Abstract
N-3-(oxododecanoyl)-l-homoserine lactone (OdDHL), a quorum-sensing molecule of Pseudomonas aeruginosa, plays an important role in the pathogenesis of the organism through its control of virulence factor expression. Several reports have suggested that OdDHL can also directly modulate host immune responses. However, the nature of the modulation is controversial, with different reports suggesting promotion of either humoral (Th2-mediated) or inflammatory (Th1-mediated) responses. This report describes a series of studies which demonstrate for the first time that in vivo administration of OdDHL can modulate the course of an antibody response, with an increase in ovalbumin (OVA)-specific immunogloblulin G1 (IgG1) but not IgG2a in OdDHL-treated OVA-immunized BALB/c mice compared to levels for controls. In vitro stimulation of lymphocytes from both Th1-biased C57Bl/6 and T-cell receptor transgenic mice and Th2-biased BALB/c mice in the presence of OdDHL demonstrated that OdDHL inhibits in vitro cytokine production in response to both mitogen and antigen, with gamma interferon (IFN-γ) tending to be more inhibited than interleukin-4 (IL-4). In vitro mitogen or antigen restimulation of cells from mice treated with OdDHL in vivo shows effects on cytokine production which depend on the underlying immune bias of the mouse strain used, with a relative increase of IFN-γ in Th1-biased C57Bl/6 mice and a relative increase of IL-4 in Th2-biased BALB/c mice. Thus, the mode of action of OdDHL on T-cell cytokine production is likely to be a relatively nonspecific one which accentuates an underlying immune response bias rather than one which specifically targets either Th1 or Th2 responses.
N-(3-oxododecanoyl)-l-homoserine lactone (OdDHL), a member of the acylated homoserine lactone (AHL) family of bacterial signaling molecules, is utilized by Pseudomonas aeruginosa to coordinate population behavior and to control the expression of numerous virulence factors in a population density-dependent fashion (12, 16, 34, 36, 37, 52). P. aeruginosa is a significant pathogen of immunocompromised individuals, including burn patients (24, 38, 39, 49), and human immunodeficiency virus and AIDS patients (1, 17), and patients with the genetic disorder cystic fibrosis (15, 22), and is a common cause of ocular (21) and cutaneous (45) infections. OdDHL is clearly an important factor in the pathogenesis of P. aeruginosa because of its role in the control of the expression of virulence factors, such as elastase, alkaline protease, and pyoverdine (12, 16, 34, 36, 37, 52), and it has been demonstrated in animal models that strains of P. aeruginosa which produce no OdDHL or which are resistant to its actions are less virulent than OdDHL-producing strains (35, 53). However, several reports have suggested that OdDHL can directly affect mammalian cell function, including that of cells of the immune system, and thus that the contribution of OdDHL to pathogenesis may be partly due to effects on host immune responses.
Telford et al. (51) reported that the in vitro production of interleukin-12 (IL-12) and tumor necrosis factor alpha (TNF-α) by lipopolysaccharide (LPS)-stimulated macrophages is inhibited by OdDHL and that, in an in vitro model of B-cell activation, the production of immunoglobulin G1 (IgG1) antibodies and IgE but not other antibody subclasses was elevated by OdDHL. This led the group to propose that OdDHL acts to modulate a T-cell-mediated immune response from a type 1 (Th1, proinflammatory) response to a type 2 (Th2, antiinflammatory) response. By contrast, Smith et al. (47) observed that stimulation of T-cell receptor (TCR) transgenic murine splenic T cells with antigen in vitro in the presence of OdDHL followed by restimulation of those T cells without OdDHL resulted in increased production of gamma interferon (IFN-γ), with little or no effect on IL-4 production. Smith et al. (47) have also shown that OdDHL injected intradermally into inbred mice induced an influx of inflammatory cells to, and increased production of proinflammatory mediators at, the site of injection. Together with data from two groups suggesting that OdDHL induced IL-8 production by epithelial cells (7, 46, 48), these data suggested that rather than promoting Th2 responses, OdDHL promoted an inflammatory Th1 response.
The conflicting in vitro data of Telford et al. (51) and Smith et al. (47), plus the paucity of data available on the effect of OdDHL on adaptive immune responses in vivo, led us to investigate the effect of pure, synthetic OdDHL in a range of in vivo and in vitro models of T- and B-cell-mediated responses, including in vivo antibody responses to a protein antigen, ovalbumin (OVA), and both antigen- and mitogen-induced T-cell cytokine production in vitro. To investigate the relative effects of OdDHL on Th1 and Th2 immune responses, we have studied both Th1-biased C57BL/6 (6, 50, 54) and Th2-biased BALB/c (42, 50) mice and a TCR transgenic mouse strain where 50 to 80% of the T cells express a receptor specific for a peptide of moth cytochrome c (MCC) plus major histocompatibility complex (MHC) class II. We chose models of immune responses to defined protein antigens in order to separate the direct effect of OdDHL on immunity from the feedback effect of AHL signaling on bacterial growth and virulence factor production that would complicate any infectious model. The data presented in this report support the hypothesis that immunomodulation by OdDHL is a relatively nonspecific phenomenon and that the effects of OdDHL on immunity are dependent on the experimental context, the mouse strain used, and whether the responses measured are antigen specific or mitogen induced. This report also provides the first evidence of a direct effect of OdDHL on in vivo antigen-specific immunity and suggests a basis for rationalizing the apparently conflicting reports of the effects of OdDHL in vitro.
MATERIALS AND METHODS
Mice.
Female specific-pathogen-free C57Bl/6 mice were purchased from the Animal Resource Centre (Canningvale, Australia) and were between 10 and 14 weeks of age when used. Female specific-pathogen-free BALB/c mice were purchased from the Biological Resource Centre (Little Bay, Australia) and were between 10 and 14 weeks of age when used. TCR transgenic mice that are on a B10.Br background and express a TCR specific for the COOH-terminal epitope of MCC plus MHC class II on 50 to 80% of peripheral CD4+ T cells (19) were bred in house from homozygous breeding pairs kindly provided by B. Fazekas de St. Groth, and male mice 10 to 14 weeks of age were used for experiments. Mice were housed in accordance with National Health and Medical Research Council guidelines and were given sterile food and water ad libitum. All animal experiments were approved by the University of New South Wales Animal Care and Ethics Committee (ACEC00/01).
OdDHL.
OdDHL was synthesized by Naresh Kumar, School of Chemical Sciences, University of New South Wales, according to the method described by Bycroft et al. (2). The resulting OdDHL was checked for identity and purity by nuclear magnetic resonance, and its activity as a quorum-sensing molecule was confirmed by the quorum-sensing bioassay described by Fuqua and Winans (11).
In vivo treatments.
Sixty C57Bl/6 and 80 BALB/c mice were immunized intraperitoneally (i.p.) with 0.5-ml injections of alum-precipitated OVA [OVA-alum; 100 μg of OVA (Sigma, St. Louis, Mo.)/ml, 5% (wt/vol) AlK(SO4)2 · 12H2O (Sigma), 0.1% (wt/vol) Al(OH)3 (Sigma), pH 7.2]. One hour later 30 C57Bl/6 and 40 BALB/c treatment animals were given 0.2-ml i.p. injections of 100 μM OdDHL (approximately 0.3 mg/kg of body weight) in 1% dimethyl sulfoxide (DMSO; Sigma) in Dulbecco's Ca2+ and Mg2+ free phosphate-buffered saline (PBS), pH 7.2 (treatment), and 30 C57Bl/6 and 40 BALB/c control animals were given 0.2-ml i.p. injections of 1% DMSO in PBS (control).
Cell and serum collection.
For C57Bl/6 mice treated in vivo, groups of 10 treatment and 10 control mice were euthanized by CO2 asphyxiation and cervical dislocation 2, 4, and 8 days postinjection, and their spleens were removed for cell culture. For BALB/c mice treated in vivo, groups of 10 treatment and 10 control mice were euthanized by CO2 asphyxiation and cervical dislocation 2, 4, and 8 days postinjection, and their spleens were removed for cell culture. Twenty-two days postinjection groups of 10 treatment and 10 control BALB/c mice were anesthetized with 1.25 mg of Xylazil-20 (Troy Laboratories Pty. Ltd., Smithfield, Australia)/mouse and 1.25 mg of Ketamil (Troy Laboratories Pty. Ltd.)/mouse, and blood was collected by cardiac puncture for antibody subclass analysis. Mice were then euthanized by cervical dislocation, and their spleens were removed for cell culture. Prior to immunization, these same mice each had a small volume of blood removed by cardiac puncture while anesthetized in order to analyze background levels of anti-OVA antibody. For in vitro stimulation of splenocytes from unimmunized mice, unimmunized BALB/c, C57Bl/6, or TCR transgenic mice were euthanized by CO2 asphyxiation and cervical dislocation and their spleens were removed for cell culture.
Spleen cell culture.
Single spleen cell suspensions were prepared and erythrocytes were removed by incubation in red cell lysis solution (1.5 M NH4Cl [Ajax Chemicals, Auburn, Australia], 100 mM NaHCO3 [Ajax Chemicals], 10 mM disodium EDTA [Sigma], pH 7.2) for 12 min, followed by resuspension in cell culture media (CCM; 10% [vol/vol] heat-inactivated fetal calf serum [Trace Bioscience, Castle Hill, Australia], 2 mM l-glutamine [Gibco BRL, Gaithersburg, Md.], 50 U of penicillin-streptomycin [Gibco BRL]/ml in RPMI 1640 [Gibco BRL]). For cytokine protein analysis, splenocytes were cultured at 2 ml per well in 24-well tissue culture plates (Greiner GmbH, Maybachstrasse, Germany) at 37°C in 5% CO2 at a concentration of 2 × 106 cells/ml for in vivo BALB/c experiments and 1 × 106 cells/ml for all other experiments. For cytokine mRNA analysis, splenocytes were cultured in 10-ml volumes in 50-ml tissue culture flasks (Greiner GmbH) at 37°C in 5% CO2 at a concentration of 106 cells/ml. Splenocytes from each individual unimmunized C57Bl/6 and BALB/c animal were incubated in CCM alone or were stimulated by using 5 μg of concanavalin A (ConA; Sigma)/ml in the presence of either various concentrations of OdDHL in 0.1% DMSO or in 0.1% DMSO only. For cytokine protein analysis, splenocytes from each individual unimmunized TCR transgenic animal were incubated in CCM alone or were stimulated by using 5 μM MCC variant peptide T102S (MCCT102S; Auspep, Parkville, Australia) (MCCT102S is reported to induce higher levels of both IFN-γ and IL-4 than the native peptide at the doses used in this study [40]) in the presence of either various concentrations of OdDHL in 0.1% DMSO or in 0.1% DMSO only. For analysis of the toxicity of OdDHL, splenocytes from unimmunized TCR mice were incubated in CCM in the presence of either various concentrations of OdDHL in 0.1% DMSO or in 0.1% DMSO only. Cells were harvested after 2 h, and cell death was analyzed by propidium iodide staining and flow cytometry. For cytokine mRNA analysis, splenocytes from individual unimmunized TCR transgenic mice were incubated in CCM alone or were stimulated by using 5 μM MCCT102S in the presence of 4 or 10 μM OdDHL in 0.2% DMSO or 0.2% DMSO only. Cells were harvested at 4, 8, and 12 h poststimulation, and total RNA was prepared as described below. Splenocytes from immunized C57Bl/6 and BALB/c mice were incubated in CCM alone or were stimulated by using either 200 μg of OVA/ml or 5 μg of ConA/ml. For assay of cytokine protein all supernatants were harvested after 48 h, at which time preliminary experiments had demonstrated the highest detected cytokine levels, and were stored in aliquots at −70°C until assayed.
Cytokine protein analysis.
IFN-γ and IL-4 levels in cell culture supernatants were analyzed by using enzyme-linked immunosorbent assay (ELISA) minikit development systems (Endogen, Woburn, Mass.) and the following procedure. Ninety-six-well Maxisorp plates (Nalge Nunc International Corp., Naperville, Ill.) were coated with 100 μl of the appropriate capture antibody/well at 50% of the recommended concentration for all IFN-γ plates and IL-4 plates used for analyzing ConA-stimulated samples and at 100% of the recommended concentration for IL-4 plates used for analyzing OVA, MCCT102S-stimulated samples, and unstimulated samples, and were incubated at room temperature for 18 to 20 h. Plates were blocked at room temperature for 1 h with a 200-μl/well concentration of 2% (wt/vol) bovine serum albumin (BSA; Sigma) in PBS. Plates were washed three times with wash buffer (50 mM Tris [Amresco, Solon, Ohio], 0.2% polyoxyethylene-sorbitan monolaurate [Tween-20; Sigma] in PBS) and 100-μl/well concentrations of appropriate dilutions of test samples and standards in 2% (wt/vol) BSA in PBS were added, and the plates were incubated for 18 to 20 h. Plates were washed three times, and 100-μl/well concentrations of the appropriate biotin-labeled detection antibody were added at 50% of the recommended concentration for all IFN-γ plates and IL-4 plates used for analyzing ConA-stimulated samples and at 100% of the recommended concentration for IL-4 plates used for analyzing OVA, MCCT102S-stimulated samples, and unstimulated samples. Plates were incubated for 1 h at room temperature and then were washed three times. A concentration of 100 μl/well of a 1:6,400 dilution of streptavidin-bound horseradish peroxidase (Amersham Pharmacia Biotech, Buckinghamshire, United Kingdom) was added, and plates were incubated for 45 min at room temperature. Plates were washed three times, and 100-μl/well concentrations of ELISA substrate (0.0125% [wt/vol] tetramethylbenzidine [Sigma], 0.02% [vol/vol] hydrogen peroxide [MERCK Pty. Ltd.], 3.6% methanol [Asia Pacific Specialty Chemicals Ltd., Seven Hills, Australia] in 0.1 M citrate acetate [0.1 M citric acid; MERCK Pty. Ltd.], 0.1 M sodium acetate [Ajax Chemicals], pH 6.0) were added and developed in the dark for 20 min before the addition of 100 μl of 0.2 M sulfuric acid (MERCK Pty. Ltd.)/well. The absorbance of samples and standards at 450 nm was read by using a Benchmark Microplate Reader (Bio-Rad Laboratories, Hercules, Calif.), and the concentrations of IFN-γ and IL-4 were calculated by using Microplate Manager version 5.0.1 (Bio-Rad Laboratories) and GraphPad Prism version 3.00 for Windows (GraphPad Software, San Diego, Calif.).
Cytokine mRNA analysis.
Cells from in vitro cultures were centrifuged at 300 × g for 10 min, the supernatants were removed, and total RNA was extracted by using TRIzol reagent (Invitrogen, Gaithersburg, Md.) according to the manufacturer's instructions. Resultant RNA was treated with DNase (Ambion DNA-free kit; Austin, Tex.) to increase purity of RNA, and the concentration was assessed by spectrophotometry. One microgram of total RNA in a volume of 20 μl was reverse transcribed by using Superscript II (Invitrogen) according to the manufacturer's instructions. Each reaction set included control RNA that was not subjected to reverse transcription.
IFN-γ, IL-4, and β-actin mRNA was analyzed by using semiquantitative PCR. All cDNA samples were amplified in three separate PCRs by using three different sets of primers: β-actin primers as a housekeeping control, IFN-γ primers, and IL-4 primers. The IFN-γ and β-actin primers were as described by Overbergh et al. (31) and were purchased from Sigma Aldrich (St. Louis, Mo.). The expected size of the amplified cDNA product for IFN-γ was 92 bp, and the expected size of the amplified cDNA product for β-actin was 138 bp. IFN-γ and β-actin PCRs contained 4% (vol/vol) cDNA from 1 μg of RNA, 0.5 μM each of the forward and reverse primers, 10 mM deoxynucleoside triphosphates (Promega Corp., Madison, Wis.), 0.08 U of Taq polymerase (Promega), 100 mM KCl, 20 mM Tris-HCl (pH 9.0 at 25°C), 1% Triton X-100, and 2 mM MgCl2. IFN-γ and β-actin PCRs were performed for 2 min at 94°C followed by a total of 25 cycles of 30 s at 94°C, 30 s at 60°C, and 45 s at 75°C by using a Hybaid PCR express machine (Hybaid, Middlesex, United Kingdom). The IL-4 primers had the sequences 5′-AGAGCTATTGATGGGTCTCA-3′ and 5′-CACCTTGGAAGCCCTACAG-3′ and were purchased from GeneWorks (Adelaide, Australia). The expected size of the amplified cDNA product for IL-4 was 232 bp. IL-4 PCRs contained 4% (vol/vol) cDNA from 1 μg of RNA, 0.2 μM each primer, and 50% (vol/vol) commercial PCR master mix (Invitrogen). PCR was performed for 3 min at 95°C followed by a total of 40 cycles of 15 s at 95°C and 60 s at 60°C by using a Rotor-Gene RG3000 PCR machine (Corbett Research, Cambridge, United Kingdom). All PCR products were resolved on an 8% Tris-borate-EDTA polyacrylamide gel.
Antibody subclass analysis.
OVA-specific IgG1 and IgG2a antibody levels in serum from BALB/c mice preimmunization and 22 days postimmunization were analyzed by using class-specific anti-heavy chain antibodies, and ELISAs were developed in the laboratory. Polysorp 96-well plates (Nalge Nunc International Corp.) were coated with a 100-μl/well concentration of 10 (for IgG1 ELISA) or 20 μg (for IgG2a ELISA) of OVA/ml and were incubated for 18 h at room temperature. Plates were blocked for 1 h at room temperature with 200 μl of 2% (wt/vol) BSA in PBS/well. Plates were washed three times, and 150-μl/well concentrations of appropriate dilutions of test sera and standards, which were developed in our laboratory by using pooled sera from OVA-immunized mice, in 2% (wt/vol) BSA in PBS were added. Plates were incubated for 3 h at room temperature and were washed three times, and 100-μl/well concentrations of 1 μg of biotin-labeled rat anti-mouse IgG2a heavy chain-specific antibody (Serotec Ltd., Oxford, United Kingdom)/ml or 250 ng of rat-anti mouse IgG1 heavy chain-specific antibody (Serotec)/ml were added and incubated for 2 h. Plates were washed three times, and 100 μl of a 1:8,000 dilution of streptavidin-horseradish peroxidase per well was added and incubated for 1 h. Plates were washed three times, and 100 μl of ELISA substrate per well was added and allowed to develop in the dark for 1 h before the addition of 100 μl of 0.2 M sulfuric acid/well. The absorbances of samples and standards at 450 nm were read by using a Benchmark Microplate Reader, and the relative concentration of OVA-specific IgG2a or IgG1, compared to that of the set of standards developed in our lab, was calculated by using Microplate Manager version 5.0.1.
Statistical analysis.
Statistical analysis of all in vitro cytokine protein data comparing OdDHL-treated groups to untreated controls was carried out by using the Friedman test followed by Dunn's posttest. Statistical analysis of in vivo cytokine protein data, comparing changes in IFN-γ production by cells from OdDHL-treated animals to IFN-γ production by cells from control animals and comparing changes in IL-4 production by cells from OdDHL-treated animals to IL-4 production by cells from control animals, was carried out by using the Mann-Whitney test. Statistical analysis of in vivo antibody data, comparing data for OdDHL-treated groups to data for untreated controls, was carried out by using the Mann-Whitney test. All statistical analyses were carried out by using GraphPad Prism version 3.00 for Windows.
RESULTS
Cytokine production by nonimmunized murine splenocytes following mitogen stimulation in vitro.
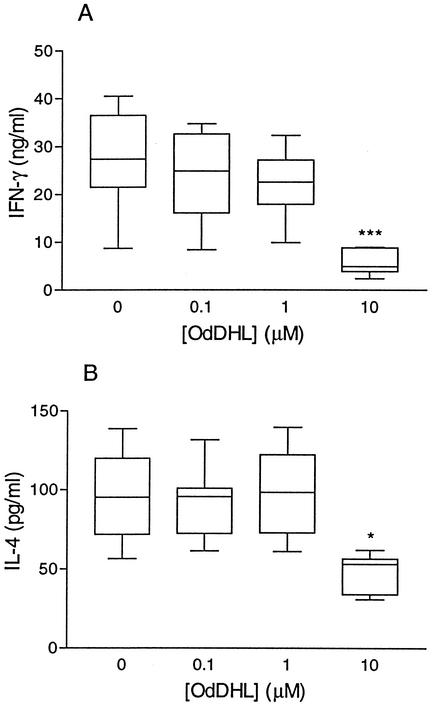
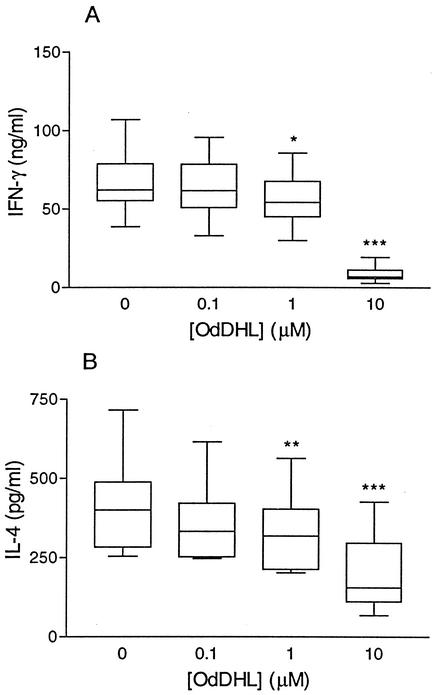
The cytokines IFN-γ and IL-4 were chosen for analysis in this study as markers of the Th1 and Th2 responses, respectively (5, 30), although it should be remembered that cells other than Th cells (such as CD8+ T cells and NK cells) present in the mixed splenocyte populations may also be producing IFN-γ, and it is possible that OdDHL is also affecting these cells. In order to study the effects of OdDHL on the balance of cytokine production by murine splenocytes undergoing a primary immune response in vitro, both C57Bl/6 and BALB/c mice were used, as they are representative of immune responses that tend to be biased towards Th1 and Th2, respectively. The observation that C57Bl/6 mice favor a more Th1-type response while BALB/c mice favor a more Th2-type response is confirmed by the ratios of IFN-γ and IL-4 produced by splenocytes undergoing in vitro stimulation by mitogen (ConA) in the absence of OdDHL (Fig. 1 and 2). In the case of C57Bl/6 mice, median IFN-γ production was 27.3 ng/ml (Fig. 1A) and median IL-4 production was 95 pg/ml (Fig. 1B), giving an IFN-γ-to-IL-4 ratio of 287. In the case of BALB/c mice, median IFN-γ production was 62 ng/ml (Fig. 2A) and median IL-4 production was 400 pg/ml (Fig. 2B), giving an IFN-γ-to-IL-4 ratio of 155. To examine the effects of OdDHL on this cytokine production profile, splenocytes from C57Bl/6 and BALB/c mice were stimulated with ConA in the presence of various concentrations of OdDHL, and cell culture supernatants were harvested following 48 h of incubation, which had previously been determined to represent peak production of both IFN-γ and IL-4. All supernatants from cell cultures that did not include mitogen were found to produce undetectable levels of IFN-γ and IL-4 (data not shown).
FIG. 1.
The production of IFN-γ and IL-4 by C57Bl/6 splenocytes exposed to OdDHL in vitro. Splenocytes from unimmunized C57Bl/6 mice were stimulated with 5 μg of ConA/ml and were exposed to various concentrations of OdDHL. An ELISA was used to quantify IFN-γ (A) and IL-4 (B) protein levels following 48 h of incubation. Data are represented as the medians ± 25th and 75th percentiles (boxes). Error bars represent the maximum and minimum values; n = 10 (A) or 9 (B). *, P < 0.05 compared to results for untreated cells; ***P < 0.001 compared to results for untreated cells.
FIG. 2.
The production of IFN-γ and IL-4 by BALB/c splenocytes exposed to OdDHL in vitro. Splenocytes from unimmunized BALB/c mice were stimulated with 5 μg of ConA/ml and were exposed to various concentrations of OdDHL. An ELISA was used to quantify IFN-γ (A) and IL-4 (B) protein levels following 48 h of incubation. Data are represented as the median ± 25th and 75th percentiles (boxes). Error bars represent the maximum and minimum values; n = 10. *, P < 0.05 compared to results for untreated cells; **, P < 0.01 compared to results for untreated cells; ***, P < 0.001 compared to results for untreated cells.
Splenocytes from C57Bl/6 mice stimulated with ConA produced significantly lower levels of both IFN-γ (P < 0.001) and IL-4 (P < 0.05) when stimulation occurred in the presence of 10 μM OdDHL compared to levels for control cells (Fig. 1). Such differences were not seen when cells were stimulated in the presence of 1 and 0.1 μM OdDHL. Splenocytes from BALB/c mice stimulated with ConA produced significantly lower levels of both IFN-γ (P < 0.001) and IL-4 (P < 0.001) when stimulation occurred in the presence of 10 μM OdDHL compared to levels for control cells (Fig. 2). Similarly, significantly lower levels of both IFN-γ (P < 0.05) and IL-4 (P < 0.01) were seen when cells were stimulated in the presence of 1 μM OdDHL. Such differences were not seen when cells were stimulated in the presence of 0.1 μM OdDHL. Thus, in both strains of mice, OdDHL clearly inhibited production of both IFN-γ and IL-4.
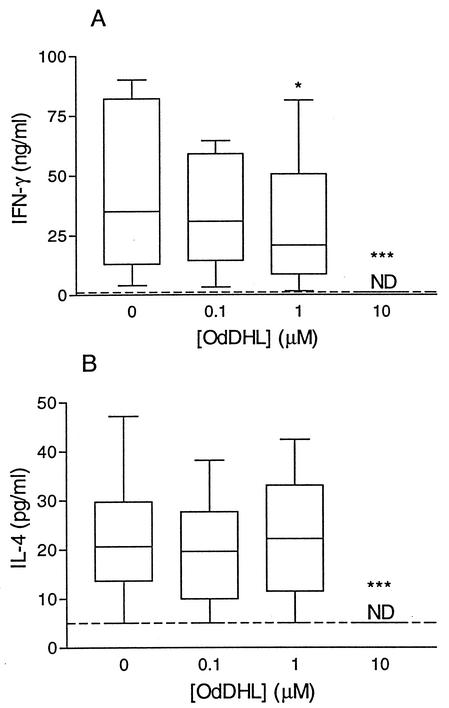
Cytokine production after primary in vitro stimulation of TCR transgenic splenocytes.
Although the mitogen, ConA, used in the above experiments is principally a T-cell mitogen, it was of importance to demonstrate that OdDHL could also affect an antigen-specific T-cell response. However, in normal mice the levels of IFN-γ and IL-4 produced following primary antigen stimulation in vitro is below the limits of detection (data not shown). Thus, in order to confirm that the observed effects of OdDHL on splenocytes stimulated in vitro also applied to antigenic stimulation, splenocytes from TCR transgenic mice expressing a TCR specific for MCC plus MHC class II were stimulated with peptide antigen in the presence or absence of various concentrations of OdDHL. In this model only CD4+ T cells express the transgene and respond to the antigen, so any effect of OdDHL in this model must be on either the transgenic CD4+ T cells or the antigen-presenting cells. In addition, between 50 to 80% of the CD4+ cells express the transgene, which means that cytokine production during a primary response is easily detectable. The results of these experiments are shown in Fig. 3. As with the mitogen-stimulated BALB/c and C57BL/6 splenocytes, the TCR transgenic spleen cells produced significantly lower levels of both IFN-γ (P < 0.001) and IL-4 (P < 0.001) when stimulated in the presence of 10 μM OdDHL compared to levels for cells cultured in the absence of OdDHL. At 1 μM OdDHL, IFN-γ production was significantly inhibited overall (P < 0.05), although the degree of inhibition was very low, and IL-4 production was not significantly inhibited. No inhibition of either IFN-γ or IL-4 was seen when cells were stimulated in the presence of 0.1 μM OdDHL. These data confirm that in vitro antigen-specific cytokine responses are also inhibited by OdDHL and suggest that IFN-γ may be more susceptible to this inhibition than is IL-4.
FIG. 3.
The production of IFN-γ and IL-4 by TCR transgenic splenocytes exposed to OdDHL in vitro. Splenocytes from unimmunized TCR transgenic mice were stimulated with 5 μM MCCT102S and were exposed to various concentrations of OdDHL. An ELISA was used to quantify IFN-γ (A) and IL-4 (B) protein levels following 48 h of incubation. Data are represented as the median ± 25th and 75th percentiles (boxes). Error bars represent the maximum and minimum values. ND, all values below the limit of detection. The dotted line represents the limit of detection for each assay; n = 10. *, P < 0.05 compared to results for untreated cells. ***, P < 0.001 compared to results for untreated cells.
To confirm that this reduction in cytokine production was not due to OdDHL killing cytokine-producing cells, splenocytes incubated in the presence of various concentrations of OdDHL were assayed for induction of cell death. While OdDHL treatment was found to result in some increase in cell death in the overall splenocyte population, minimal effects were seen on CD4+ cells, with the maximum level of cell death seen at 10 μM OdDHL being less than 10% and no significant death occurring at the lower concentrations of 4 and 1 μM OdDHL.
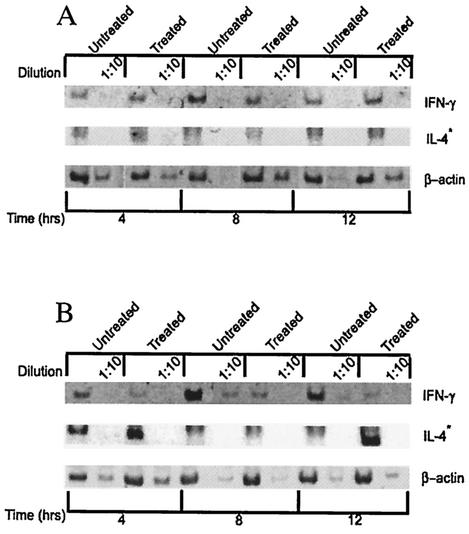
IFN-γ and IL-4 mRNA levels in TCR transgenic mice splenocytes following primary stimulation in vitro.
To determine whether the reduction in cytokine production by TCR transgenic T cells observed in the presence of OdDHL was reflected in the expression of cytokine mRNA, and thus that OdDHL was acting at a stage prior to the secretion of the cytokine, levels of IFN-γ and IL-4 mRNA in antigen-stimulated TCR transgenic spleen cells were assessed. Cells were harvested at 4, 8, and 12 h after antigen stimulation in vitro, and total RNA was extracted and reverse transcribed. For IFN-γ, cDNA was used for PCR either undiluted or at a 1:10 dilution, while IL-4 reverse transcription (RT)-PCR was performed only with undiluted cDNA, as the level of message for this cytokine is much lower than that for IFN-γ. The PCR product band densities were analyzed by using Quantity One, version 4.03, for the Macintosh (Bio-Rad Laboratories). Figure 4 shows the gel analysis results for this experiment and demonstrates a clear reduction in IFN-γ mRNA in cells treated with 4 or 10 μM OdDHL. The RT-PCR was not performed for samples treated with 1 μM OdDHL, as preliminary data indicated that there was no quantifiable reduction in IFN-γ or IL-4 mRNA in these cultures. The comparison of the band intensities of undiluted and 1:10 diluted samples, following normalization to β-actin, suggests that the reduction in the amount of IFN-γ mRNA in the presence of 10 μM OdDHL is of the order of 10-fold at all time points tested. At 4 μM the reduction is still detectable but is of the order of 1.5- to 2-fold. For IL-4 the results demonstrate that mRNA levels, in cells from both control and OdDHL-treated cultures, are very low, and no quantifiable change in IL-4 mRNA was observed. These data confirm that the reduction in IFN-γ protein observed was unlikely to represent an inhibition of secretion or enhanced degradation of the protein in the presence of OdDHL but was more likely to represent an inhibition of induction of mRNA expression. The results of the IL-4 RT-PCR are not informative in this respect, as any reduction in mRNA levels is too small to be quantifiable in the RT-PCR used.
FIG. 4.
Expression of IFN-γ but not IL-4 mRNA is inhibited by OdDHL. TCR transgenic splenocytes were stimulated with antigen, and the cells were harvested at 4, 8, and 12 h poststimulation. Total RNA was extracted and subjected to RT-PCR for β-actin (lower panel), IL-4 (middle panel), and IFN-γ (upper panel). Products were visualized on an 8% polyacrylamide gel. Products were the expected sizes for cDNA. Untreated, control cells stimulated in the absence of OdDHL; treated, cells stimulated in the presence of 4 (A) or 10 μM (B) OdDHL. All cDNA products following RT were either undiluted or diluted 1:10 before undergoing PCR (*, IL-4 results do not include the 1:10 dilution). Results are from one experiment representative of two.
Cytokine production by C57Bl/6 splenocytes after in vivo immunization.
In order to compare the in vitro and in vivo effects of OdDHL on cytokine production by stimulated C57Bl/6 T cells, C57Bl/6 mice were injected with OdDHL following immunization with OVA, and the ability of their splenocytes to respond to both mitogenic and antigenic restimulation in vitro in the absence of OdDHL was analyzed. It should be emphasized that these experiments do not directly measure the ability of splenocytes from treated mice to produce cytokines in vivo, but rather they represent an assessment of the capacity of these cells to respond to in vitro restimulation at selected time points after in vivo treatment. For these experiments, the in vivo dose of OdDHL was calculated on the basis of an estimated blood volume per mouse of 2 ml to reflect as closely as possible the 10 μM concentration that had been demonstrated to have significant effects in vitro. For the same reason, a single injection was used as close as possible to the time of immunization to reflect the in vitro situation where OdDHL was added at the time of antigen or mitogen stimulation. Splenocytes from C57Bl/6 mice immunized with OVA-alum and injected with either OdDHL or control were harvested 2, 4, and 8 days postimmunization and were restimulated in vitro either with mitogen (ConA), in order to analyze the effects of OdDHL on the underlying capacity of the immune response, or with antigen (OVA), in order to analyze the effects of OdDHL on an antigen-specific immune response. Unstimulated cells uniformly produced undetectable levels of IFN-γ and IL-4 (data not shown). Antigen-stimulated cells did not produce detectable levels of either cytokine consistently enough for analysis (data not shown). The results of the ConA stimulation experiments are shown in Fig. 5. In order to facilitate the analysis of the changes in the balance of the Th1 and Th2 responses as a result of OdDHL exposure and to directly compare the effects of OdDHL on both IFN-γ and IL-4 production, results in these experiments are expressed a percentages of the cytokine production of immunized control mice.
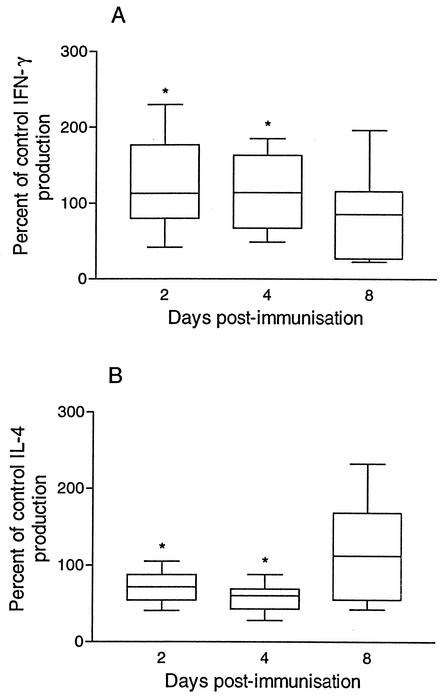
FIG. 5.
Relative production of IFN-γ and IL-4 by C57Bl/6 splenocytes exposed to OdDHL in vivo. Splenocytes from OVA-immunized C57Bl/6 mice, given either an OdDHL or control injection, were stimulated with 5 μg of ConA/ml. An ELISA was used to quantify IFN-γ (A) and IL-4 (B) protein levels following 48 h of incubation. Data are presented as the relative production of each cytokine by splenocytes from mice injected with OdDHL compared to the production of each cytokine by splenocytes from mice injected with control. Data represented as the median ± 25th and 75th percentiles (boxes). Error bars represent the maximum and minimum values; n = 8 to 10. *, P < 0.05 comparing the effect of OdDHL on the production of IFN-γ (A) to the production of IL-4 (B).
Compared to cells from control immunized mice, splenocytes from mice injected with OdDHL produced similar or slightly elevated levels of IFN-γ and lower levels of IL-4 when harvested and restimulated with mitogen at days 2 and 4 after immunization, while those harvested at 8 days after immunization were not different to controls. The differences between control and OdDHL-treated groups at 2 and 4 days postimmunization were found to be statistically significant (P < 0.05) and indicated that, in these Th1-biased C57Bl/6 mice, in vivo treatment with OdDHL caused a transient, relative increase in the expression of the Th1 cytokine IFN-γ over the Th2 cytokine IL-4, thus temporarily accentuating the Th1 nature of the response in these mice. However, the inability to detect cytokine production by splenocytes stimulated with antigen in vitro meant that evaluation of the significance of this effect in C57BL/6 mice in terms of antigen responses was not possible. For this reason, the experiments with BALB/c mice used a higher cell concentration for the in vitro restimulation in an attempt to produce detectable cytokine levels.
Cytokine production by BALB/c splenocytes after in vivo immunization.
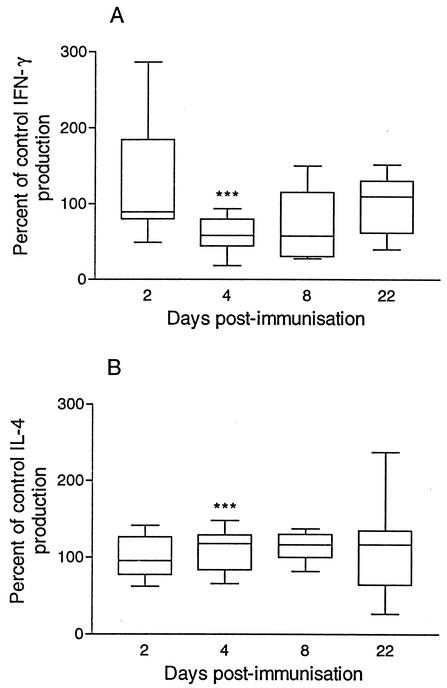
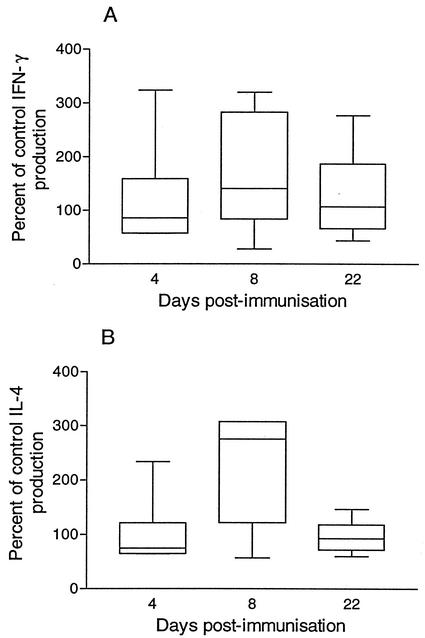
In order to compare the in vitro and in vivo effects of OdDHL on cytokine production by BALB/c T cells, BALB/c mice were injected with OdDHL following immunization, and the ability of their splenocytes to respond to both mitogenic and antigenic restimulation in vitro in the absence of OdDHL was analyzed. These experiments also allowed for the comparison of the effects of in vivo OdDHL exposure to T cells from C57Bl/6 and BALB/c mice. Splenocytes from BALB/c mice immunized with OVA-alum and injected with either OdDHL or control were harvested 2, 4, 8, and 22 days postimmunization and were restimulated with either mitogen (ConA) or antigen (OVA) in vitro. Unstimulated cells uniformly produced undetectable levels of IFN-γ and IL-4 (data not shown). Results of mitogen-stimulated BALB/c splenocyte experiments are shown in Fig. 6. Once again, results for OdDHL-treated mice are expressed as a percentage of those for control mice. Compared to levels of cells from control mice, mitogen-stimulated cells from mice injected with OdDHL produced similar or slightly elevated levels of IL-4 and lower levels of IFN-γ when harvested 4 or 8 days after immunization, while levels of those harvested at 2 or 22 days postimmunization were similar to those of controls. These differences were found to be statistically significant at 4 days (P < 0.001) but not at 8 days. Thus, in contrast to the effect observed with C57Bl/6 mice, the effect of OdDHL on mitogen-induced responses in Th2-biased BALB/c mice was to transiently increase the bias towards Th2 cytokine production. In order to determine whether this was also true for antigen-stimulated cytokine production, cells from these OVA-immunized BALB/c mice were restimulated with antigen in vitro. These experiments were performed at a higher cell concentration than that for the C57Bl/6 mice solely in an attempt to obtain detectable cytokine production. Preliminary experiments comparing cytokine production by BALB/c spleen cells at the two concentrations suggested that this increase in cell concentration led to an increased level of IFN-γ, and to a lesser extent IL-4, in these cultures (data not shown). However, this change does not affect the interpretation of the data indicating no significant modification of OdDHL-treated animals as opposed to control animals. Splenocytes harvested 2 days postimmunization from either OdDHL or control mice and stimulated with antigen in vitro produced undetectable levels of both IFN-γ and IL-4 (data not shown). Splenocytes harvested at later times from mice injected with OdDHL produced similar levels of both cytokines as control mice, although splenocytes harvested from mice injected with OdDHL 8 days postimmunization produced higher levels of both cytokines than control mice (Fig. 7). Although IL-4 production appeared to be elevated more than IFN-γ production, suggesting a trend towards a more Th2-like response, these differences were not found to be statistically significant. Thus, while there is a suggestion that the effect of OdDHL on an antigen-specific response in these mice is to favor a more Th2-like effect, it was not possible to confirm this by using in vitro restimulation of T cells. For this reason, we examined the in vivo OVA-specific antibody responses in these mice.
FIG. 6.
The relative production of IFN-γ and IL-4 by ConA-stimulated BALB/c splenocytes exposed to OdDHL in vivo. Splenocytes from OVA-immunized BALB/c mice, given either an OdDHL or control injection, were stimulated with 5 μg of ConA/ml. An ELISA was used to quantify IFN-γ (A) and IL-4 (B) protein levels following 48 h of incubation. Data are presented as the relative production of each cytokine by splenocytes from mice injected with OdDHL compared to the production of each cytokine by splenocytes from mice injected with control. Data are represented as the median ± 25th and 75th percentiles (boxes). Error bars represent the maximum and minimum values; n = 7 to 10. ***, P < 0.001 comparing the effect of OdDHL on the production of IFN-γ (A) to the production of IL-4 (B).
FIG. 7.
The relative production of IFN-γ and IL-4 by OVA-stimulated BALB/c splenocytes exposed to OdDHL in vivo. Splenocytes from OVA-immunized BALB/c mice, given either an OdDHL or control injection, were stimulated with 200 μg of OVA/ml. An ELISA was used to quantify IFN-γ (A) and IL-4 (B) protein levels following 48 h of incubation. Data are presented as the relative production of each cytokine by splenocytes from mice injected with OdDHL compared to the production of each cytokine by splenocytes from mice injected with control. Data are represented as the median ± 25th and 75th percentiles (boxes). Error bars represent the maximum and minimum values; n = 8 to 10.
OVA-specific antibody responses in BALB/c mice.
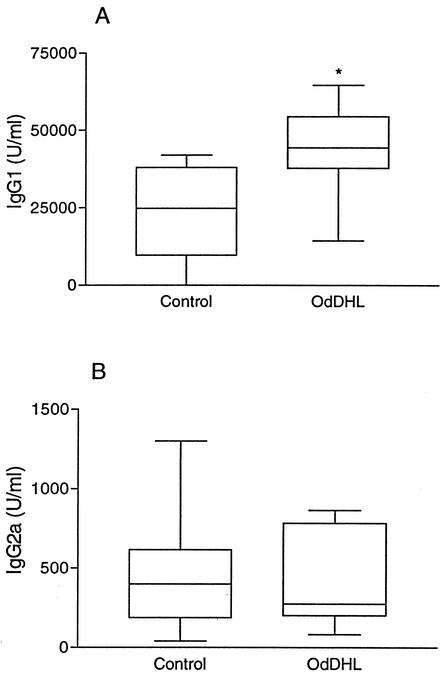
Because the relatively minor changes in cytokine production following mitogen stimulation and the nonsignificant changes following antigen stimulation of cells from immunized C57Bl/6 and BALB/c mice (Fig. 5, 6, and 7) could be argued to be of little relevance to a model of an in vivo antigen-specific immune response, we elected to measure a true in vivo response: the antibody response to the protein antigen OVA. The relative levels of IgG1 (Th2-associated) and IgG2a (Th1-associated) OVA-specific antibodies were characterized as a measure of the relative Th2 or Th1 nature of the response. This experiment was carried out only in BALB/c mice, since it has been established that C57Bl/6 mice are genetically incapable of producing significant amounts of the Th1-associated antibody subclass IgG2a (23). Serum from OVA-immunized, OdDHL-treated or control mice was collected 22 days postimmunization and was analyzed for levels of both OVA-specific IgG1 and OVA-specific IgG2a by subclass-specific ELISA. All serum taken prior to immunization was found to contain undetectable levels of OVA-specific IgG1 and IgG2a (data not shown). Twenty-two days postimmunization it was clear that OdDHL injection caused an approximate doubling in the levels of OVA-specific IgG1 produced (P < 0.05) while causing a slight but not significant decrease in the median level of OVA-specific IgG2a (Fig. 8). Thus, OdDHL has clearly caused a significant shift of the OVA-specific antibody response towards an IgG1 (Th2) response rather than an IgG2a (Th1) response, suggesting that the changes seen in cytokine production by splenocytes from OVA-immunized BALB/c mice reflect an in vivo change powerful enough to modulate the makeup of an immune response.
FIG. 8.
The production of IgG1 and IgG2a by OVA-immunized BALB/c mice injected with OdDHL. Serum from OVA-immunized BALB/c mice, given either an OdDHL or control injection, was collected, and an ELISA was used to quantify OVA-specific IgG1 (A) and IgG2a (B) levels. Data are represented as the median ± 25th and 75th percentiles (boxes). Error bars represent the maximum and minimum values; n = 7 to 10. *, P < 0.05 compared to results for untreated mice.
DISCUSSION
This study is the first to demonstrate a direct effect of OdDHL on an in vivo antigen-specific immune response, the production of antibody to the protein antigen OVA. OdDHL treatment of BALB/c mice in vivo was found to increase the titer of OVA-specific IgG1, a Th2-associated antibody subclass, while having no significant effect on the levels of OVA-specific IgG2a, a Th1-associated antibody (Fig. 8). In addition, our results demonstrate a modulation of the ratio of production of the Th1 cytokine IFN-γ and the Th2 cytokine IL-4 following in vivo exposure to OdDHL during an immune response. This modulation was seen to cause a relative increase in IFN-γ production by mitogen-stimulated splenocytes from Th1-biased C57Bl/6 mice while causing a relative increase in IL-4 production by mitogen-stimulated splenocytes from Th2-biased BALB/c mice. These results suggest that OdDHL is acting in vivo to accentuate the underlying immune response bias of the host rather than specifically promoting either Th1 or Th2 responses and would suggest that if it were possible to evaluate the ratio of OVA-specific IgG1 to IgG2a in C57Bl/6 mice (23), that this would be biased towards the Th1-linked isotype. This modulation of an underlying tendency to either Th1 or Th2 responsiveness has the potential to lead to a very strong inflammatory or humoral response, depending on the mouse strain studied. If this were the case, it would imply that OdDHL immunomodulation could play a variable role in P. aeruginosa-related disease. The cumulative results from a variety of P. aeruginosa infection models suggest that rather than one or the other of Th1 or Th2 responses to P. aeruginosa being detrimental to the host, very biased immune responses, either inflammatory or humoral, are associated with worsening disease prognosis (14, 18, 26-29, 41). Thus, an increased polarization of the response by OdDHL could potentially increase the survival of the bacteria and worsen the outcome of the infection.
The hypothesis that OdDHL is acting to accentuate the underlying immune bias of the host rather than uniformly promoting a Th1 or Th2 type response goes some way to reconciling differences in previously reported results on the immunomodulatory properties of OdDHL. The original report of immunomodulation by OdDHL by Telford et al. (51) demonstrated an inhibition in production of the Th1 cytokines TNF-α and IL-12 by murine peritoneal macrophages from BALB/c mice stimulated with LPS in vitro and an increase in the production of IgG1 by murine splenocytes undergoing secondary stimulation in an in vitro model of antibody production. The effect of OdDHL on IL-12 production in Telford's report (51) appeared to occur at concentrations much lower than those which affected TNF-α and much lower than those we have shown to inhibit IL-4 and IFN-γ production, suggesting that another component of the variable observations in different models could be changes in the relative production of cytokines at different concentrations of OdDHL and by different cell types, since IL-12 is primarily produced by macrophages. The amount of OdDHL used in our in vivo treatments was calculated to be in the 1 to 10 μM range, where effects were observed in vitro, but it is certainly possible that the effective concentration was lower than this. This could affect the overall outcome and could contribute to differences between the in vivo and in vitro observations.
A more recent report that suggested that OdDHL could promote a Th1-type response in C57Bl/6 mice through its induction of inflammation and numerous inflammatory mediators, including several chemokines, the cytokines IL-1α and IL-6, and the inflammatory mediator cyclooxygenase-2 (47), is also consistent with our hypothesis that OdDHL accentuates an underlying immune response bias. The only report inconsistent with this hypothesis is a study that used OVA-specific TCR transgenic mice on a BALB/c background, which showed increased production of IFN-γ by splenic T cells after secondary antigen stimulation in vitro following exposure to OdDHL during primary in vitro stimulation (47). Preliminary experiments in our laboratory with the MCC-specific TCR transgenic mice have been unable to replicate these data (results not shown), but this study is continuing.
The results of the present study show a contrast between results of in vitro stimulation of spleen cells in the presence of OdDHL and those observed following in vivo immunization in the presence of OdDHL followed by in vitro restimulation in the absence of OdDHL. While injection of OdDHL into mice in vivo tended to further accentuate the underlying immune response of the mouse strain during subsequent in vitro stimulation, our results demonstrate that in vitro exposure to OdDHL had a suppressive effect on both IFN-γ and IL-4 protein secretion by mitogen and antigen stimulation of splenocytes from at least three different strains of mice (Fig. 1, 2, and 3). As discussed earlier, this may be in part due to differences in the effective concentration of OdDHL in the two models. For example, AHLs can variably undergo hydrolysis under conditions of pH and temperature that may be differentially applicable to different experimental systems (55). Additionally, anecdotal evidence suggests that OdDHL does not move freely through body fluids, so compartmentalization of OdDHL in vivo may lead to differences in effective concentration at different sites. However, evidence that P. aeruginosa strains that do not produce OdDHL are less virulent in vivo (35, 53) and that OdDHL is detectable in the lungs of P. aeruginosa-colonized cystic fibrosis patients (8, 9, 25) indicates that OdDHL is able to function in vivo. Other complicating factors of the in vivo experiments are the potential for OdDHL to be acting on cell types other than the T cells and antigen-presenting cells present in the in vitro cultures and the reported instability of OdDHL under physiological conditions (55). For example, there are reports of OdDHL affecting the function of cell types as diverse as vascular smooth muscle cells (13, 20), epithelial cells (7, 46, 47), and fibroblasts (46, 48), all of which could be involved in an in vivo model, as well as the immune cells present in the in vitro model systems (47, 51). In addition, some effects of OdDHL appear to depend on the context in which cells are studied. Two studies carried out by the same group looking at the cardiovascular effects of OdDHL found that in an in vitro model examining porcine arterial smooth muscle cells, OdDHL inhibited contraction, but that in an in vivo rat model it caused a slowing of the heart rate and some signs of vasoconstriction (13, 20).
A further point arising from our studies is that the differences observed between the effects of OdDHL in vitro and in vivo suggest strongly that caution should be taken when applying experimental results to disease models of P. aeruginosa infection, where not only is OdDHL acting in vivo but where its effects may be compounded by other bacterial products which affect the immune system, particularly LPS.
The observation that IFN-γ mRNA expression was reduced in antigen-stimulated TCR transgenic splenocytes treated with OdDHL strongly suggests that the effects of OdDHL on mitogen- or antigen-stimulated cytokine production are unlikely to be due only to degradation of cytokine protein or to inhibition of cytokine secretion, although the semiquantitative nature of the RT-PCR data as well as the lack of evidence of reduction in IL-4 mRNA means this cannot be entirely ruled out as a contributing factor. However, it seems likely that the effects of OdDHL are at least partly due to a mechanism involving inhibition of a step prior to the transcription of cytokine mRNA. This could include effects on antigen-presenting cells, which indirectly affect T-cell activation, or possibly one or more steps in the transduction of the signal from the T-cell antigen receptor to the nucleus. To date there have been no studies reporting the mechanism of action of OdDHL in antigen-specific immune responses, although Smith et al. (46), in a study reporting induction of IL-8 production in the respiratory epithelial cell lines 16HBE and A549, indicated that OdDHL was inducing IL-8 production through activation of the transcriptional regulators NF-κB and activator protein 2 via a mitogen-activated protein kinase-dependent pathway. These data are in contrast to a report by Palfreyman et al. (33), which showed no induction by OdDHL of IL-8 production by A549 cells. Smith et al. (48) have also demonstrated that OdDHL induces prostaglandin E2 expression by L828 cells via an NF-κB-dependent mechanism. These data indicate that in these cell lines, OdDHL is inducing inflammatory mediators through activation of NF-κB. However, the results of our study, in which in vitro IFN-γ production was inhibited in the presence of OdDHL, suggest that it is unlikely that OdDHL is activating NF-κB-dependent pathways in T cells, since such activation is associated with increased transcription and production of inflammatory mediators, such as IFN-γ (43, 44). It should be kept in mind that due to the differences in the isoforms (3, 4, 10), methods of activation (32), and transcriptional regulation (32) of NF-κB in different cell types, results obtained with other cell types can only be extrapolated to T cells with caution.
The broad range of effects of OdDHL on different types of mammalian cells, combined with the range of immunomodulatory effects reported for OdDHL, suggest that it is most probably acting either through a specific target that is ubiquitous to many cell types, such as NF-κB or an NF-κB-dependent pathway, or that OdDHL is in fact interacting with a range of different targets. For example, it is possible that OdDHL interferes with a range of cell surface receptors on different cell types. It is also a possibility that the wide-ranging effects of OdDHL are due to its being able to interact with a variety of cellular components from different cell types and that this is why there have been apparent discrepancies in results reported by different groups. Thus, while the only mechanism proposed to date for OdDHL action on mammalian cells comes from Smith et al. (47), who implicate NF-κB-mediated signal transduction pathways, there is no evidence that OdDHL is directly interacting with NF-κB, and the molecular target(s) of OdDHL action remains unknown.
Overall, the results of the study reported here suggest that while OdDHL can have immunomodulatory activities in vivo, the exact nature of these effects may be dependent on the underlying immune status of the host. Significantly, our results also demonstrate that OdDHL has very different in vivo and in vitro effects on cytokine production, which has important implications for extrapolating in vitro results to models of P. aeruginosa infection. These results provide a basis for partially reconciling reports of contrasting effects of OdDHL on markers of the Th1 and Th2 responses in murine models. While our study provides no direct evidence as to the mechanism through which OdDHL is acting on T cells, it seems unlikely that it is by activating NF-κB, as has been reported for some other cell types. We hypothesize that either the target of OdDHL action is a molecule or pathway common to numerous cell types whose effects differ depending on the cell type studied or that OdDHL is interacting with mammalian cells in a nonspecific manner to modulate the innate capacities of those cells. Studies to distinguish these possibilities are continuing.
Acknowledgments
We thank Naresh Kumar, School of Chemical Sciences, The University of New South Wales, for the synthesis of OdDHL and Barbara Fazekas de St. Groth, Centenary Institute for Cancer Biology and Medicine, for providing homozygous TCR transgenic mice breeding pairs.
This work was supported by funding from The University of New South Wales.
Editor: F. C. Fang
REFERENCES
- 1.Afessa, B., and B. Green. 2000. Bacterial pneumonia in hospitalized patients with HIV infection. Chest 117:1017-1022. [DOI] [PubMed] [Google Scholar]
- 2.Bycroft, B. W., D. I. Pritchard, S. R. Chhabra, and D. Hooi. October 2001. Preparation of immunosuppressant N-acyl homoserine lactones. PCT International Application Patent WO 0174801.
- 3.Carrasco, D., R. P. Ryseck, and R. Bravo. 1993. Expression of relB transcripts during lymphoid organ development: specific expression in dendritic antigen-presenting cells. Development 118:1221-1231. [DOI] [PubMed] [Google Scholar]
- 4.Carrasco, D., F. Weih, and R. Bravo. 1994. Developmental expression of the mouse c-rel proto-oncogene in hematopoietic organs. Development 120:2991-3004. [DOI] [PubMed] [Google Scholar]
- 5.Cherwinski, H. M., J. H. Schumacher, K. D. Brown, and T. R. Mosmann. 1987. Two types of mouse helper T cell clone. III. Further differences in lymphokine synthesis between Th1 and Th2 clones revealed by RNA hybridization, functionally monospecific bioassays, and monoclonal antibodies. J. Exp. Med. 166:1229-1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Darville, T., C. W. Andrews, Jr., J. D. Sikes, P. L. Fraley, L. Braswell, and R. G. Rank. 2001. Mouse strain-dependent chemokine regulation of the genital tract T helper cell type 1 immune response. Infect. Immun. 69:7419-7424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DiMango, E., H. J. Zar, R. Bryan, and A. Prince. 1995. Diverse Pseudomonas aeruginosa gene products stimulate respiratory epithelial cells to produce interleukin-8. J. Clin. Investig. 96:2204-2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Erickson, D. L., R. Endersby, A. Kirkham, K. Stuber, D. D. Vollman, H. R. Rabin, I. Mitchell, and D. G. Storey. 2002. Pseudomonas aeruginosa quorum-sensing systems may control virulence factor expression in the lungs of patients with cystic fibrosis. Infect. Immun. 70:1783-1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Favre-Bonte, S., J. C. Pache, J. Robert, D. Blanc, J. C. Pechere, and C. van Delden. 2002. Detection of Pseudomonas aeruginosa cell-to-cell signals in lung tissue of cystic fibrosis patients. Microb. Pathog. 32:143-147. [DOI] [PubMed] [Google Scholar]
- 10.Feuillard, J., M. Korner, A. Israel, J. Vassy, and M. Raphael. 1996. Differential nuclear localization of p50, p52, and RelB proteins in human accessory cells of the immune response in situ. Eur. J. Immunol. 26:2547-2551. [DOI] [PubMed] [Google Scholar]
- 11.Fuqua, C., and S. C. Winans. 1996. Conserved cis-acting promoter elements are required for density-dependent transcription of Agrobacterium tumefaciens conjugal transfer genes. J. Bacteriol. 178:435-440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gambello, M. J., S. Kaye, and B. H. Iglewski. 1993. LasR of Pseudomonas aeruginosa is a transcriptional activator of the alkaline protease gene (apr) and an enhancer of exotoxin A expression. Infect. Immun. 61:1180-1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gardiner, S. M., S. R. Chhabra, C. Harty, P. Williams, D. I. Pritchard, B. W. Bycroft, and T. Bennett. 2001. Haemodynamic effects of the bacterial quorum sensing signal molecule, N-(3-oxododecanoyl)-L-homoserine lactone, in conscious, normal and endotoxaemic rats. Br. J. Pharmacol. 133:1047-1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gosselin, D., J. DeSanctis, M. Boule, E. Skamene, C. Matouk, and D. Radzioch. 1995. Role of tumor necrosis factor alpha in innate resistance to mouse pulmonary infection with Pseudomonas aeruginosa. Infect. Immun. 63:3272-3278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hutchison, M. L., and J. R. Govan. 1999. Pathogenicity of microbes associated with cystic fibrosis. Microbes Infect. 1:1005-1014. [DOI] [PubMed] [Google Scholar]
- 16.Jones, S., B. Yu, N. J. Bainton, M. Birdsall, B. W. Bycroft, S. R. Chhabra, A. J. Cox, P. Golby, P. J. Reeves, and S. Stephens. 1993. The lux autoinducer regulates the production of exoenzyme virulence determinants in Erwinia carotovora and Pseudomonas aeruginosa. EMBO J. 12:2477-2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kielhofner, M., R. L. Atmar, R. J. Hamill, and D. M. Musher. 1992. Life-threatening Pseudomonas aeruginosa infections in patients with human immunodeficiency virus infection. Clin. Infect. Dis. 14:403-411. [DOI] [PubMed] [Google Scholar]
- 18.Kondratieva, T. K., N. V. Kobets, S. V. Khaidukov, V. V. Yeremeev, I. V. Lyadova, A. S. Apt, M. F. Tam, and M. M. Stevenson. 2000. Characterization of T cell clones derived from lymph nodes and lungs of Pseudomonas aeruginosa-susceptible and resistant mice following immunization with heat-killed bacteria. Clin. Exp. Immunol. 121:275-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lambrecht, B. N., R. A. Pauwels, and B. Fazekas de St. Groth. 2000. Induction of rapid T cell activation, division, and recirculation by intratracheal injection of dendritic cells in a TCR transgenic model. J. Immunol. 164:2937-2946. [DOI] [PubMed] [Google Scholar]
- 20.Lawrence, R. N., W. R. Dunn, B. Bycroft, M. Camara, S. R. Chhabra, P. Williams, and V. G. Wilson. 1999. The Pseudomonas aeruginosa quorum-sensing signal molecule, N-(3-oxododecanoyl)-L-homoserine lactone, inhibits porcine arterial smooth muscle contraction. Br. J. Pharmacol. 128:845-848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lyczak, J. B., C. L. Cannon, and G. B. Pier. 2000. Establishment of Pseudomonas aeruginosa infection: lessons from a versatile opportunist. Microbes Infect. 2:1051-1060. [DOI] [PubMed] [Google Scholar]
- 22.Lyczak, J. B., C. L. Cannon, and G. B. Pier. 2002. Lung infections associated with cystic fibrosis. Clin. Microbiol. Rev. 15:194-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin, R. M., J. L. Brady, and A. M. Lew. 1998. The need for IgG2c specific antiserum when isotyping antibodies from C57BL/6 and NOD mice. J. Immunol. Methods 212:187-192. [DOI] [PubMed] [Google Scholar]
- 24.McManus, A. T., A. D. Mason, Jr., W. F. McManus, and B. A. Pruitt, Jr. 1985. Twenty-five year review of Pseudomonas aeruginosa bacteremia in a burn center. Eur. J. Clin. Microbiol. 4:219-223. [DOI] [PubMed] [Google Scholar]
- 25.Middleton, B., H. C. Rodgers, M. Camara, A. J. Knox, P. Williams, and A. Hardman. 2002. Direct detection of N-acylhomoserine lactones in cystic fibrosis sputum. FEMS Microbiol. Lett. 207:1-7. [DOI] [PubMed] [Google Scholar]
- 26.Morissette, C., C. Francoeur, C. Darmond-Zwaig, and F. Gervais. 1996. Lung phagocyte bactericidal function in strains of mice resistant and susceptible to Pseudomonas aeruginosa. Infect. Immun. 64:4984-4992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morissette, C., E. Skamene, and F. Gervais. 1995. Endobronchial inflammation following Pseudomonas aeruginosa infection in resistant and susceptible strains of mice. Infect. Immun. 63:1718-1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moser, C., H. P. Hougen, Z. Song, J. Rygaard, A. Kharazmi, and N. Hoiby. 1999. Early immune response in susceptible and resistant mice strains with chronic Pseudomonas aeruginosa lung infection determines the type of T-helper cell response. APMIS 107:1093-1100. [DOI] [PubMed] [Google Scholar]
- 29.Moser, C., H. K. Johansen, Z. Song, H. P. Hougen, J. Rygaard, and N. Hoiby. 1997. Chronic Pseudomonas aeruginosa lung infection is more severe in Th2 responding BALB/c mice compared to Th1 responding C3H/HeN mice. APMIS 105:838-842. [PubMed] [Google Scholar]
- 30.Mosmann, T. R., H. Cherwinski, M. W. Bond, M. A. Giedlin, and R. L. Coffman. 1986. Two types of murine helper T cell clone. I. Definition according to profiles of lymphokine activities and secreted proteins. J. Immunol. 136:2348-2357. [PubMed] [Google Scholar]
- 31.Overbergh, L., D. Valckx, M. Waer, and C. Mathieu. 1999. Quantification of murine cytokine mRNAs using real time quantitative reverse transcriptase PCR. Cytokine 11:305-312. [DOI] [PubMed] [Google Scholar]
- 32.Pahl, H. L. 1999. Activators and target genes of Rel/NF-κB transcription factors. Oncogene 18:6853-6866. [DOI] [PubMed] [Google Scholar]
- 33.Palfreyman, R. W., M. L. Watson, C. Eden, and A. W. Smith. 1997. Induction of biologically active interleukin-8 from lung epithelial cells by Burkholderia (Pseudomonas) cepacia products. Infect. Immun. 65:617-622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Passador, L., J. M. Cook, M. J. Gambello, L. Rust, and B. H. Iglewski. 1993. Expression of Pseudomonas aeruginosa virulence genes requires cell-to-cell communication. Science 260:1127-1130. [DOI] [PubMed] [Google Scholar]
- 35.Pearson, J. P., M. Feldman, B. H. Iglewski, and A. Prince. 2000. Pseudomonas aeruginosa cell-to-cell signaling is required for virulence in a model of acute pulmonary infection. Infect. Immun. 68:4331-4334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pearson, J. P., K. M. Gray, L. Passador, K. D. Tucker, A. Eberhard, B. H. Iglewski, and E. P. Greenberg. 1994. Structure of the autoinducer required for expression of Pseudomonas aeruginosa virulence genes. Proc. Natl. Acad. Sci. USA 91:197-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pearson, J. P., E. C. Pesci, and B. H. Iglewski. 1997. Roles of Pseudomonas aeruginosa las and rhl quorum-sensing systems in control of elastase and rhamnolipid biosynthesis genes. J. Bacteriol. 179:5756-5767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rastegar Lari, A., and R. Alaghehbandan. 2000. Nosocomial infections in an Iranian burn care center. Burns 26:737-740. [DOI] [PubMed] [Google Scholar]
- 39.Rastegar Lari, A., H. Bahrami Honar, and R. Alaghehbandan. 1998. Pseudomonas infections in Tohid Burn Center, Iran. Burns 24:637-641. [DOI] [PubMed] [Google Scholar]
- 40.Rogers, P. R., and M. Croft. 1999. Peptide dose, affinity, and time of differentiation can contribute to the Th1/Th2 cytokine balance. J. Immunol. 163:1205-1213. [PubMed] [Google Scholar]
- 41.Sapru, K., P. K. Stotland, and M. M. Stevenson. 1999. Quantitative and qualitative differences in bronchoalveolar inflammatory cells in Pseudomonas aeruginosa-resistant and -susceptible mice. Clin. Exp. Immunol. 115:103-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scott, P. 1991. IFN-gamma modulates the early development of Th1 and Th2 responses in a murine model of cutaneous leishmaniasis. J. Immunol. 147:3149-3155. [PubMed] [Google Scholar]
- 43.Sica, A., L. Dorman, V. Viggiano, M. Cippitelli, P. Ghosh, N. Rice, and H. A. Young. 1997. Interaction of NF-κB and NFAT with the interferon-gamma promoter. J. Biol. Chem. 272:30412-30420. [DOI] [PubMed] [Google Scholar]
- 44.Sica, A., T. H. Tan, N. Rice, M. Kretzschmar, P. Ghosh, and H. A. Young. 1992. The c-rel protooncogene product c-Rel but not NF-kappa B binds to the intronic region of the human interferon-gamma gene at a site related to an interferon-stimulable response element. Proc. Natl. Acad. Sci. USA 89:1740-1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Silvestre, J. F., and M. I. Betlloch. 1999. Cutaneous manifestations due to Pseudomonas infection. Int. J. Dermatol. 38:419-431. [DOI] [PubMed] [Google Scholar]
- 46.Smith, R. S., E. R. Fedyk, T. A. Springer, N. Mukaida, B. H. Iglewski, and R. P. Phipps. 2001. IL-8 production in human lung fibroblasts and epithelial cells activated by the Pseudomonas autoinducer N-3-oxododecanoyl homoserine lactone is transcriptionally regulated by NF-kappa B and activator protein-2. J. Immunol. 167:366-374. [DOI] [PubMed] [Google Scholar]
- 47.Smith, R. S., S. G. Harris, R. Phipps, and B. Iglewski. 2002. The Pseudomonas aeruginosa quorum-sensing molecule N-(3-oxododecanoyl)homoserine lactone contributes to virulence and induces inflammation in vivo. J. Bacteriol. 184:1132-1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Smith, R. S., R. Kelly, B. H. Iglewski, and R. P. Phipps. 2002. The Pseudomonas autoinducer N-(3-oxododecanoyl) homoserine lactone induces cyclooxygenase-2 and prostaglandin E2 production in human lung fibroblasts: implications for inflammation. J. Immunol. 169:2636-2642. [DOI] [PubMed] [Google Scholar]
- 49.Still, J., T. Newton, B. Friedman, S. Furhman, E. Law, and J. Dawson. 2000. Experience with pneumonia in acutely burned patients requiring ventilator support. Am. Surgeon 66:206-209. [PubMed] [Google Scholar]
- 50.Sun, B., L. V. Rizzo, S. H. Sun, C. C. Chan, B. Wiggert, R. L. Wilder, and R. R. Caspi. 1997. Genetic susceptibility to experimental autoimmune uveitis involves more than a predisposition to generate a T helper-1-like or a T helper-2-like response. J. Immunol. 159:1004-1011. [PubMed] [Google Scholar]
- 51.Telford, G., D. Wheeler, P. Williams, P. T. Tomkins, P. Appleby, H. Sewell, G. S. Stewart, B. W. Bycroft, and D. I. Pritchard. 1998. The Pseudomonas aeruginosa quorum-sensing signal molecule N-(3-oxododecanoyl)-l-homoserine lactone has immunomodulatory activity. Infect. Immun. 66:36-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Whiteley, M., K. M. Lee, and E. P. Greenberg. 1999. Identification of genes controlled by quorum sensing in Pseudomonas aeruginosa. Proc. Natl. Acad. Sci. USA 96:13904-13909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu, H., Z. Song, M. Givskov, G. Doring, D. Worlitzsch, K. Mathee, J. Rygaard, and N. Hoiby. 2001. Pseudomonas aeruginosa mutations in lasI and rhlI quorum sensing systems result in milder chronic lung infection. Microbiology 147:1105-1113. [DOI] [PubMed] [Google Scholar]
- 54.Yang, X., K. T. HayGlass, and R. C. Brunham. 1996. Genetically determined differences in IL-10 and IFN-gamma responses correlate with clearance of Chlamydia trachomatis mouse pneumonitis infection. J. Immunol. 156:4338-4344. [PubMed] [Google Scholar]
- 55.Yates, E. A., B. Philipp, C. Buckley, S. Atkinson, S. R. Chhabra, R. E. Sockett, M. Goldner, Y. Dessaux, M. Camara, H. Smith, and P. Williams. 2002. N-acylhomoserine lactones undergo lactonolysis in a pH-, temperature-, and acyl chain length-dependent manner during growth of Yersinia pseudotuberculosis and Pseudomonas aeruginosa. Infect. Immun. 70:5635-5646. [DOI] [PMC free article] [PubMed] [Google Scholar]