Abstract
Asthma is a chronic disease with both inflammatory and bronchoconstrictive elements and often requires multiple medications. Most asthma regimens include medications with different therapeutic modes of action and a number of different medication delivery devices. To effectively participate in their asthma management, patients need to recognize each of their medication types, understand their purpose, adhere to their treatment regimen, and be proficient in using the required delivery devices. This study evaluated patient knowledge of asthma pharmacotherapy and adherence. An interview study was undertaken in two rural locations, in Australia, to elicit participants' knowledge, use, and inhalation device technique. Of participants, 75.9% used preventer medication and the remaining 24.1% used reliever medication only. Of those using preventer medication, 82.5% could distinguish their preventer from a range of asthma medicines. Metered dose inhalers (MDIs) were used by 80% of participants; 23% used a Turbuhaler®; 24% used an Accuhaler®; and 5% used an MDI with a spacer device. The study established poor medication knowledge, suboptimal device technique, and disturbing levels of adherence with management recommendations. Asthma education strategies need to be modified to engage patients with low asthma knowledge to achieve improved patient outcomes. Further, strategies need to motivate patients to use preventer medication during times when they feel well.
Keywords: asthma, medication knowledge, medication adherence
Asthma in Australia
With two out of five Australians exhibiting symptoms consistent with asthma at some stage in their lives, asthma is one of Australia's major health problems and is associated with significant morbidity, avoidable mortality, and impaired quality of life (Woolcock et al 2002; Wilson 2003). As a result of the prevalence of asthma in the general community, which is widely considered to be 20% in children and 7%–12% in adults (Bauman 1999), it would be expected that about one in ten adults that enter a pharmacy suffer from asthma.
Asthma is a disease that has both chronic and acute components and often requires complex management. Most people with asthma are prescribed regimens that include multiple medications with different actions and one or more different devices for the delivery of medications (NAC 2002). The increasing prevalence of asthma in Australia and worldwide (Pearce et al 2000; Barraclough et al 2002; Mannino et al 2002) means that patient understanding and adherence to asthma management guidelines is critically important (AIHW 2000).
Asthma management, patient knowledge, and therapy
Aspects of disease management that are important to asthma include knowledge of the disease, its treatment, and the effective use of different therapies. Healthcare providers play a crucial role in empowering patients with the necessary skills and knowledge to manage their asthma.
It is important however to remember that whilst the goal of a healthcare professional might be clinical, such as objective improvement in lung function parameters, patients are focused on their self-perceived health status, which likely includes their ability to participate without limitation in their everyday life (Clark and Partridge 2002). If not managed effectively, asthma is potentially a debilitating condition that can cause a reduced quality of life in terms of physical, social, and psychological aspects (AIHW 2000; Mathers 2000; Wilson 2003).
Increasing patients' knowledge about their asthma therapy is vital to asthma management (Walker and Edwards 1999), as people with asthma are likely to be using multiple medications and delivery devices. Fitzclarence and Henry (1990) asked participants to give examples of medications that could be used to prevent and treat asthma attacks. They demonstrated that 50% of people with asthma knew the action of different medications with some demonstrating an exceptional level of knowledge (Fitzclarence and Henry 1990).
Medication is generally delivered directly to the lung by specialized devices. These devices require that the patient learn an effective device technique to use their medication (Wilson 2003). Studies that have examined device technique have recognized that MDIs are difficult for patients to use as they require coordination, breath hold ability, and patient hand strength and dexterity (Rydman et al 1999; Anderson 2001). Further, inhaler technique has been established to decline rapidly over time and reassessment at each supply can be beneficial (Clark and Partridge 2002; Pain 2003; Wilson 2003).
Asthma management adherence
Meichenbaum and Turk (1987) conceptualize adherence as “active, voluntary, collaborative involvement of the patient in a mutually acceptable course of behavior to produce a desired preventative or therapeutic result”. Some consider that the terms adherence and compliance are synonymous. By adopting this definition, reasoned agreement with the management plan on the part of the patient is implied. Whilst asthma management plans incorporate a number of recommended health behaviors, the role of medication is paramount. Medication adherence has been defined as “the amount of time a patient takes a given medication as prescribed” (Jones et al 2003, p 94). Rates of nonadherence with pharmacotherapy across all chronic disease states including asthma is high, ranging from 40%–70% (Clark and Partridge 2002; Sawyer 2002). Patients should be educated about their drug therapy including how the drugs act so that they can make logical decisions regarding their treatment, since use of medicinal drugs is not founded on medication knowledge alone but also on lay reasoning and logic (Lumme and Sandt et al 2000). People with asthma can lead a normal and healthy life, and one major step in insuring this is the adherence to their management plan. A significant challenge for healthcare professionals is motivating patients to take preventive medication when asymptomatic (Anarella et al 2004). The aim of this study was to evaluate patient knowledge of asthma pharmacotherapy and adherence.
Methods
Recruitment
The study was undertaken in five pharmacies in two rural locations in Australia. All individuals entering the pharmacies were, after a brief introduction, asked if they had asthma and if so, were then invited to participate in the study. The questionnaire was administered by one of the researchers (TF) during a one-on-one interview. Times of recruitment were varied in an attempt to avoid any bias or restriction of the sample in relation to their gender, age, or employment status. The Charles Sturt University Ethics in Human Research Committee granted approval for this project.
Interview schedule
A structured interview was conducted using a questionnaire designed to elicit information in the following areas: basic sociodemographics, asthma medication and management knowledge, adherence, and quality of life (see Table 1). Questions were asked exactly as written and in the order specified by the interview schedule. During the interview, participants were asked to identify their medication, and describe their treatment regimen and the mode of action of “preventer” and “reliever” medications. A colored medication chart was used as a prompt because many patients cannot remember their medication names but are more likely to be able to identify them. Additionally participants were asked about their asthma management plan. Participants' medication adherence and skills at using medication devices were also assessed.
Table 1.
Questionnaire structure
| Domain | Information about the domain |
|---|---|
| Sociodemographics | 6 items: age, gender, ethnic background, marital status, education, smoking status |
| Health professionals | 2 items: health professionals role in asthma management |
| Medication knowledge | 5 items: information about patients understanding of medication types and actions |
| Medication adherence | 6 items: frequency of missed doses of medication and reasons |
| Asthma action plan | 2 items: knowledge and ownership |
Participants' responses were recorded as discrete values, free format, or multi-option responses as appropriate. Free responses to medication and asthma knowledge items were scored, summed, and categorized into 3 levels: “poor”, “basic”, and “clear”. Each participant was invited to demonstrate their technique using a placebo for the medication delivery device that they regularly used. Their device technique was scored against a checklist and categorized.
Another component of the survey involved the use of an asthma-specific quality of life (QOL) evaluation (Marks 1992). This questionnaire encompasses three domains of life: the physical, social, and psychological aspects. In the original version of the questionnaire, the participants were presented with a series of five options to best describe their response to each statement: “none”, “mildly”, “moderately”, “severely”, and “very severely”. However, in the development of this study it was felt that there was a certain degree of ambiguity between the terms “severely” and “very severely”, and so only four options were used: “none”, “mildly”, “moderately”, and “severely”. Other researchers have previously made adjustments to the subscale structure and scoring of the questionnaire prior to its application to eliminate perceived overlap (Katz et al 2001).
Analysis
The analysis of the data was performed using Statistical Packages for the Social Sciences (SPSS) version 10.0 (Norusis 1993). Once the data had been collected, the information was coded and entered into a database, verified for data entry errors, and corrected. Frequencies, means, and standard deviations were examined for all of the participant responses. Cross-tabulations were also used to identify relationships between the study variables. Scores were calculated for the QOL section.
Results
Sociodemographics
There were 83 participants in the study. The participation rate was 92% of those individuals eligible. The mean age of participants was 58.9 (± 17.7) years. Forty-five percent of respondents were male and 55% were female. Smokers accounted for 14.5% of the respondents, with an average of 17.5 cigarettes smoked per day. The mean number of occasions of exercise per week was 2.8.
Medication Knowledge
Preventer medication was used by 75.9% of participants; the remaining 24.1% used reliever medication only to manage their condition. Of those using reliever alone, 30% used it more than 3–4 times per week.
Respondents to items concerning mode of action of “preventer” and “reliever” medications number 80.7%. Participants provided a response in their own words with 6.3% providing an incorrect response when defining preventer medication and 7.8% unable to define reliever medication (refer to Figure 1).
Figure 1.
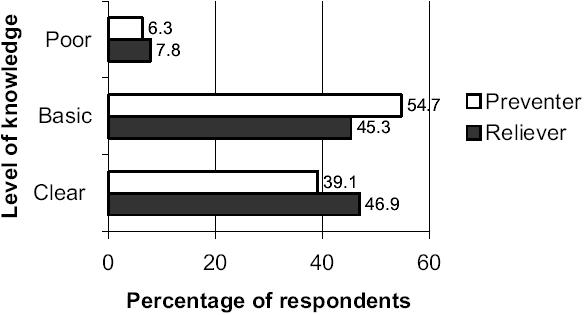
Participants' knowledge of mode of action of “preventer” and “reliever” medication.
Of participants using preventer medication, 82.5% could distinguish and correctly identify their preventer from the range of asthma medications. As the depth of knowledge of the mode of action of preventer medication increased (“basic” 81%; “clear” 95.7%), so did the participants ability to identify their preventer medication.
Medication adherence
Thirty-eight percent of patients used preventer medication as prescribed and 11% never used it (refer to Figure 2). Participants offered a number of reasons explaining their nonadherence: the most common (57%) was forgetting to take preventer medication, 10% were too busy, 10% were concerned about side effects, and 9% don't believe it is effective. Other responses were offered only by individual participants and were not endorsed by the participant sample. Older patients adhered to their medication regimen more closely than younger patients (refer to Figure 3).
Figure 2.

Participant adherence with “preventer” medication regimen.
Figure 3.

Effect of participant age on adherence.
Medication device technique
Sixty-six percent of participants used only one device whilst 33.7% used two different devices. MDIs were used by 80% of participants; 23% used a Turbuhaler®; 24% used an Accuhaler®; and 5% used an MDI with a spacer device. Effectiveness of device usage is classified for each device type in Table 2. Errors in device technique arose at almost every stage of the process of MDI device actuation (refer to Figure 4).
Table 2.
Effectiveness of participants' device technique
| Rating (% users) | MDI | MDI Turbuhaler® | Accuhaler® | MDI+spacer |
|---|---|---|---|---|
| Ineffective | 39 | 11 | 15 | 25 |
| Acceptable | 27 | 52 | 10 | 0 |
| Optimal | 34 | 37 | 75 | 75 |
Abbreviation: MDI, metered dose inhalers.
Figure 4.

Observed errors with metered dose inhaler (MDI) technique.
Quality of life
The average QOL score for the sample population was found to be 1.99 (range 0.83–8.13). Males had a higher mean QOL score (2.17) than females (1.84). There was a significant negative correlation (Pearson's r – 0.352, p = 0.001) between QOL score and adherence with preventer medication such that as quality of life decreased adherence with preventer medication increased.
Discussion and conclusion
Pharmacies are an ideal site for surveying people with chronic diseases as most are managed by prescribed medicines. Interview studies have been shown to produce better completion rates than other types of questionnaires and are a good method for administration of detailed or complex surveys (Bailey 1982). Surveying at local pharmacies may however, introduce bias by recruiting people who are perhaps more concerned for their health (Lupton and Najman 1995).
People with asthma are likely to be using multiple medications required at different times during the course of the disease; therefore, increasing patients' knowledge about their asthma therapy is vital to asthma management (Walker and Edwards 1999). In this study, we identified relatively high preventer use with 79% of participants prescribed this medication. Participants could describe the actions of preventer (83.8%) and reliever (92.2%) medication appropriately. Although there is a paucity of research addressing this issue, these results are comparable to previous Australian research that identified that 90% of those surveyed were able to distinguish their preventer and reliever medications and when to use them (Anonymous 2000). However, other research conducted in Trinidad more recently (Pinto-Pereira et al 2002), established that only 53% of chest clinic patients could provide accurate reasons for using preventer and reliever medications.
Of concern was the overuse of reliever medication which occurred in 30% of those using reliever alone to manage their asthma. If a patient is over reliant on this medication they may develop tachyphylaxis and when they need bronchodilating action their reliever will not be as effective. Regular use of reliever medications alone has been associated with a 2.6 increased risk of death or near death (Hartzema 2000). Clearly, asthma management guidelines would indicate the use of preventer medication in this group.
While it is often reported that patients have difficulty communicating to health professionals the medications they are currently taking, this study found that over 80% could correctly identify their medications from a medication chart. The use of visual prompting is a strong tool for some people and can provide a quick way for helping people to remember a particular item (Sargeant and Unkenstein 1998), and its use in future research is encouraged.
Poor adherence by people with asthma is extensively documented especially for preventer medications (Sawyer 2002). Of those prescribed preventer in this study, only 38% were adherent to dose and dose frequency recommendations, a further 41% were adherent to dose but 11% did not use their preventer at all. These results are consistent with other research where 38% of respondents used preventer medication as prescribed by their doctor (Anarella et al 2004). As QOL decreased, adherence with preventer medication increased and this may be attributable to increased patient motivation.
The major reason for nonadherence identified in this study was forgetfulness. This is not unique to this study and has been documented by other researchers (Chambers et al 1999; Chapman et al 2000). Further reasons included concern about side effects and a feeling that there was no need to take the medication when well. This study therefore identified areas for improvement in asthma management, which included education about the risk/benefit ratio of preventers. Additional strategies to address poor adherence have been identified in the literature and include reducing the dose frequency, and choosing the same type of delivery device for both preventer and reliever medications (Sawyer 2002).
Our study identified suboptimal MDI device technique with the most frequently recorded errors related to the required changes in ventilatory pattern and breath holding. This is consistent with the literature (Pinto-Pereira et al 2002; Slader et al 2002; Pain 2003). Dry powder devices are generally considered to present fewer problems due to a lesser requirement for patient coordination (Pain 2003). However, research has established that patients tend to lack confidence in this device because a visible aerosol is not produced nor sensed on the pharynx. Despite the differences in devices, the critical feature in dosing efficacy rests more on patient skill than the features of the device itself (Reed 2004). Consistent with the literature, this study provided evidence of the need for improved and ongoing device use education (Slader et al 2002).
Our study demonstrated that substantial numbers of people with asthma lack the necessary knowledge to contribute effectively to their disease state management. Strategies need to be developed to engage patients with low asthma knowledge in asthma education programs to achieve improved patient outcomes, including quality of life. Further, strategies need to be tailored to motivate patients to take preventer medication during times when they feel well.
References
- [AIHW] Australian Institute of Health and Welfare. 2000. Australia's health. Canberra: AIHW; 2000. [Google Scholar]
- Anarella J, Roohan P, Balistreri E, et al. A survey of Medicaid recipients with asthma: perceptions of self-management, access and care. Chest. 2004;125:1359–67. doi: 10.1378/chest.125.4.1359. [DOI] [PubMed] [Google Scholar]
- Anderson PJ. Delivery options and devices for aerosolized therapeutics. Chest. 2001;120:89S–93S. doi: 10.1378/chest.120.3_suppl.89s. [DOI] [PubMed] [Google Scholar]
- Anonymous. Seretide's combination therapy advances asthma management. Aust J Pharm. 2000;81:1028–9. [Google Scholar]
- Bailey K. Methods of social research. 2nd ed. New York: Collier Macmillan; 1982. [Google Scholar]
- Barraclough R, Devereux G, Hendrick DJ, et al. Apparent but notreal increase in asthma prevalence during the 1990s. Eur Respir J. 2002;20:826–33. doi: 10.1183/09031936.02.00822002. [DOI] [PubMed] [Google Scholar]
- Bauman A. Melbourne: National Asthma Campaign; 1999. A decade of coordinated asthma management in Australia–latest statistical trends. [Google Scholar]
- Chambers CV, Markson L, Diamond JJ, et al. Health beliefs and compliance with inhaled corticosteroids by asthmatic patients in primary care practices. Respir Med. 1999;93:88–94. doi: 10.1016/s0954-6111(99)90296-2. [DOI] [PubMed] [Google Scholar]
- Chapman KR, Walker L, Cluley S, et al. Improving patient compliance with asthma therapy. Respir Med. 2000;94:2–9. doi: 10.1053/rmed.1999.0667. [DOI] [PubMed] [Google Scholar]
- Clark NM, Partridge MR. Strengthening asthma education to enhance disease control. Chest. 2002;121:1661–9. doi: 10.1378/chest.121.5.1661. [DOI] [PubMed] [Google Scholar]
- Fitzclarence CB, Henry RL. Validation of an asthma knowledge questionnaire. J Paediatr Child Health. 1990;26:200–4. doi: 10.1111/j.1440-1754.1990.tb02429.x. [DOI] [PubMed] [Google Scholar]
- Hartzema A. Quality improvement in pharmacotherapy – preliminary results from the United States. Pharm J. 2000;265:498. [Google Scholar]
- Jones C, Santanello NC, Boccuzzi SJ, et al. Adherence to prescribed treatment for asthma: evidence from pharmacy benefits data. J Asthma. 2003;40:93–101. doi: 10.1081/jas-120017212. [DOI] [PubMed] [Google Scholar]
- Katz PP, Eisner MD, Henke J, et al. The Marks Asthma QOL Questionnaire: further validation and examination of responsiveness to change. J Clin Epidemiol. 2001;54:106–7. doi: 10.1016/s0895-4356(99)00026-8. [DOI] [PubMed] [Google Scholar]
- Lumme-Sandt K, Hervonen A, Jylha M. Interpretative repertoires of medication among the oldest-old. Soc Sci Med. 2000;50:1843–50. doi: 10.1016/s0277-9536(99)00421-9. [DOI] [PubMed] [Google Scholar]
- Lupton GM, Najman JM. Sociology of health and illness: Australian readings. 2nd ed. Australia: Macmillan; 1995. [Google Scholar]
- Mannino DM, Homa DM, Akinbami LJ, et al. Surveillance for asthma – United States, 1980–1999. MMWR Surveill Summ. 2002;51:1–13. [PubMed] [Google Scholar]
- Marks GB, Dunn SM, Woolcock AJ. A scale for the measurement of quality of life of adults with asthma. J Clin Epidemiol. 1992;45:461–72. doi: 10.1016/0895-4356(92)90095-5. [DOI] [PubMed] [Google Scholar]
- Mathers CD, Theo Vos E, Stevenson CE, et al. The Australian Burden of Disease Study: measuring the loss of health from disease, injuries and risk factors. Med J Aust. 2000;172:592–6. doi: 10.5694/j.1326-5377.2000.tb124125.x. [DOI] [PubMed] [Google Scholar]
- Meichenbaum D, Turk DC. In: Treatment adherence: terminology, incidence and conceptualisation. Facilitating treatment adherence. Meichenbaum D, Turk DC, editors. New York: Plenum Pr.; 1987. pp. 19–39. [Google Scholar]
- [NAC] National Asthma Council. 2002. Asthma management handbook. Melbourne: NAC; 2002. [Google Scholar]
- Norusis MJ. SPSS for Windows base system user's guide release 6.0. Chicago: SPSS Inc.; 1993. [Google Scholar]
- Pain MCF. Delivering inhaled asthma therapy. Aust Prescriber. 2003;26:5–7. [Google Scholar]
- Pearce N, Sunyer J, Cheng S, et al. Comparison of asthma prevalence in the ISAAC and ECRHS. ISAAC Steering Committee and the European Community Respiratory Health Survey. International Study of Asthma and Allergies in Childhood. Eur Respir J. 2000;16:420–6. doi: 10.1183/9031936.00.16337700. [DOI] [PubMed] [Google Scholar]
- Pinto-Pereira LM, Clement Y, Da Silva CK, et al. Understanding and use of inhaler medication by asthmatics in specialty care in Trinidad: a study following development of Caribbean guidelines for asthma management and prevention – clinical investigations. Chest. 2002;121:1833–40. doi: 10.1378/chest.121.6.1833. [DOI] [PubMed] [Google Scholar]
- Reed CE. Inhaled corticosteroids: why do physicians and patients fail to comply with guidelines for managing asthma. Mayo Clinic Proc. 2004;79:453–5. doi: 10.4065/79.4.453. [DOI] [PubMed] [Google Scholar]
- Rydman RJ, Sonethal K, Tadimeti L, et al. Evaluating the outcome of two teaching methods of breath activated inhaler in an inner city asthma clinic. J Med Syst. 1999;23:349–56. doi: 10.1023/a:1020525116505. [DOI] [PubMed] [Google Scholar]
- Sargeant D, Unkenstein A. Remembering well. St Leonards: Allen and Unwin; 1998. [Google Scholar]
- Sawyer SM. Action plans, self-monitoring and adherence: changing behaviour to promote better self-management. Med J Aust. 2002;177:S72–4. doi: 10.5694/j.1326-5377.2002.tb04825.x. [DOI] [PubMed] [Google Scholar]
- Slader CA, Reddel HK, Bosnic-Anticevich S. Use of CFC-free metered dose inhalers: do patients and pharmacists know what to do? Aust Pharm. 2002;21:526–31. [Google Scholar]
- Walker R, Edwards C, editors. Clinical pharmacy and therapeutics. 2nd ed. New York: Churchill Livingstone; 1999. [Google Scholar]
- Wilson J. Pharmacists-making a difference in asthma management. Aust J Pharm. 2003;84:638–41. [Google Scholar]
- Woolcock AJ, Bastiampillai SA, Marks GB, et al. The burden of asthma in Australia. Sydney: The Cooperative Research Centre for Asthma; 2002. [Google Scholar]


