Abstract
Ribavirin is a nucleotide analog that can be incorporated by viral polymerases, causing mutations by allowing base mismatches. It is currently used therapeutically as an antiviral drug during hepatitis C virus infections. During the amplification of poliovirus genomic RNA or hepatitis C replicons, error frequency is known to increase upon ribavirin treatment. This observation has led to the hypothesis that ribavirin's antiviral activity results from error catastrophe caused by increased mutagenesis of viral genomes. Here, we describe the generation of ribavirin-resistant poliovirus by serial viral passage in the presence of increasing concentrations of the drug. Ribavirin resistance can be caused by a single amino acid change, G64S, in the viral polymerase in an unresolved portion of the fingers domain. Compared with wild-type virus, ribavirin-resistant poliovirus displays increased fidelity of RNA synthesis in the absence of ribavirin and increased survival both in the presence of ribavirin and another mutagen, 5-azacytidine. Ribavirin-resistant poliovirus represents an unusual class of viral drug resistance: resistance to a mutagen through increased fidelity.
Ribavirin (1-β-d-ribofuranosyl-1, 2,4-triazole-3-carboxyamide) is an antiviral compound used in the treatment of infections with hepatitis C, respiratory syncytial and severe acute respiratory viruses. Although ribavirin was known to be a guanosine nucleotide analog, the precise step at which ribavirin exerted its antiviral action was unclear until Crotty and colleagues (1, 2) demonstrated that ribavirin triphosphate is incorporated into viral genomes during RNA synthesis. Incorporated ribavirin causes transition mutations (A-to-G, G-to-A) because of its ability to pair with both uracil and cytosine. Ribavirin has been shown to increase error frequency for both poliovirus genomic RNA and hepatitis C replicon synthesis (1–3). Thus, ribavirin is thought to exert its antiviral activity by increasing the error rate of viral genome replication past the point of “error catastrophe,” whereby the fitness of all members of the viral population is reduced. After several rounds of infection and growth, this can result in extinction of the virus population.
We hypothesized that there may be a link between fidelity of RNA replication and resistance to ribavirin. There is precedent for polymerases with increased fidelity. For example, mutations in the DNA polymerase genes of Escherichia coli and bacteriophage T4 have been shown to confer antimutator phenotypes (4–6). For the retrovirus HIV-1, drug-resistant variants arise during treatment with nucleotide analog chain terminators such as 3TC (2′-deoxy-3′-thiacytidine). The polymerase of one isolate of 3TC-resistant virus contains a mutation, M184V, which is thought to result in reduced incorporation of chain-terminating nucleotide analogs (7). The M184V reverse transcriptase may display altered fidelity of DNA synthesis, though there is some controversy as to whether fidelity is increased or decreased (7–11). Could variants of RNA viruses with increased replicative fidelity display resistance to ribavirin?
In this study, we passaged poliovirus in the presence of ribavirin to select ribavirin-resistant variants. We found that a single nucleotide change in the polymerase coding region was sufficient to generate ribavirin-resistant virus, which showed a nonspecific increase in replicative fidelity. Therefore, ribavirin resistance is likely to be provided by reduced incorporation of nucleotide analogs, decreased susceptibility to the error catastrophe exacerbated by incorporation of nucleotide analogs, or both.
Materials and Methods
Cells and Viruses. HeLa cells were grown in Dulbecco modified Eagle's medium supplemented with 10% calf serum (12). Mahoney serotype 1 poliovirus was grown from a single plaque generated by transfection of the viral cDNA clone (13). Individual plaques were grown into high titer virus stocks by infecting monolayers of HeLa cells. All experiments were performed at 37°C.
Ribavirin Passage Experiments. For the experiments shown in Fig. 1 A and B, 1 × 105 to 5 × 106 HeLa cells on 35- or 60-mm tissue culture dishes were pretreated with or without ribavirin (Sigma) for 1.5 h, and infected at a multiplicity of infection (MOI) of 0.1 plaque-forming units (PFU) per cell. Briefly, 0.2 ml of virus in PBS supplemented with 100 μg/ml CaCl2 and 100 μg/ml MgCl2 (PBS+) was applied to cells and plates were incubated at 37°C for 30 min. The virus was removed, and media with or without ribavirin was added. After 6.5 h, cells were harvested with trypsin, washed with PBS+, and resuspended in 0.1–1 ml of PBS+, depending on the amount of virus used in the experiment. Cells were lysed by freeze-thawing three times, and cell debris was removed by centrifugation. Virus was titered by standard plaque assay (12) to determine the required inoculum for the next passage. This cycle was repeated for several passages, by using an MOI of ≤ 0.1 PFU per cell each passage. After nine serial passages in ribavirin, “pool 3” virus was plaque-purified three times in the presence of 400 μM ribavirin, and the resulting virus isolate was termed 3-1.
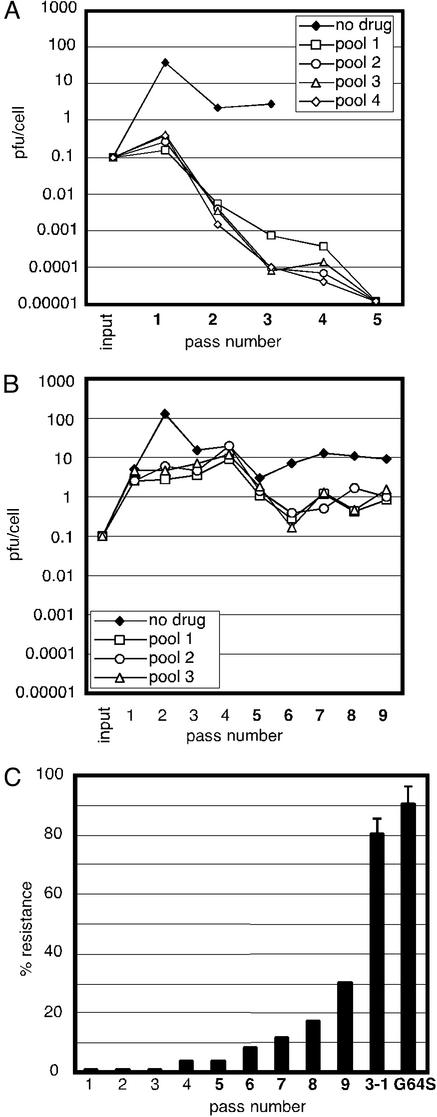
Fig. 1.
Passage of poliovirus in the presence of ribavirin to generate resistance. (A) Viral passage in 400 μM ribavirin. HeLa cells were infected at an MOI of 0.1 PFU per cell in the presence or absence of 400 μM ribavirin. Resulting titers were graphed as a function of passage number. (B) Viral passage in 100 μM ribavirin followed by 400 μM ribavirin. A total of 100 μM ribavirin was used for passages 1–4, and 400 μM ribavirin was used for passages 5–9. (C) Generation of ribavirin resistance during passaging. The percentage resistance for each of nine passages of pool 3 virus stocks from B was determined by titering in the presence or absence of 800 μM ribavirin. The percentage resistance of a virus isolate, 3-1, obtained by three plaque-purification steps in the presence of 400 μM ribavirin, is shown. The percentage resistance of virus containing the single amino acid change G64S is also shown.
Cloning and Identification of the Resistance Mutation. Viral RNA was purified from virions by using the QiaAmp viral RNA isolation kit (Qiagen). RT-PCR was performed with SuperScript II RT (Invitrogen) by using a sense primer upstream of the polymerase-coding region in the 3C-coding region (5′-TTACCAACCCACGCTTCACC-3′) and an antisense primer in the 3′ noncoding region (5′-GGTACAATGTTGAGTACTCTGGG-3′). The PCR products were either sequenced by Sequetech (Mountain View, CA) using a sense primer in the 3D-coding region (5′-GAAATCCAGTGGATGAGACC-3′), or were cloned into the viral cDNA. The 3-1 PCR product was cloned into the viral cDNA vector T7pGEMpolio from nucleotide 5601 (BglII) to nucleotide 7305 (MfeI), which includes most of 3D, the viral polymerase coding region (14). The PCR-generated region was sequenced (Table 1). Finally, a fragment containing only the G64S mutation was subcloned into a new T7pGEMpolio vector in a BglII–AccI fragment. The ribavirin resistance phenotype of this new clone was confirmed by plaque assay and ribavirin serial passage, as described below.
Table 1. Mutations present in the RdRp region of the ribavirin-resistant clone.
| Nucleotide* | Change | Amino acid change |
|---|---|---|
| 6176 | G → A | G64S |
| 6652 | G → A | None |
| 6736 | G → A | None |
| 6879 | A → G | None |
| 7132 | G → A | None |
| 7216 | T → C | None |
Nucleotides 5595-7305 of the resistant virus were subcloned and sequenced.
Nucleotide numbers are from the Mahoney stain of poliovirus type 1
Ribavirin Resistance Assays. Serial passage assays shown in Fig. 3 B and C were performed as in Fig. 1, except a MOI of 10 PFU per cell was used, and viruses were passaged in 0 μM, 400 μM (Fig. 3B), or 800 μM (Fig. 3C) ribavirin. For the plaque assays (Fig. 3A), ≈50 PFU were plated on 1 × 106 HeLa cells on 60-mm dishes. An agar overlay containing various concentrations of ribavirin was added and the plates were incubated at 37°C for 3 days. For Fig. 1C, dilutions of each virus passage stock from pool 3 was used to infect 1 × 106 HeLa cells on 60-mm dishes, and agar overlays with or without 800 μM ribavirin were added. After 3 days at 37°C, cells were stained with crystal violet and plaques were counted.
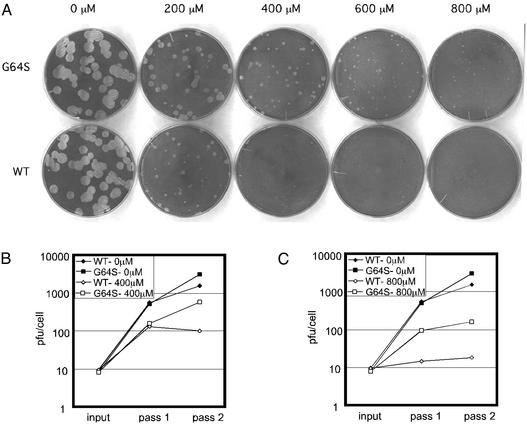
Fig. 3.
Ribavirin-resistance profiles of the selected virus. (A) Plaque assay of G64S and wild-type virus on HeLa cells in the presence of various concentrations of ribavirin. (B) Serial passage of G64S and wild-type virus in the presence or absence of 400 μM ribavirin. HeLa cells were infected at an MOI of 10 PFU per cell in the presence or absence of 400 μM ribavirin. Resulting amounts of virus (PFU per cell) were graphed as a function of passage number. (C) Serial passage of G64S and wild-type virus in the presence or absence of 800 μM ribavirin (performed as in B, in the presence or absence of 800 μM ribavirin).
Fidelity Assays. The apparent error frequencies of wild-type and G64S viruses were measured by a guanidine resistance assay (see Fig. 4 A and B). Briefly, 1 × 106 HeLa cells were infected with dilutions of virus and incubated for 48 h under agar overlays with or without 0.5 mM guanidine HCl (Sigma) (12). The apparent error frequencies were calculated as the titer per ml on plates containing guanidine divided by the titer per ml on plates lacking guanidine. For the guanidine resistance assay, high titer stocks were used in Fig. 4A experiments, and several individual plaque isolates were used in Fig. 4B experiments. Mutagen passage experiments (Fig. 4C) were performed as described for ribavirin passage experiments (Fig. 3 B and C), except cells were treated with or without 5-azacytidine (5-AZC, Sigma).
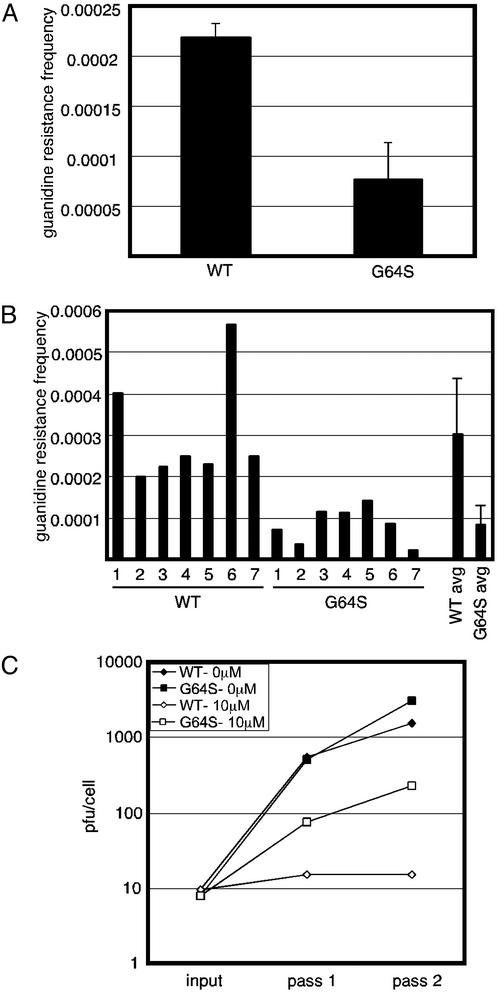
Fig. 4.
Comparative fidelity of wild-type (WT) and G64S mutant virus. (A) The frequency of wild-type and G64S viruses that also contained mutations conferring resistance to 0.5 mM guanidine. Standard errors from two replicate experiments of the stocks used in Fig. 3 are shown. (B) The frequency of viruses that contained mutations conferring resistance to 0.5 mM guanidine for seven independently derived stocks of wild-type and G64S mutant virus. Seven individual measurements, and the average (avg) with standard error, are shown. (C) Serial passage of wild-type and G64S mutant virus in the presence and absence of 10 μM 5-AZC. Passages in the presence and absence of drug were performed as in Fig. 3.
Results
Passage of Poliovirus in the Presence of Ribavirin. In an initial attempt to select ribavirin-resistant poliovirus, we performed serial single-cycle passages of the virus in the presence of 400 μM ribavirin. At 6.5 h after infection with poliovirus at a MOI of 0.1 PFU/cell, cell-associated virus was harvested and titered. After the first cycle, viral titer was reduced ≈50-fold compared with the yield obtained in the absence of drug. When this virus population was titered and used to infect fresh monolayers at the same MOI, the resulting virus yield was reduced >50-fold. This could have resulted either from accumulated genetic damage or from selection of variants with reduced doubling time. In any event, subsequent cycles led to extinction of the passaged population in each of four different pools (Fig. 1 A).
A second passaging experiment with less stringent selection was then performed, using 100 μM ribavirin for the first four passages followed by five passages in the presence of 400 μM ribavirin. During passage in 100 μM ribavirin, no reduction in viral yield was observed and a slight stimulation was observed at passage 4. Therefore, any accumulated mutations at 100 μM ribavirin did not lead to significant genotoxicity (Fig. 1B). However, when this population was grown in the presence of 400 μM ribavirin, the pools of virus were able to withstand passage in the presence of 400 μM ribavirin. After nine single-cycle passages, a single plaque isolate, designated 3-1, was purified from virus pool 3 by three successive plaque-to-plaque transfers in the presence of 400 μM ribavirin.
To monitor the acquisition of ribavirin resistance during passage, each virus stock from the passaging experiment was titered in the presence and absence of 800 μM ribavirin. The percentage of viruses able to form plaques in the presence of ribavirin increased steadily with passage, especially during passage in the presence of 400 μM ribavirin. The isolated 3-1 virus showed >80% plaquing efficiency in the presence of 800 μM ribavirin (Fig. 1C).
Identification of the Mutation Responsible for Resistance to Ribavirin. To identify the mutation or mutations responsible for resistance to ribavirin, the polymerase-coding region of the 3-1 virus genome was cloned by RT-PCR and sequenced. As shown in Table 1, the polymerase-coding region of clone 3-1 contained five silent mutations and one mutation that caused an amino acid change, G64S. All of the observed nucleotide changes were transition mutations and thus could have resulted from ribavirin incorporation during either positive- or negative-strand synthesis. That the resistant clone contained five silent mutations in the polymerase region alone suggests that it is likely that numerous virus derivatives bearing additional amino acid substitutions arose during passage in ribavirin. Presumably, these variants were less fit and therefore did not survive the selection process.
To test whether the mutations in the polymerase coding region were sufficient to confer resistance to ribavirin, a new poliovirus cDNA construct that contained only the mutations in the polymerase coding region was constructed by subcloning the 3-1 PCR product into a new viral cDNA. On transfection of HeLa cells and subsequent ribavirin plaque assay, this virus was confirmed to be ribavirin resistant (data not shown). Finally, to test whether ribavirin resistance was conferred by the G64S substitution, the transition mutation causing the G64S substitution was subcloned into a new viral cDNA. The G64S cDNA was transfected into HeLa cells, individual plaque isolates were recovered, and the resulting viruses were tested in several assays for ribavirin resistance.
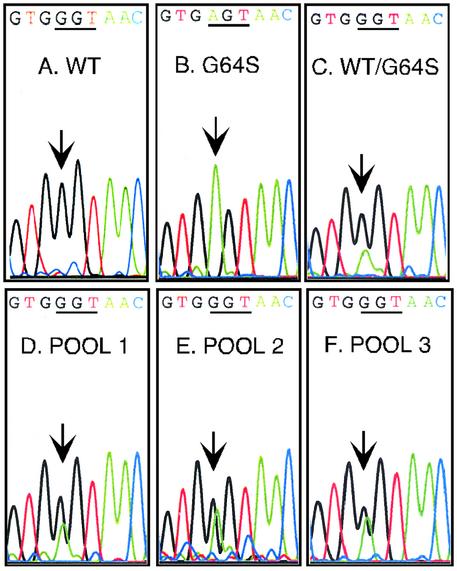
To address whether the G-to-A substitution that created the G64S amino acid change was common among the three separately passaged pools, the viral genomes from passage 9 virus stocks from pools 1, 2, and 3 were amplified by RT-PCR and sequenced. As shown in Fig. 2, the pools of sequence contain both G and A signal in the peak at position 6176 for the three passaged pools, but not for control templates that contain only the wild-type or G64S codon. This finding suggests that the G6176A nucleotide substitution, which is the only possible single mutation that would change the codon at position 64 from Gly to Ser, was present in all three pools that survived serial passage in ribavirin.
Fig. 2.
Sequence of the G64S region in separate pools of virus that display ribavirin resistance. Virion RNA was isolated, amplified by RT-PCR, and sequenced from wild-type virus (A), G64S virus (B), a mixture of wild-type and G64S viruses (C), pool 1 passage 9 (D), pool 2 passage 9 (E), and pool 3 passage 9 (F). The sequencing chromatograms are shown. The wild-type sequence is GTG GGT AAC, and the G64S sequence is GTG AGT AAC. Arrows indicate position 6176, the location of the G-to-A transition mutation in G64S.
Ribavirin-Resistance Profiles of Selected and Reconstituted Virus. One of the reasons it was difficult to demonstrate the mechanism of the antiviral effect of ribavirin is that ribavirin has little effect on single-cycle viral infections. Cell entry, translation, and RNA synthesis of poliovirus, for example, are unaffected by ribavirin at concentrations up to 1,000 μM (1). Instead, the cumulative damage of increased mutagenesis rates becomes apparent at elevated concentrations, or on multiple passage. Therefore, the extent of ribavirin resistance of the 3-1 plaque isolate and the G64S virus was determined by plaque assay in the presence and absence of ribavirin, because development of plaques requires multiple cycles of infection. HeLa cells were infected with ≈50 PFU per monolayer, and an agar overlay containing 0 μMor800 μM ribavirin was added. As shown in Fig. 1C, both the 3-1 virus and the G64S virus showed >80% plaquing efficiency in the presence of 800 μM ribavirin after a 3-day incubation at 37°C. In a second assay, we performed a plaque assay of G64S and wild-type viruses with agar overlays containing different concentrations of ribavirin (Fig. 3A). As observed in Fig. 1B, low doses of ribavirin had little effect on wild-type poliovirus growth (Fig. 3A, 200 μM). However, at higher concentrations of ribavirin, wild-type virus was unable to form plaques, whereas G64S virus formed small plaques (Fig. 3A, 600 and 800 μM). Therefore, G64S virus is relatively resistant to high concentrations of ribavirin.
As an independent method to demonstrate ribavirin resistance, wild-type and G64S viruses were serially passaged in the presence of 0, 400, or 800 μM ribavirin. These assays were performed in the same manner as the initial passaging experiments designed to optimize selection for resistant variants (Fig. 1), except at higher multiplicities of infection. We hypothesized that the higher multiplicities of infection would more closely mimic a natural infection, in which opportunities for complementation and recombination would increase viral survival. Fig. 3 B and C shows the results of passages performed in 400 and 800 μM ribavirin, respectively. At both concentrations of ribavirin, G64S virus was less susceptible to error catastrophe than wild-type virus, an effect amplified during passage.
G64S Poliovirus Displays Increased Fidelity of RNA Synthesis. We envisaged two different models for the mechanism of G64S resistance to ribavirin: either the G64S mutation reduced the binding affinity for ribavirin triphosphate specifically, or the G64S-containing polymerase had a general increase in fidelity. A polymerase with increased fidelity would not only discriminate against ribavirin triphosphate more efficiently, but the virus would also be less vulnerable to mutagen-induced error catastrophe in the presence of any mutagen.
To test the possibility that G64S virus has increased fidelity of RNA synthesis compared with wild-type virus, we performed a guanidine-resistance assay as described by Crotty et al. (1). Poliovirus resistance to guanidine can be generated by single or multiple point mutations in the 2C coding region (1, 15–18). By measuring the number of resistant viruses in a population, an estimation of error frequency can be obtained. Dilutions of G64S or wild-type virus from the high-titer stocks used in the experiments shown in Fig. 3 were plated in the presence or absence of 0.5 mM guanidine in an agar overlay. The average frequencies of guanidine-resistant viruses from two independent experiments are shown in Fig. 4A. To ensure that the observed decrease in guanidine resistance frequency of G64S was not simply due to a “jackpot effect” for a single stock of virus, seven individual plaque isolates of wild-type and G64S viruses were tested in the guanidine resistance assay (Fig. 4B). Although variation existed between plaque isolates, on average, G64S viruses show apparent error frequencies ≈3-fold lower than wild type.
To ask whether the apparently increased fidelity of G64S-containing virus decreased its sensitivity to another mutagen besides ribavirin, G64S and wild-type viruses were passaged in the presence of 5-AZC, which has been used previously to mutagenize RNA viruses (1, 19). First, we determined a concentration of 5-AZC (10 μM) that reduced wild-type virus titer by 70-fold for a single cycle of replication and increased the error frequency in a guanidine resistance assay by ≈4-fold (data not shown), effects comparable to those seen during passage in the presence of 400 μM ribavirin. We then serially passaged G64S and wild-type viruses at an MOI of 10 PFU per cell in the presence or absence of 10 μM 5-AZC and measured viral titer after each passage. As shown in Fig. 4C, G64S virus was less susceptible to error catastrophe in the presence of 10 μM 5-AZC than wild-type virus. That two different assays for fidelity, both performed in the absence of ribavirin, show increased fidelity for the G64S mutant virus argues that the G64S virus is resistant to ribavirin because of a general increase in fidelity that is not mutagen-specific.
Discussion
Here we describe the generation of ribavirin-resistant poliovirus by serial passage in the presence of the drug. Interestingly, no drug-resistant virus was isolated from passages in 400 μM ribavirin. Instead, data in Fig. 1C suggest that passage of virus at a lower concentration of ribavirin was necessary to allow the accumulation of mutations before the stringent selection for resistant variants provided by passage in 400 μM ribavirin. In hepatitis C virus (HCV)-infected patients treated with ribavirin, estimates of the drug concentrations in blood plasma range from 10 to 30 μM, though the concentration in hepatocytes may be higher (20, 21). Although it is uncertain whether the concentration of ribavirin required to inhibit poliovirus growth is similar to the concentration required to inhibit HCV growth, the results presented here suggest that treatment with low concentrations of the drug could facilitate later selection of resistant variants. In fact, clinical data from HCV patients have shown that short-term therapy with high doses of ribavirin is more effective than long-term therapy with low doses (22).
Several mechanisms could have explained the observed ribavirin resistance of G64S virus. Compared with wild-type virus, a ribavirin-resistant virus could simply amplify its RNA more slowly, and therefore acquire fewer mutations over any given time period. It has been proposed that, in complex virus populations, fitness level and replication rate are as important as the error rate in determining quasispecies diversity (23). However, plaques formed by the G64S virus (Fig. 3A) and viral titers after single-cycle infection (Fig. 3B) are identical to those of wild-type virus. Furthermore, in the guanidine-resistance assay, where G64S virus showed a 3-fold increase in fidelity, fitness differences cannot affect the apparent error frequency because it is a ratio of the number of plaques grown in the presence and absence of guanidine. Therefore, it is not likely that a slower rate of RNA replication is responsible for the decreased susceptibility of G64S virus to ribavirin.
Another possible mechanism by which G64S virus might have acquired resistance to ribavirin is via a specific defect in RTP binding or incorporation. Because increased fidelity of G64S virus was observed in the guanidine-resistance assay (Fig. 4 A and B), and cross-resistance to 5-azacytidine was observed in viral passaging experiments (Fig. 4C), it is unlikely that the sole determinant of ribavirin resistance is a specific reduction in RTP binding or incorporation.
We favor, therefore, a third mechanism to explain the resistance of G64S virus to ribavirin: the G64S mutation confers a general increase in the fidelity of RNA replication. This increased fidelity can have two outcomes that affect the survival of the G64S virus in the presence of mutagens such as ribavirin and 5-azacytidine. First, the increased fidelity could decrease the incorporation of all or most nucleotide analogs relative to the appropriate nucleotides. Second, a general increase in fidelity could simply reduce the average number of mutations per genome in the absence of mutagen, such that then, in the presence of mutagen, the virus population can better withstand additional genomic damage. These possibilities are not mutually exclusive and can be tested by determining the rates of RTP incorporation for G64S and wild-type polymerases (1).
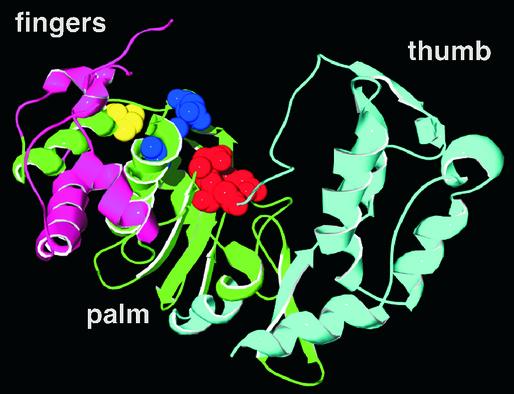
As with most polymerases, the poliovirus polymerase can be likened to a right hand with palm, fingers, and thumb subdomains (Fig. 5). The active site of the polymerase is located in the palm region, where conserved aspartate residues facilitate catalysis. The structure of the poliovirus polymerase has been determined, though a large portion of the fingers domain remains unresolved, including Gly-64 (23, 24). In the polymerase structure shown in Fig. 5, we indicated the approximate location of Gly-64 based on the nearest resolved residue, Ile-67. Although this region of the fingers may seem distant from the active-site residues, the fingers may undergo substantial rearrangement during polymerization. For HIV-1 reverse transcriptase and TaqDNA polymerase I, structures of catalytically trapped complexes show significant rearrangements of the fingers domain relative to structures of the apoenzymes (25, 26). For example, the fingers of HIV-1 reverse transcriptase fold in toward the active site by 20° and residues in the fingertips move >5 Å in the conformation most likely to represent the active form (25). The locations of certain HIV-RT mutations that conferred resistance to the chain terminating nucleotide analog AZT, D67N, K70R, T215Y/F, and K219Q, were not readily interpretable until the structure of the catalytically trapped complexes were solved (25, 27). Some of these mutated residues (D67N and K70R) mapped to positions in the fingertips far from the active site in the “open complex”; however, in the closed, active complex, they were closer to the active aspartates (25). Therefore, it is possible that during catalysis by the poliovirus polymerase, Gly-64 may be closer to the active site than is apparent in Fig. 5. Interestingly, Gly-64 is likely to be near Lys-61, a side chain previously shown to be susceptible to nucleotide cross-linking (28–30). We propose that Gly-64 is near a nucleotide-binding site in the fingers domain, and that mutation of this glycine to the bulkier serine may reduce the space for base mispair formation or reduce the flexibility of the fingers domain. Residues Asp-238 and Asn-297 have been reported to play a role in nucleotide binding and selection (31). These residues are near the active site, and may bind the incoming nucleotide from the side opposite to Gly-64 and Lys-61 (Fig. 5).
Fig. 5.
Poliovirus polymerase structure. The known structure of poliovirus polymerase (23) is shown. Catalytic aspartate residues in the active site, 328, 329, and 233 are shown in red, residues thought to contact nucleotide substrates directly are shown in royal blue (31), and Ile-67, the closest resolved residue to Gly-64, is shown in yellow.
To our knowledge, G64S poliovirus is the first example of a picornavirus with increased fidelity in RNA synthesis. Initially, it seems counterintuitive that a mutant virus would have higher fidelity than wild-type virus. However, the wild-type virus may have been optimized for replication at the brink of error catastrophe to facilitate viral survival under variable growth conditions (32, 33). Although G64S virus has thus far displayed no growth defect compared with wild-type virus, it will be interesting to test whether G64S virus can grow as well as wild-type virus in animals, or whether increased fidelity will be disadvantageous in an environment of increased complexity.
Acknowledgments
We thank Joanna Boerner, Scott Crowder, and Peter Sarnow for critical review of the manuscript and helpful suggestions. This work was supported by the National Institutes of Health and the Hutchison Foundation for Translational Research. J.K.P. is a Rebecca Ridley Kry Fellow of the Damon Runyon Cancer Research Foundation.
Abbreviations: MOI, multiplicity of infection; PFU, plaque-forming units; 5-AZC, 5-azacytidine.
References
- 1.Crotty, S., Maag, D., Arnold, J. J., Zhong, W., Lau, J. Y., Hong, Z., Andino, R. & Cameron, C. E. (2000) Nat. Med. 6, 1375-1379. [DOI] [PubMed] [Google Scholar]
- 2.Crotty, S., Cameron, C. E. & Andino, R. (2001) Proc. Natl. Acad. Sci. USA 98, 6895-6900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Contreras, A. M., Hiasa, Y., He, W., Terella, A., Schmidt, E. V. & Chung, R. T. (2002) J. Virol. 76, 8505-8517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gillin, F. D. & Nossal, N. G. (1976) J. Biol. Chem. 251, 5219-5224. [PubMed] [Google Scholar]
- 5.Schaaper, R. M. (1998) Genetics 148, 1579-1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muzyczka, N., Poland, R. L. & Bessman, M. J. (1972) J. Biol. Chem. 247, 7116-7122. [PubMed] [Google Scholar]
- 7.Wainberg, M. A., Drosopoulos, W. C., Salomon, H., Hsu, M., Borkow, G., Parniak, M., Gu, Z., Song, Q., Manne, J., Islam, S., et al. (1996) Science 271, 1282-1285. [DOI] [PubMed] [Google Scholar]
- 8.Rezende, L. F., Drosopoulos, W. C. & Prasad, V. R. (1998) Nucleic Acids Res. 26, 3066-3072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mansky, L. M., Pearl, D. K. & Gajary, L. C. (2002) J. Virol. 76, 9253-9259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drosopoulos, W. C. & Prasad, V. R. (1998) J. Virol. 72, 4224-4230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keulen, W., van Wijk, A., Schuurman, R., Berkhout, B. & Boucher, C. A. (1999) AIDS 13, 1343-1349. [DOI] [PubMed] [Google Scholar]
- 12.Kirkegaard, K. & Baltimore, D. (1986) Cell 47, 433-443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Racaniello, V. R. & Baltimore, D. (1981) Proc. Natl. Acad. Sci. USA 78, 4887-4891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ausubel, F. M., Brent, R., Kingston, R. E., Moore, D. D., Smith, J. A. & Struhl, K. (1994) Current Protocols in Molecular Biology (Wiley, New York).
- 15.Tolskaya, E. A., Romanova, L. I., Kolesnikova, M. S., Gmyl, A. P., Gorbalenya, A. E. & Agol, V. I. (1994) J. Mol. Biol. 236, 1310-1323. [DOI] [PubMed] [Google Scholar]
- 16.Pincus, S. E., Diamond, D. C., Emini, E. A. & Wimmer, E. (1986) J. Virol. 57, 638-646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pincus, S. E. & Wimmer, E. (1986) J. Virol. 60, 793-796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pincus, S. E., Rohl, H. & Wimmer, E. (1987) Virology 157, 83-88. [DOI] [PubMed] [Google Scholar]
- 19.Sierra, S., Davila, M., Lowenstein, P. R. & Domingo, E. (2000) J. Virol. 74, 8316-8323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Larrat, S., Stanke-Labesque, F., Plages, A., Zarski, J. P., Bessard, G. & Souvignet, C. (2003) Antimicrob. Agents Chemother. 47, 124-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bruchfeld, A., Lindahl, K., Schvarcz, R. & Stahle, L. (2002) Ther. Drug Monit. 24, 701-708. [DOI] [PubMed] [Google Scholar]
- 22.da Silva, L. C., Bassit, L., Ono-Nita, S. K., Pinho, J. R., Nishiya, A., Madruga, C. L. & Carrilho, F. J. (2002) J. Gastroenterol. 37, 732-736. [DOI] [PubMed] [Google Scholar]
- 23.Hansen, J. L., Long, A. M. & Schultz, S. C. (1997) Structure (London) 5, 1109-1122. [DOI] [PubMed] [Google Scholar]
- 24.Hobson, S. D., Rosenblum, E. S., Richards, O. C., Richmond, K., Kirkegaard, K. & Schultz, S. C. (2001) EMBO J. 20, 1153-1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang, H., Chopra, R., Verdine, G. L. & Harrison, S. C. (1998) Science 282, 1669-1675. [DOI] [PubMed] [Google Scholar]
- 26.Patel, P. H., Suzuki, M., Adman, E., Shinkai, A. & Loeb, L. A. (2001) J. Mol. Biol. 308, 823-837. [DOI] [PubMed] [Google Scholar]
- 27.Larder, B. A. & Kemp, S. D. (1989) Science 246, 1155-1158. [DOI] [PubMed] [Google Scholar]
- 28.Richards, O. C., Hanson, J. L., Schultz, S. C. & Ehrenfeld, E. (1995) Biochemistry 34, 6288-6295. [DOI] [PubMed] [Google Scholar]
- 29.Richards, O. C., Baker, S. & Ehrenfeld, E. (1996) J. Virol. 12, 8564-8570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Richards, O. C. & Ehrenfeld, E. (1997) J. Biol. Chem. 272, 23261-23264. [DOI] [PubMed] [Google Scholar]
- 31.Gohara, D. W., Crotty, S., Arnold, J. J., Yoder, J. D., Andino, R. & Cameron, C. E. (2000) J. Biol. Chem. 275, 25523-25532. [DOI] [PubMed] [Google Scholar]
- 32.Domingo, E. & Holland, J. J. (1997) Annu. Rev. Microbiol. 51, 151-178. [DOI] [PubMed] [Google Scholar]
- 33.Drake, J. W., Charlesworth, B., Charlesworth, D. & Crow, J. F. (1998) Genetics 148, 1667-1686. [DOI] [PMC free article] [PubMed] [Google Scholar]