Scholar]
- 18.Doherty, P. C., Allan, W., Boyle, D. B., Coupar, B. E. & Andrew, M. E. (1989) J. Infect. Dis. 159, 1119-1122. [DOI] [PubMed] [Google Scholar]
- 19.Lawson, C. M., Bennink, J. R., Restifo, N. P., Yewdell, J. W. & Murphy, B. R. (1994) J. Virol. 68, 3505-3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoffmann, E., Neumann, G., Kawaoka, Y., Hobom, G. & Webster, R. G. (2000) Proc. Natl. Acad. Sci. USA 97, 6108-6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoffmann, E., Krauss, S., Perez, D., Webby, R. & Webster, R. G. (2002) Vaccine 20, 3165-3170. [DOI] [PubMed] [Google Scholar]
- 22.Hoffmann, E., Stech, J., Guan, Y., Webster, R. G. & Perez, D. R. (2001) Arch. Virol. 146, 2275-2289. [DOI] [PubMed] [Google Scholar]
- 23.Flynn, K. J., Belz, G. T., Altman, J. D., Ahmed, R., Woodland, D. L. & Doherty, P. C. (1998) Immunity 8, 683-691. [DOI] [PubMed] [Google Scholar]
- 24.Kitamura, D., Roes, J., Kuhn, R. & Rajewsky, K. (1991) Nature 350, 423-426. [DOI] [PubMed] [Google Scholar]
- 25.Allan, W., Tabi, Z., Cleary, A. & Doherty, P. C. (1990) J. Immunol. 144, 3980-3986. [PubMed] [Google Scholar]
- 26.Hou, S., Hyland, L., Ryan, K. W., Portner, A. & Doherty, P. C. (1994) Nature 369, 652-654. [DOI] [PubMed] [Google Scholar]
- 27.Altman, J. D., Moss, P. A., Goulder, P. J., Barouch, D. H., McHeyzer-Williams, M. G., Bell, J. I., McMichael, A. J. & Davis, M. M. (1996) Science 274, 94-96. [DOI] [PubMed] [Google Scholar]
- 28.Liang, S., Mozdzanowska, K., Palladino, G. & Gerhard, W. (1994) J. Immunol. 152, 1653-1661. [PubMed] [Google Scholar]
- 29.Topham, D. J., Tripp, R. A., Sarawar, S. R., Sangster, M. Y. & Doherty, P. C. (1996) J. Virol. 70, 1288-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mozdzanowska, K., Furchner, M., Maiese, K. & Gerhard, W. (1997) Virology 239, 217-225. [DOI] [PubMed] [Google Scholar]
- 31.Topham, D. J. & Doherty, P. C. (1998) J. Virol. 72, 882-885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Graham, M. B. & Braciale, T. J. (1997) J. Exp. Med. 186, 2063-2068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Riberdy, J. M., Christensen, J. P., Branum, K. & Doherty, P. C. (2000) J. Virol. 74, 9762-9765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grusby, M. J., Johnson, R. S., Papaionnou, V. E. & Glimcher, L. H. (1991) Science 253, 1417-1420. [DOI] [PubMed] [Google Scholar]
- 35.Flynn, K. J., Riberdy, J. M., Christensen, J. P., Altman, J. D. & Doherty, P. C. (1999) Proc. Natl. Acad. Sci. USA 96, 8597-8602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O'Neill, E., Krauss, S. L., Riberdy, J. M., Webster, R. G. & Woodland, D. L. (2000) J. Gen. Virol. 81, 2689-2696. [DOI] [PubMed] [Google Scholar]
- 37.Christensen, J. P., Doherty, P. C., Branum, K. C. & Riberdy, J. M. (2000) J. Virol. 74, 11690-11696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seo, S. H., Hoffmann, E. & Webster, R. G. (2002) Nat. Med. 8, 950-954. [DOI] [PubMed] [Google Scholar]
- 39.Sarawar, S. R., Sangster, M., Coffman, R. L. & Doherty, P. C. (1994) J. Immunol. 153, 1246-1253. [PubMed] [Google Scholar]
- 40.Price, G. E., Gaszewska-Mastarlarz, A. & Moskophidis, D. (2000) J. Virol. 74, 3996-4003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lukacher, A. E., Braciale, V. L. & Braciale, T. J. (1984) J. Exp. Med. 160, 814-826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu, A. N., Mohammed, A. Z., Rice, W. R., Fiedeldey, D. T., Liebermann, J. S., Whitsett, J. A., Braciale, T. J. & Enelow, R. I. (1999) Am. J. Respir. Cell Mol. Biol. 20, 849-858. [DOI] [PubMed] [Google Scholar]
- 43.Gerhard, W. (2001) Curr. Top. Microbiol. Immunol. 260, 171-190. [DOI] [PubMed] [Google Scholar]
- 44.Mozdzanowska, K., Maiese, K., Furchner, M. & Gerhard, W. (1999) Virology 254, 138-146. [DOI] [PubMed] [Google Scholar]
- 45.Eichelberger, M., Allan, W., Zijlstra, M., Jaenisch, R. & Doherty, P. C. (1991) J. Exp. Med. 174, 875-880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Scherle, P. A., Palladino, G. & Gerhard, W. (1992) J. Immunol. 148, 212-217. [PubMed] [Google Scholar]
- 47.Epstein, S. L., Misplon, J. A., Lawson, C. M., Subbarao, E. K., Connors, M. & Murphy, B. R. (1993) J. Immunol. 150, 5484-5493. [PubMed] [Google Scholar]
- 48.Enelow, R. I., Mohammed, A. Z., Stoler, M. H., Liu, A. N., Young, J. S., Lou, Y. H. & Braciale, T. J. (1998) J. Clin. Invest. 102, 1653-1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen, W., Anton, L. C., Bennink, J. R. & Yewdell, J. W. (2000) Immunity 12, 83-93. [DOI] [PubMed] [Google Scholar]
- 50.Legge, K. L. & Braciale, T. J. (2003) Immunity 18, 265-277. [DOI] [PubMed] [Google Scholar]