Abstract
Background
The typical lesion of focal nodular hyperplasia (FNH) is a benign tumor-like mass characterized by hepatocytic nodules separated by fibrous bands. The solitary central artery with high flow and the absent portal vein give the lesions their characteristic radiological appearance. The great majority of cases seen in daily practice conform to the above description. Additional small nodules (from 1-2 up to 15-20 mm in diameter) detected by imaging techniques or on macroscopic examination may be difficult to identify as representing FNH if they lack the key features of FNH as defined in larger lesions. The aim of this study was to characterize these small nodules, and to compare their characteristics with those of typical lesions of FNH present in the same specimens.
Results
Eight patients underwent hepatic resections for the removal of a mass lesion ("nodule") diagnosed as: FNH (1 patient); nodules of unknown nature (5 patients); or nodules thought to be adenoma or hepatocellular carcinoma (2 patients). Six nodules out of 9 discovered by imaging techniques met histopathological criteria for the diagnosis of typical FNH, at least in parts of the nodule; 2 nodules corresponded to a minor form of FNH ("subtle FNH") and one nodule to a steatotic area. Although FNH was thought to be found in a normal or nearly normal liver, this study revealed that, in addition, there were various types of small FNH-like nodules and vascular abnormalities in the liver with typical FNH nodule. The various types of small FNH-like nodules (n = 8, diameter 2 to 20 mm) consisted of the association to various degrees of numerous and/or enlarged arteries in portal tracts or in septa, with hyperplastic foci, slight ductular reaction, and regions of sinusoidal dilatation, accompanied by thin fibrous bands. Vascular abnormalities consisted of unpaired arteries, portal tracts with arteries larger than the associated bile duct, and regions of sinusoidal dilatation.
Conclusions
Although these small nodules can be considered as insufficient type or abortive forms of FNH, or adenoma, they can be precursors of the large mass lesions in which FNH was recognized and defined.
Background
The typical lesion of focal nodular hyperplasia (FNH) is a benign tumor-like mass characterized by hepatocytic nodules separated by fibrous bands. The mass has a central stellate fibrous region containing malformed vascular structures that include large arteries but, as a rule, without portal veins. The component nodules consist of nearly normal hepatocytes arranged in plates 1 to 2 cells thick. A more or less prominent bile ductular reaction is usually found at the interface between hepatocytes and fibrous bands. It is thought that increased arterial flow [1,2] hyperperfuses the local parenchyma leading to secondary hepatocellular hyperplasia [3]. FNH is therefore considered a hyperplastic rather than a neoplastic process. The solitary central artery with high flow and the absent portal vein give the lesions their characteristic radiological appearance [4-6].
The great majority of cases seen in daily practice conform to the above description [7]. Additional small nodules (from 1–2 up to 15–20 mm in diameter) detected by imaging techniques or on macroscopic examination may be difficult to identify as representing FNH if they lack the key features of FNH as defined in larger lesions.
The aim of this study was to characterize these small nodules, and to compare their characteristics with those of typical lesions of FNH present in the same specimens.
Results
The main relevant pathological data are presented in Tables 1 and 2.
Table 1.
Data of nodules
| Cases | Imaging techniques (results) | Total number of nodules (imaging + slicing): size / aspect | Histological diagnosis |
| 1 | a: 2.5 cm nodule (LL), FNH b: 1.5 cm adjacent triangular lesion c: not detected d: not detected | a: 2.5 cm, aspect of FNH b: 1.5 cm / yellow c: 5 mm / yellow d: 2 mm / yellow | a: FNH (typical) b: steatotic nodule (type 1–2 lesion) c: steatotic nodule (type 2–3 lesion) d: steatotic nodule (type 2–3 lesion) |
| 2 | a: 2.5 cm nodule (LL) probable adenoma | a: nodule difficult to identify from the surrounding tissue | a: partly type 2–3 lesion, partly subtle FNH (type 4 lesion) |
| 3 | a: 6 cm nodule (RL), FNH or adenoma b: not detected | a: 6 cm, aspect of FNH b: 5 mm whitish nodule | a: FNH (typical) b: dilatation of thin wall vessels (type 1 lesion) |
| 4 | a: 4 cm nodule (LL), probable adenoma b: not detected | a: 4 cm, aspect of FNH b: 1 × 2 cm whitish nodule | a: FNH (typical and telangiectatic type) b: type 2, 3, 4 lesions |
| 5 | a: 3.5 cm nodule (III and IV), adenoma or HCC b: not detected c: not detected d: not detected | a: 3.5 cm, aspect of FNH b: 1.5 cm c: 3 mm yellow d: 2 mm hemorrhagic | a: FNH (typical but steatotic) b: FNH (typical but steatotic) c: type 3 lesions d: dilatation of thin wall vessels (type 1 lesion) |
| 6 | a: 3 cm nodule (VIII), adenoma or FNH | a: 3 cm, aspect of FNH | a: typical FNH with type 2–3 lesion at the periphery |
| 7 | a: 7 cm nodule (V, VI), FNH b: not detected | a: 7 cm, aspect of FNH b: 1.1 × 1.8 cm pale | a: FNH (typical) b: steatotic (type 3 lesion) |
| 8 | a: 2 cm nodule (V, VI), suspicion of HCC | a: 2 cm, aspect of FNH | a: subtle FNH (type 4 lesion) with type 2–3 lesion at the periphery |
Cases 1 to 7 are women. Letters a, b, c, d identify different nodules for a same case. Roman numbers indicate the segments of the liver. LL: left lobe; RL: right lobe.
Table 2.
Data of cases
| Cases | Age | Discovery | Other findings | Surgery | Pathological findings of non nodular liver |
| 1 | 37 | Abdominal pain | Type 1 diabetes, Hashimoto thyroiditis | LH | Some foci of steatotic and clear hepatocytes. Mildly enlarged portal tracts with thickened arteries. |
| 2 | 49 | Abdominal pain | Gallbladder lithiasis | LH | Micro and macro steatosis (30 %). Few foci of steatotic hepatocytes, some portal tracts with enlarged arteries. |
| 3 | 35 | Incidental (episode of fever and rise in transaminases) | Persistant rise in GGT | RH | Macrovesicular steatosis (15 %). Small and rare peliotic areas. Accentuation of the lobular septation. |
| 4 | 39 | Incidental | LH | Macrovesicular steatosis (10 %). Small and rare peliotic areas. Some portal tracts with enlarged arteries. | |
| 5 | 49 | Follow up for chronic alcoholism | LH + IV | Severe steatosis (60 %). Few limited areas with dilated sinusoids and peliosis. Often enlarged arteries. | |
| 6 | 29 | Incidental | VII | ||
| 7 | 32 | Abdominal pain | Hemangioma | V, VI | Around nodule b, approximation of portal tracts, absence of portal veins, thickened wall of hepatic veins, one steatotic focus. |
| 8 | 47 | Abdominal pain | V, VI | Macrovesicular steatosis (50 %) medio/centro lobular. |
Cases 1 to 7 are women. Roman numbers indicate the segments of the liver. GGT: gammaglutamyl transpeptidase; HCC: hepatocellular carcinoma: LH: left hepatectomy; LL: left lobe; RL: right lobe.
Nine nodules were discovered by imaging techniques in specimens resected from 8 patients. Eight were FNH: 4 typical, 1 typical and telangiectatic, and 3 either typical steatotic or subtle FNH. One steatotic nodule was difficult to classify (see below). None of the patients had multiple lesions of typical FNH.
Eight additional small nodules were discovered during slicing. Only one was a typical FNH (steatotic).
For didactic purposes, we arbitrarily classified these small nodules into 5 types, from type 1 to type 5 (see Methods for description of different types), referring to the typical FNH lesion as type 5. Among the other small nodules, 3 being steatotic, 2 were classified as lesions of type 1 (Fig. 1), 2 as of types 2 (Fig. 2) and 3 lesions, and 2 as type 3 (Fig. 3) lesions, respectively; the seventh was classified as type 2, 3, and 4 lesions (Figs. 4, 5).
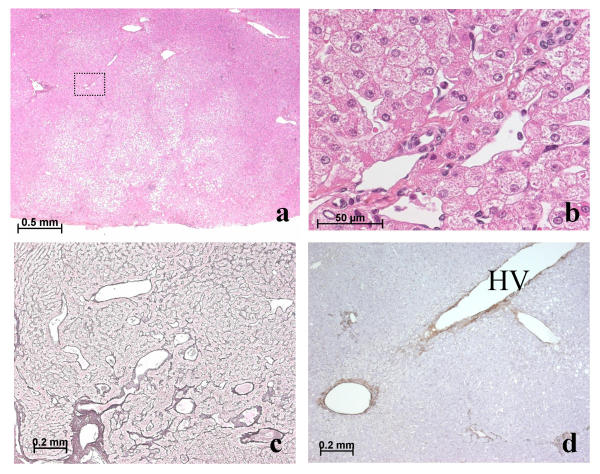
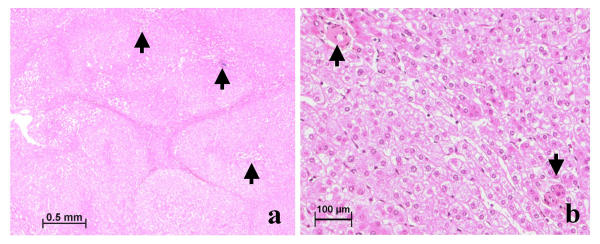
Figure 1.
(a, b) Patient 1, nodule b: type 1 lesion. Small steatotic nodule with mildly disorganized lobular architecture; some small portal tracts contain arteries unaccompanied by bile ducts. At higher magnification (box) (b), dilated thin-walled vessels adjoin a small portal tract at the periphery of the nodule. H&E. (c) Patient 3, nodule b: type 1 lesion. Dilated vessels in and around small portal tracts near a large portal tract. Reticulin staining. (d) Patient 1: Non-lesional liver. A large hepatic vein with an irregularly thickened wall lies near small portal tracts that contain numerous arterial cross-sections. Anti-α-SMA immunostaining
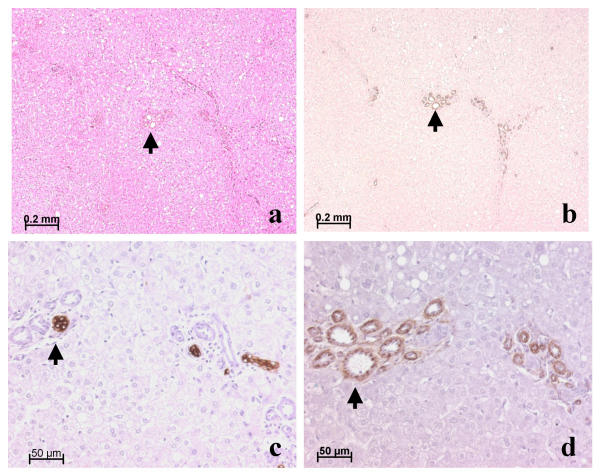
Figure 2.
(a, b, c, d) Patient 2, nodule a: type 2 lesion; all images represent the same region. Portal tracts (arrow) contain numerous arterial cross-sections and bile ducts. There is no ductular reaction. Portal veins are not identified with certainty. a, H&E; b, anti-α-SMA; c, anti-CK7; d, anti-CD34 immunostaining.
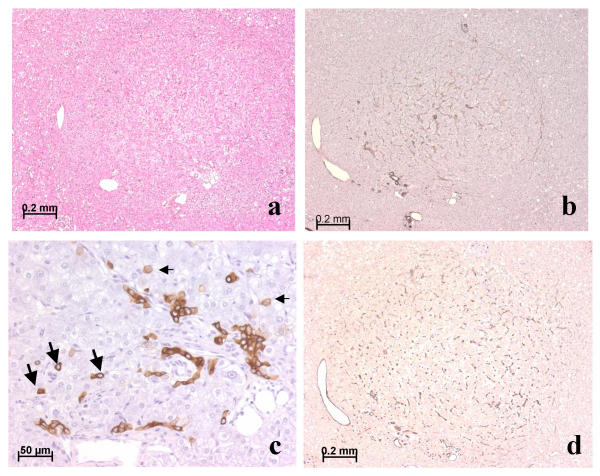
Figure 3.
(a, b, c, d), Patient 2, nodule a: type 3 lesion (same nodule as in Fig 2, but another region). This hyperplastic focus is surrounded with atrophic hepatocytes (a, b, d); arteries are seen at the periphery and inside the focus. A mild ductular reaction along the axis of arterioles is visualized by anti-CK7 immunostaining (c). A few isolated biliary cells (large arrow) and intermediate hepatocytic cells (small arrow) immunostain. Note the presence (a, b, d) of large venules near small arteries. Most sinusoids are capillarized, as shown by expression of CD34 by sinusoidal endothelial cells (d). a, H&E; b, anti-α-SMA; c, anti-CK7; d, anti-CD34 immunostaining.
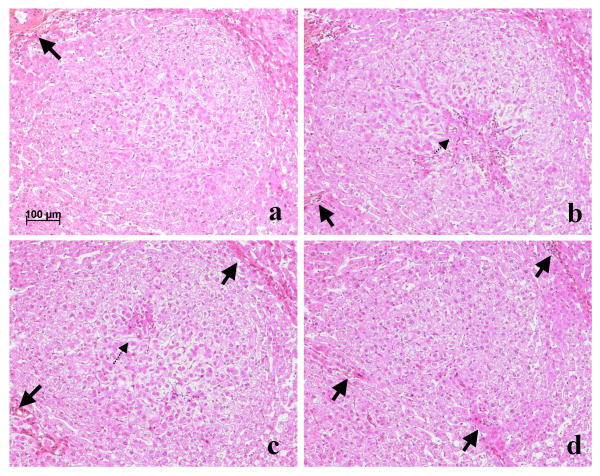
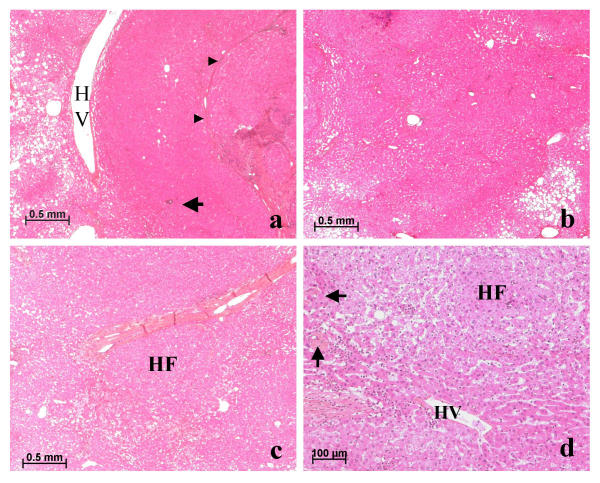
Figure 4.
(a, b, c, d), Patient 4, nodule b: type 4 lesion, serial sections. The hyperplastic focus is surrounded by atrophic hepatocytes and dilated sinusoids in which course arteries or arterioles (thick arrows). According to the plane of section, regions of regenerating hepatocytes, associated with ductular reaction (not visible at this magnification), and feeding arteries (dotted arrow) are more or less obvious. All, H&E.
Figure 5.
Patient 4, nodule b (same nodule as Fig 4, another region): type 3–4 lesion. (a) Fibrotic bands without ductular reaction encircle hyperplastic foci; arterioles in the center or at the periphery (arrow) are cuffed by a ductular reaction (not visible). Sinusoids along fibrotic bands are slightly dilated and a large region of sinusoidal dilatation can be seen on the left. H&E. (b) Between 2 hyperplastic foci is a zone of mild hepatocytic atrophy and sinusoidal dilatation in which arteries (arrow) course. H&E.
The non-classified nodule detected by imaging techniques (patient 1) corresponded to type 1–2 lesion. Both full-blown (Fig. 6a) and subtle FNH occasionally had type 2 or 3 lesions at their periphery (Fig. 6). A large hepatic vein wall hypertrophy was occasionally observed in the vicinity of nodules (Fig. 1d).
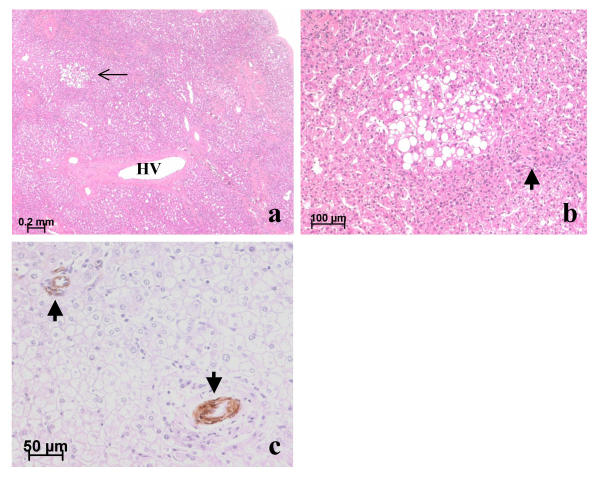
Figure 6.
Patient 8, periphery of nodule a (subtle FNH): types 2, 3, and 4 lesions (a, b, c); patient 4, periphery of nodule b: type 4 lesion (d). (a, b, c, d) The limit of the nodule is hard to define. In (a) and (b), steatosis is present outside the nodule; in (c), there is a thick band of collagen which contains abnormal vessels; in (d), the limit lies between the hepatic vein (HV) and the course of the arterioles (arrow). In (a), between the hepatic vein (HV) and the fibrous band of the subtle lesion of FNH (arrowhead), the rim of parenchyma looks superficially normal; however, it contains many isolated arteries (arrow). In (b, and d), regions of dilated sinusoids with compressed hepatocytes lie between hyperplastic foci (HF) with obvious or no ductular reaction. In (c), outside the limit of the subtle lesion of FNH, a region of sinusoidal dilatation is present, with peliosis encircling a hyperplastic focus (HF) beneath the fibrotic band. All, H&E.
Hyperplastic foci (Figs. 3, 5) in type 3 lesions were fed by arterioles accompanied by slight changes of the ductular reaction. These changes comprised anastomosing biliary ductules with poorly defined lumina, lined by flattened cells with scanty cytoplasm that in paraffin sections marked strongly for cytokeratin (CK) 7 and failed to mark or marked weakly for CK 19. A few small, single cells with an ovoid nucleus and scanty cytoplasm, marking for CK7 but not for CK19 (possible "undifferentiated progenitor cells"), were observed, as were intermediate cells, resembling hepatocytes, that marked faintly for CK7 (Fig. 3c). Sinusoids sometimes expressed endothelial antigen (CD34) and α-smooth muscle actin (α-SMA) (Figs. 3b,3d). Serial sections and CK7 immunostaining were often required to identify the ductular reaction.
Cirrhotic-like nodules progressively tend to appear when hyperplastic foci were separated by regions of sinusoidal dilatation containing arterioles and/or areas of cellular damage with necrosis, accompanied by thin fibrous bands which tend to approximate neighboring hepatic veins (Fig 5) characterizing type 4 lesion (minor form of FNH, so called "subtle FNH").
The non-nodular liver was grossly normal, although significant steatosis (> 30% of hepatocytes in sections) in 3 patients, including one addicted to alcohol. However, careful microscopic examination revealed a few focal abnormalities (Fig. 7): unpaired arteries, portal tracts with arteries larger than the associated bile duct, steatotic foci, and areas of sinusoidal dilatation or even peliosis.
Figure 7.
Non-nodular liver: (a, b) Patient 7; (c) Patient 3. (a) Near a steatotic nodule (not shown) lies a region of abnormal parenchyma. Note approximated portal tracts with thick-walled arteries and bile ducts (not visible at this magnification) but lacking portal veins, a large hepatic vein (HV) with a very thick wall, and a steatotic focus (thin arrow). (b) At a higher magnification, this steatotic focus near an artery (thick arrow) is partly bordered by slightly dilated sinusoids. H&E. (c) On the left, the portal tract contains an artery (arrow) but no visible bile duct; on the right an artery not partnered with a bile duct. Anti-α-SMA immunostaining.
Discussion
FNH is not a neoplasm but a nonspecific hyperplastic reaction to vascular abnormalities [1,2]. Vascular abnormalities can be developmental or secondary and vary in their distribution from focal to diffuse; leading to highly varied clinical and pathological presentations [8,9].
However, there is no clear understanding as to how this hyperplastic reaction gives rise to a kind of focal cirrhosis. The origin of the bile ductular structures, one of the hallmarks of the diagnosis, is not definitely established. The presence of "undifferentiated progenitor cells" in FNH suggests that the ductular reaction in these lesions results, at least partly, from activation of those cells [10]. If fibrosis in FNH arises as an accompaniment of the ductular reaction [11], how this fibrosis encircles nodules remains to be shown.
Since it is impossible to follow the growth of a given FNH lesion by microscopy, we can only speculate how nodules form. The histological criteria proposed to describe lesions as type 1, 2, or 3 are compatible with a high arterial influx even for tiny nodules; indeed, they are in favour of the diagnosis of small FNH-like lesions.
In addition, other arguments suggest that those small FNH-like lesions could be precursor lesions of FNH. These arguments are the following: the possible association of FNH-like lesions with either classical criteria of FNH in the same nodule (as in patient 6), or with typical FNH (in the case of several nodules, 5 patients in this series), or with hemangioma (one patient in this series).
Small FNH (with in the center typical cirrhotic-like nodules) may be surrounded with type 1 and 2 lesions (Fig. 6). Furthermore, beyond the apparent limit of a lesion of FNH, it was not rare to observe hyperplastic foci, as if another rim was underway, all together suggesting that growth was not completed. The possibility that these changes could be a secondary effect, related to the tumoral mass, cannot be ruled out but to us appears unlikely because of the small size of the nodule.
Small nodules may be difficult to identify. When they contain abnormal arteries (in size and/or number), accompanied by occasional bile ducts and/or portal vein branches, those arteries could represent the strongest and earliest identifiable sign of FNH (type 2 lesions). This is in accordance with the hypothesis of focal high arterial flow as either a primary or secondary phenomenon. We hypothesize that communication of arterioles with various vessels (terminal portal vein branches, inlet venules, even sinusoids) could lead to dilatation of the latter, a dilatation that we have sometimes observed as the sole abnormality in some small nodules (type 1 lesions).
However, taking into account that the lesions of FNH are usually stable, these FNH-like nodules could also be recognized as an insufficient type or abortive form of FNH.
We cannot ignore that not all nodules identified by imaging techniques or by the pathologist on macroscopy, are typical FNH or even FNH-like nodule; they may represent other lesions, including adenoma. Indeed, FNH has been described in association with hepatocellular adenoma [12-15] and with adenomatosis [16]. This association raises difficult diagnostic and pathogenetic problems [17], as mixed hyperplastic and adenomatous forms of FNH have been described [8]. In our experience, particularly in adenomatosis, it is sometimes impossible to identify with certainty whether some small nodules are indeed FNH or adenomas. Additional studies using more appropriate tools such as molecular techniques [18], as well as careful follow-up studies, will be necessary to resolve this issue.
An important observation made in this study was that the coexistence of typical lesions of FNH with nodule that resembled FNH was associated with vascular abnormalities in the non-nodular liver. It could indicate that both the frank FNH and nodule that resemble FNH are the visible part of a more diffuse pathological entity. FNH are generally assumed to be rather stable, but this may not apply to all small lesions. In at least one published instance, new FNH appeared during the follow-up of a patient who previously had a liver resection for FNH [19]. Finally, the hypertrophy of a large hepatic vein in the vicinity of some nodules remains unexplained; we can speculate that it could be related to the use of oral contraceptives [20] or to abnormal arterial feeding of the vein [21].
Conclusions
In keeping with the concept that in FNH increased arterial flow [3] hyperperfuses the local parenchyma leading to secondary hepatocellular hyperplasia, the presence of nodules that contain numerous or enlarged arteries in portal tracts or isolated arteries, associated with a focus of hyperplastic hepatocytes, suggests that these nodules and (a fortiori) nodules with some degree of ductular reaction are nodules with features of FNH. Although these small nodules can be considered as insufficient type or abortive form of FNH, or adenoma, they can be precursors of the large mass lesions in which FNH was recognized and defined.
Methods
During 3 years (1999 – 2001), 8 patients (7 women, all on oral contraceptives, and 1 man) had a partial hepatectomy for the removal of nodules. Five patients underwent resection for one nodule thought or suspected to be adenoma. Among them, one was known to have had FNH before. One patient underwent resection for a painful mass considered a FNH and 2 for a mass suspected to be a hepatocellular carcinoma (1 man; 1 woman with chronic alcoholism). Relevant clinical, radiological, surgical, and gross-anatomy data are presented in Tables 1 and 2. During careful slicing and inspection of the resected liver, 8 additional nodules were discovered in five patients; one nodule macroscopically resembled a typical FNH (patient 5, nodule b). The 7 others were distinguished from the surrounding normal tissue by a slight change in color; the nodules usually were paler. The consistency of these nodules was difficult to discern because of their small size.
All nodules were sampled, as was the non-nodular liver. One to 10 blocks were prepared for each nodule, according to nodule size, with 4 to 6 blocks for the non-nodular liver. Sections were stained routinely (H&E, trichrome, reticulin) as well as immunostained for detection of CK7, CK19, α-SMA, and CD34. Serial sections were examined on occasion.
Nodules were arbitrarily classified into 5 types:
1 – Type 1 lesions were tiny nodules, steatotic or not, with mildly disorganized liver architecture and dilatation of thin-walled vessels in the immediate vicinity of portal tracts (Fig. 1).
2 – Type 2 lesions were nodules with mildly disorganized liver architecture and enlarged or tortuous arteries (with tortuosity identified by finding multiple cross-sections of the same vessel) in portal tracts or in septa. Portal tracts sometimes lacked a bile duct or portal vein (Fig. 2).
3 – Type 3 lesions were nodules like those of type 2 that also included hyperplastic foci (Fig. 3).
4 – Type 4 lesions were minor or "subtle" forms of FNH (Fig. 4), with incomplete or very small fibrous scar, inconstant ductular reaction, and incomplete nodular organization.
5 – Type 5 lesions were full-blown FNH.
Authors' contributions
C Laurent obtained the clinical data. C Balabaud wrote the paper. S Lepreux contributed to the pathological examination. P Bioulac-Sage did the pathological examination and reviewed the paper. All authors read and approved the final manuscript.
Acknowledgments
Acknowledgements
The authors thank Professors J Saric and J Carles for referring their patients and giving access to those patients' records, Doctors B Le Bail and A Rullier for their participation in histopathological assessment and Dr Alex Knisely for reviewing the manuscript.
Contributor Information
Sébastien Lepreux, Email: sebastien.lepreux@chu-bordeaux.fr.
Christophe Laurent, Email: christophe.laurent@chu-bordeaux.fr.
Charles Balabaud, Email: charles.balabaud@chu-bordeaux.fr.
Paulette Bioulac-Sage, Email: paulette.bioulac-sage@chu-bordeaux.fr.
References
- Fukukura Y, Nakashima O, Kusaba A, Kage M, Kojiro M. Angioarchitecture and blood circulation in focal nodular hyperplasia of the liver. J Hepatol. 1998;29:470–475. doi: 10.1016/S0168-8278(98)80067-6. [DOI] [PubMed] [Google Scholar]
- Gaiani S, Piscaglia F, Serra C, Bolondi L. Hemodynamics in focal nodular hyperplasia. J Hepatol. 1999;31:576. doi: 10.1016/S0168-8278(99)80057-9. [DOI] [PubMed] [Google Scholar]
- Wanless IR, Mawdsley C, Adams R. On the pathogenesis of focal nodular hyperplasia of the liver. Hepatology. 1985;5:1194–1200. doi: 10.1002/hep.1840050622. [DOI] [PubMed] [Google Scholar]
- Marti-Bonmati L, Casillas C, Dosda R. Enhancement characteristics of hepatic focal nodular hyperplasia and its scar by dynamic magnetic resonance imaging. Magma. 2000;10:200–204. doi: 10.1007/BF02590646. [DOI] [PubMed] [Google Scholar]
- Miyayama S, Matsui O, Ueda K, Kifune K, Yamashiro M, Yamamoto T, Komatsu T, Kumano T. Hemodynamics of small hepatic focal nodular hyperplasia: evaluation with single-level dynamic CT during hepatic arteriography. AJR Am J Roentgenol. 2000;174:1567–1569. doi: 10.2214/ajr.174.6.1741567. [DOI] [PubMed] [Google Scholar]
- Mortele KJ, Praet M, Van Vlierberghe H, Kunnen M, Ros PR. CT and MR imaging findings in focal nodular hyperplasia of the liver: radiologic-pathologic correlation. AJR Am J Roentgenol. 2000;175:687–692. doi: 10.2214/ajr.175.3.1750687. [DOI] [PubMed] [Google Scholar]
- Rodes J, Sherlock S. Focal nodular hyperplasia in a young female. J Hepatol. 1998;29:1005–1009. doi: 10.1016/S0168-8278(98)80132-3. [DOI] [PubMed] [Google Scholar]
- Nguyen BN, Flejou JF, Terris B, Belghiti J, Degott C. Focal nodular hyperplasia of the liver: a comprehensive pathologic study of 305 lesions and recognition of new histologic forms. Am J Surg Pathol. 1999;23:1441–1454. doi: 10.1097/00000478-199912000-00001. [DOI] [PubMed] [Google Scholar]
- Bioulac-Sage P, Balabaud C, Wanless IR. Diagnosis of focal nodular hyperplasia: not so easy. Am J Surg Pathol. 2001;25:1322–1325. doi: 10.1097/00000478-200110000-00015. [DOI] [PubMed] [Google Scholar]
- Roskams T, De Vos R, Desmet V. 'Undifferentiated progenitor cells' in focal nodular hyperplasia of the liver. Histopathology. 1996;28:291–299. doi: 10.1046/j.1365-2559.1996.d01-438.x. [DOI] [PubMed] [Google Scholar]
- Kinnman N, Housset C. Peribiliary myofibroblasts in biliary type liver fibrosis. Front Biosci. 2002;7:d496–503. doi: 10.2741/A790. [DOI] [PubMed] [Google Scholar]
- Guntz M, Francois H, Ben Bouali A, Joubaud F, Taviaux R. Hepatocellular adenoma within focal nodular hyperplasia. Gastroenterol Clin Biol. 1983;7:826–827. [PubMed] [Google Scholar]
- Grange JD, Guechot J, Legendre C, Giboudeau J, Darnis F, Poupon R. Liver adenoma and focal nodular hyperplasia in a man with high endogenous sex steroids. Gastroenterology. 1987;93:1409–1413. doi: 10.1016/0016-5085(87)90273-3. [DOI] [PubMed] [Google Scholar]
- Ichikawa T, Federle MP, Grazioli L, Nalesnik M. Hepatocellular adenoma: multiphasic CT and histopathologic findings in 25 patients. Radiology. 2000;214:861–868. doi: 10.1148/radiology.214.3.r00mr28861. [DOI] [PubMed] [Google Scholar]
- Marks WH, Thompson N, Appleman H. Failure of hepatic adenomas (HCA) to regress after discontinuance of oral contraceptives. An association with focal nodular hyperplasia (FNH) and uterine leiomyoma. Ann Surg. 1988;208:190–195. doi: 10.1097/00000658-198808000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grazioli L, Federle MP, Ichikawa T, Balzano E, Nalesnik M, Madariaga J. Liver adenomatosis: clinical, histopathologic, and imaging findings in 15 patients. Radiology. 2000;216:395–402. doi: 10.1148/radiology.216.2.r00jl38395. [DOI] [PubMed] [Google Scholar]
- Bralet MP, Terris B, Vilgrain V, Bregeaud L, Molas G, Corbic M, Belghiti J, Flejou JF, Degott C. Epithelioid hemangioendothelioma, multiple focal nodular hyperplasias, and cavernous hemangiomas of the liver. Arch Pathol Lab Med. 1999;123:846–849. doi: 10.5858/1999-123-0846-EHMFNH. [DOI] [PubMed] [Google Scholar]
- Bluteau O, Jeannot E, Bioulac-Sage P, Marques JM, Blanc JF, Bui H, Beaudoin JC, Franco D, Balabaud C, Laurent-Puig P, Zucman-Rossi J. Bi-allelic inactivation of TCF1 in hepatic adenomas. Nat Gene. 2002;32:312–315. doi: 10.1038/ng1001. [DOI] [PubMed] [Google Scholar]
- Sadowski DC, Lee SS, Wanless IR, Kelly JK, Heathcote EJ. Progressive type of focal nodular hyperplasia characterized by multiple tumors and recurrence. Hepatology. 1995;21:970–975. [PubMed] [Google Scholar]
- Vandenbroucke JP, Rosing J, Bloemenkamp KW, Middeldorp S, Helmerhorst FM, Bouma BN, Rosendaal FR. Oral contraceptives and the risk of venous thrombosis. N Engl J Med. 2001;344:1527–1535. doi: 10.1056/NEJM200105173442007. [DOI] [PubMed] [Google Scholar]
- Ekataksin W. The isolated artery: an intrahepatic arterial pathway that can bypass the lobular parenchyma in mammalian livers. Hepatology. 2000;31:269–279. doi: 10.1002/hep.510310203. [DOI] [PubMed] [Google Scholar]