Abstract
Background: Spinal hyperbaric ropivacaine may produce more predictable and reliable anesthesia than plain ropivacaine for cesarean section. The dose-response relation for spinal hyperbaric ropivacaine is undetermined. This double-blind, randomized, dose-response study determined the ED50 (50% effective dose) and ED95 (95% effective dose) of spinal hyperbaric ropivacaine for cesarean section anesthesia. Methods: Sixty parturients undergoing elective cesarean section delivery with use of combined spinal-epidural anesthesia were enrolled in this study. An epidural catheter was placed at the L1~L2 vertebral interspace, then lumbar puncture was performed at the L3~L4 vertebral interspace, and parturients were randomized to receive spinal hyperbaric ropivacaine in doses of 10.5 mg, 12 mg, 13.5 mg, or 15 mg in equal volumes of 3 ml. Sensory levels (pinprick) were assessed every 2.5 min until a T7 level was achieved and motor changes were assessed by modified Bromage Score. A dose was considered effective if an upper sensory level to pin prick of T7 or above was achieved and no intraoperative epidural supplement was required. ED50 and ED95 were determined with use of a logistic regression model. Results: ED50 (95% confidence interval) of spinal hyperbaric ropivacaine was determined to be 10.37 (5.23~11.59) mg and ED95 (95% confidence interval) to be 15.39 (13.81~23.59) mg. The maximum sensory block levels and the duration of motor block and the rate of hypotension, but not onset of anesthesia, were significantly related to the ropivacaine dose. Conclusion: The ED50 and ED95 of spinal hyperbaric ropivacaine for cesarean delivery under the conditions of this study were 10.37 mg and 15.39 mg, respectively. Ropivacaine is suitable for spinal anesthesia in cesarean delivery.
Keywords: Anesthesia, Obstetric, Cesarean section, Anesthetics local, Ropivacaine, Anesthetic techniques, Subarachnoid, Dose-response
INTRODUCTION
Ropivacaine is a new long-acting amide local anesthetic with structural and pharmacodynamic similarity to bupivacaine. However, ropivacaine has a lower central nervous system and cardiotoxic potential than bupivacaine. Many investigators reported that ropivacaine can be used safely for spinal anesthesia in obstetric patients (Khaw et al., 2002; Gautier et al., 2003). Dose requirements of spinal plain ropivacaine for cesarean section have variable range from 8 to 22.5 mg, and a previous dose-response study with plain ropivacaine for cesarean section had estimated the 95% effective dose (ED95) to be 26.8 mg (Khaw et al., 2001). However, we usually use hyperbaric ropivacaine for spinal anesthesia for cesarean section in clinical practice because spinal hyperbaric ropivacaine may produce more predictable and reliable anesthesia than plain ropivacaine and with a shorter duration of sensory and motor block (Fettes et al., 2005; Whiteside et al., 2001). So far, the optimum dosage regimen for spinal hyperbaric ropivacaine used in cesarean section has not been determined. Furthermore, data from non-obstetric patients cannot be directly extrapolated to obstetrics because of lower dose requirements (Fassoulaki et al., 2004). The aim of the present randomized, prospective, double-blind study was to determine the dose-response of spinal hyperbaric ropivacaine for elective cesarean section.
METHODS
Subjects and setting
Sixty parturients with American Society of Anesthesiologists (ASA) physical status I or II who were scheduled to undergo elective cesarean delivery using spinal anesthesia at term were enrolled in the study and all patients gave informed written consent. Patients with a history of allergy or sensitivity to amide-type local anesthetics, maternal diabetes, alcohol, drug or medication abuse, multiple pregnancies, suspected fetal abnormality, or complicated pregnancies were excluded. All patients received no premedication.
Study protocol
Before the study, patients were instructed on the method of sensory, motor and pain assessments, and baseline measurements were performed. Sensory changes were recorded bilaterally along the midclavicular line by assessing changes in pin-prick sensation using a 7G needle. Motor block in the lower limbs was graded according to the modified Bromage Scale: 0=full leg movement; 1=inability to raise extended leg, can bend knee; 2=inability to bend knee, can flex ankle; 3=no movement (Fettes et al., 2005). Pain was assessed with a 10-cm linear visual analogue scale (VAS), where 0 represented ‘no pain’ and 10 represented ‘most severe pain’.
All patients had an intravenous catheter inserted in a peripheral arm vein and 10 ml/kg lactated Ringer’s solution administered before commencement of spinal anesthesia.
After enrollment, patients were randomized by means of blinded opaque envelopes that had been sorted by computer-generated random allocation. Patients were allocated to one of four groups to receive 10.5, 12, 13.5, 15 mg intrathecal ropivacaine and mixed 0.5 ml 50% glucose (mixed solutions were diluted to 3 ml with normal saline).
A combined spinal-epidural technique was used with the patients in the right lateral position. After skin disinfection and infiltration with 1% lidocaine, an 18-gauged Tuohy needle was inserted into the epidural space with using the method of loss of resistance to air at the L1~L2 interspace and an epidural catheter was threaded 2~3 cm into the epidural space. The catheter was gently aspirated and checked for the presence of blood or cerebrospinal fluid, but no local anesthetics test dose was administered. Midline lumbar spinal puncture was then performed at the L3~L4 interspace by using a 25-gauge needle, and after confirming free flow of cerebrospinal fluid, mixed intrathecal ropivacaine solution was injected over 60 s. The patients were then moved to supine with left lateral tilt immediately after spinal injection.
After 20 min surgery was allowed to start if the upper dermatome level of loss of discrimination to pinprick was at or above T7. Otherwise, 1.7% alkalinized lidocaine with 1:200000 epinephrine were administered through epidural catheter in incremental doses until satisfactory dermatomal anesthesia was achieved. Patients who reported intraoperative pain (VAS>3) were treated with an intravenous bolus dose of 20 mg ketamine. If pain remained intolerable (VAS≥7) the epidural was topped up and the spinal anesthesia was defined as a failure, but data for the onset of spinal anesthesia before epidural top-up were included for analysis. Hypotension was defined by a decrease in systolic arterial pressure to less than 90 mmHg or less than 70% from baseline was treated with intravenous boluses of 5 mg ephedrine. Nausea and vomiting were treated with 4 mg ondansetron intravenously.
Postoperative analgesia was provided via patient controlled epidural analgesia (PCEA) or via epidural bolus morphine.
Measurements
The patients’ demographic variables were recorded on enrollment in the study: age, height, weight, parity, and gestational age.
Patients monitoring included pulse oximetry for hemoglobin oxygen saturation, electrocardiography for heart rate (HR) and non-invasive blood pressure (NIBP), cycled at 2 min intervals from anesthesia commencement for 15 min, at 5 min intervals until the end of surgery.
The sensory assessments were made at 2.5 min intervals for the first 30 min after spinal injection then at 15 min intervals until the end of surgery.
For assessment of the onset of anesthesia, the time for sensory block to develop to T10, T7, and maximum block height were compared. To assess the duration of the sensory block, the time for regression to T10 was compared. The motor block characteristics were assessed using maximum Bromage Score and the time elapsed from the maximum to the lowest Bromage Score.
The adverse effects including nausea, vomiting, back pain, hypotension intraoperatively and postoperatively were recorded.
Statistical analysis
All data were presented as mean±SD or frequencies where appropriate. Analysis was performed with the use of SPSS 12.0 for Windows statistical package (Chicago, IL). Data were assessed for normal distribution of variance. Means were assessed by one-way analysis of variance (ANOVA) if normally distributed, medians or non-normally distributed means were assessed by Mann-Whitney U test, and incidence data were analyzed by Fisher exact test. Statistical significance was defined as P<0.05.
The dose-response relation for spinal ropivacaine was determined using probit analysis (Khaw et al., 2001). An effective dose (success) was defined as a dose that provided adequate sensory dermatomal anesthesia to pin prick to T7 or higher required no epidural top-up for surgery to be completed.
RESULTS
All 60 patients enrolled completed the study based on the protocol and were included in the analysis. Demographic data were similar between the respective 10.5, 12, 13.5, 15 mg groups for age, weight, and height. The mean durations of surgery were also similar and there were no differences in the 1 min and 5 min neonate Apgar Scores between groups (Table 1).
Table 1.
Demographic data, surgery data, neonate Apgar Scores
| 10.5 mg (n=15) | 12 mg (n=15) | 13.5 mg (n=15) | 15 mg (n=15) | |
| Age (year) | 28.79±3.58 | 29.53±3.56 | 29.60±3.62 | 28.47±4.07 |
| Height (cm) | 160.86±3.84 | 159.20±3.73 | 160.00±3.72 | 161.01±4.25 |
| Weight (kg) | 70.39±7.65 | 68.57±6.63 | 68.87±4.89 | 66.43±6.41 |
| Duration of surgery (min) | 35.7±9.4 | 36.3±11.5 | 35.1±9.2 | 35.5±8.7 |
| 1 min Apgar Scores | 10.0±0.0 | 10.0±0.0 | 10.0±0.0 | 9.9±0.3 |
| 5 min Apgar Scores | 10.0±0.0 | 10.0±0.0 | 10.0±0.0 | 10.0±0.0 |
Values are presented as mean±SD. Compared between four groups, there were no significant differences, P>0.05
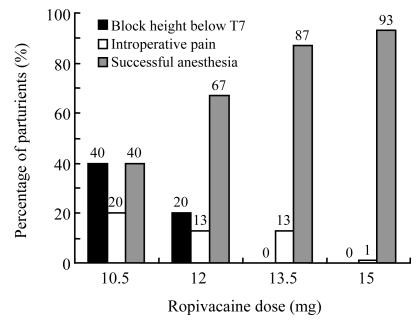
The results of anesthesia outcomes are illustrated in Fig.1. Of the 60 patients in this study, 43 patients (71.7%) completed surgery successfully under spinal anesthesia alone according to the criteria of anesthesia success described above of that there were 6 (40%), 10 (66.7%), 13 (86.7%), 14 (93.3%) patients in the 10.5-, 12-, 13.5-, 15-mg groups, respectively. And 8 (13.3%) patients [6 (40.0%), 3 (20.0%), 0, 0 cases in the 10.5-, 12-, 13.5-, 15-mg groups, respectively] whose upper dermatomal level of sensory anesthesia to pin prick was below T7 were needed epidural top-up before commence of surgery. And 9 patients (15%) [3 (20.0%), 2 (13.3%), 2 (13.3%), 1 (6.7%) cases in the 10.5-, 12-, 13.5-, 15-mg groups, respectively] experienced intraoperative pain and were not relieved by i.v. ketamine.
Fig. 1.
Anesthetic outcome for all patients
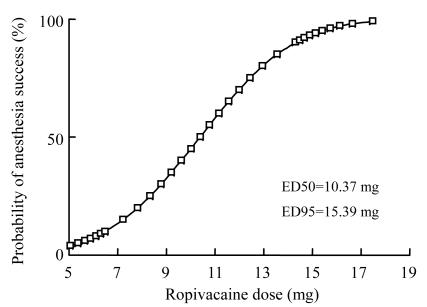
Logistic regression plots using Probit analysis were drawn for spinal anesthesia success in Fig.2. The ED50 (95% confidence interval) was 10.37 (5.23~11.59) mg, ED90 was 14.29 (13.03~19.81) mg, and ED95 was 15.39 (13.81~23.59) mg. Linear regression plot of the probit value against the log using linear regression analysis are drawn in Fig.2 showing a regression coefficient (r) of 0.995 (P<0.001).
Fig. 2.
Logistic regression plot of anesthesia success: calculation of ED50 and ED95
Block characteristics are given in Table 2. There was no significant difference regarding onset of sensory block to T10 between the 4 groups, and there was a statistically significant difference regarding onset of sensory block to T7 (P<0.05) which was not correlated to the ropivacaine dose. The maximum sensory block (dermatome) had significant correlation to ropivacaine dose (R 2=0.17, P=0.01) with the 15-mg group having the highest block. There was no difference of maximum motor block (Bromage Score) between the 4 groups (P>0.05), and the duration motor block (the time from the maximum to the lowest Bromage Score) was correlated to ropivacaine significantly (R 2=0.295, P<0.001).
Table 2.
Characteristics of sensory and motor blocks
| 10.5 mg (n=15) | 12 mg (n=15) | 13.5 mg (n=15) | 15 mg (n=15) | |
| Sensory block | ||||
| Onset to T10 (min) | 2.54±1.120 | 3.30±2.030 | 2.10±1.330 | 2.59±1.290 |
| Onset to T7 (min) | 7.38±2.670 | 8.13±2.070 | 6.13±1.87* | 6.53±3.070 |
| Median maximum block (dermatome) | T6.13±0.350 | T5.60±0.520 | T5.40±0.740 | T5.20±0.86* |
| Time to regression to T10 (min) | 46.00±12.05 | 52.33±13.60 | 62.73±19.80 | 73.40±18.59 |
| Motor block | ||||
| Max motor block (Bromage Score) | 2.87±0.350 | 2.80±0.410 | 2.87±0.350 | 2.93±0.260 |
| Duration of motor block (min) | 58.67±21.38 | 64.67±19.45 | 76.53±24.53 | 94.20±17.95 |
Values are presented as mean±SD
P<0.05, when compared with the other three groups
For the occurrence of nausea/vomiting, there were no significant differences between the 4 groups. However, there was a statistically significant correlation between ropivacaine dose and the rate of hypotension (6, 3, 2 and 0 cases in the 10.5-, 12-, 13.5-, 15-mg groups, respectively) (R 2=0.939, P<0.001). No patients had post-dural puncture headache and residual neurologic changes or back pain on the first and second day after surgery.
DISCUSSION
In this study we found the ED50 and ED95 (95% confidence interval) for intrathecal hyperbaric ropivacaine used in cesarean section based on a wide range of different doses linearly distributed were 10.37 (5.23~11.59) mg and 15.39 (13.81~23.59) mg. However, it should be noted that the ED50 and ED95 of ropivacaine reported in other studies seems to be higher than the ED50 and ED95 found in our study. Khaw et al.(2001) determined the ED50 and ED95 of plain ropivacaine for obstetrical patients in similar clinical settings and using the same dose to be 16.7 mg and 26.8 mg. Celleno et al.(2005) showed the ED50 of plain ropivacaine for cesarean section using up-down sequential method to be 14.22 mg. Wong et al.(2003) suggested that either 18.75 mg or 22.5 mg 0.75% glucose free ropivacaine can provide spinal anesthesia of the same efficacy and safety for cesarean section in Chinese parturients. This difference may be due to several factors.
First, the density of spinal solutions of ropivacaine may be the main factor. The ropivacaine solution used in this study was hyperbaric whereas the other study’s solutions shown above were plain or hypobaric. It was shown that the baricity of injectate and position of the patient primarily determine the spread of intrathecal local anesthetics (Greene, 1985; Connolly and Wildsmith, 1998). Usually, glucose-free solutions are marginally hypobaric and have been found previously to be ‘unpredictably’ (Logan et al., 1986) spread. Many studies (Fettes et al., 2005; Whiteside et al., 2001; Kallio et al., 2004) showed that hyperbaric solutions of local anesthetics for spinal anesthesia produce a more rapid spread to a higher median level and less variation in maximum sensory and motor block and might enable a smaller dose to be used compared with plain solutions. Especially in pregnant women, the width of the hips is usually larger than the shoulders which result in a head-down tilt when lying in the lateral position (Khaw et al., 2002). By the way, compared with the results obtained by Khaw and colleagues and taking our results into account, the addition of glucose allows a reduction of nearly one third of the dose of ropivacaine required for the ED95 used in cesarean section.
Second, because different statistical methodologies and end-points for adequate block which may influence the results of ED50 and ED95 of spinal anesthetics were used in different study, for example Celleno et al.(2005) used the sequential allocation method which showed ED50 to be 14.22 mg. It is difficult to make a direct comparison between estimates ED50 and ED95 of ropivacaine from different studies so more research must be conducted.
Third, in this study, the duration of surgery was less than 40 min which may be significantly shorter than the experience reported in some other study. And the duration of surgery was within the duration of spinal anesthesia of ropivacaine, thus, the rate of feeling intraoperative pain is lower than that reported in other studies.
With the three factors above, we may understand that the success rate of spinal ropivacaine anesthesia in this study was higher and the ED50 and ED95 of spinal hyperbaric ropivacaine are lower than that shown in some other reports.
Interestingly, we found that there was a statistically significant difference of the maximum sensory block (dermatome) between the 4 groups, and that the maximum sensory block had a significant correlation to ropivacaine dose (R 2=0.17, P<0.01). This finding is different from Khaw et al.(2001)’s finding which showed no difference in the maximum height of sensory block despite a difference in success rates among different ropivacaine dose. It has been proposed that to achieve optimum conditions for cesarean section one should aim to achieve an upper level of sensory anesthesia of T4 (Reisner and Lin, 1999; Glosten, 2000). But in our present study, there were no patients who experienced intraoperative pain if the upper level of sensory block reached T7, so it may be concluded that upper sensory block to T7 is an optimum anesthesia level which can provide good condition for cesarean section.
We have shown in this study that a dose-dependent relation exist between the duration of sensory [time to regression to T10 (min)], motor block, and the success rate of spinal anesthesia for cesarean section. There was no significant difference regarding onset of sensory block to T10 but a significant difference of onset to T7.
Ginosar et al.(2004) suggested that the ideal dose of intrathecal local anesthetic for cesarean delivery strikes a perfect balance between the conflicting demands of avoiding patient discomfort and avoiding adverse maternal effects (particularly hypotension and nausea). Pedersen et al.(1989) demonstrated that increasing the dose of intrathecal local anesthetic reduced the incidence and severity of visceral pain without increasing maternal hypotension. However, many other studies found that increasing the dose of local anesthetic increased maternal hypotension (Kang et al., 1998; Ben-David et al., 2000). We found in this study that there was a dose-dependent relation between the rate of hypotension and the ropivacaine dose, whereas there was no significant difference of nausea/vomiting among the 4 groups.
We did not record any postoperative neurologic changes or back pain on the first and second day after surgery. It may be concluded that ropivacaine is suitable for spinal anesthesia.
References
- 1.Ben-David B, Miller G, Gavriel R, Gurevitch A. Low-dose bupivacaine-fentanyl spinal anesthesia for cesarean delivery. Reg Anesth Pain Med. 2000;25(3):235–239. doi: 10.1016/S1098-7339(00)90004-X. [DOI] [PubMed] [Google Scholar]
- 2.Celleno D, Parpaglioni R, Frigo MG, Barbati G. Intrathecal levobupivacaine and ropivacaine for cesarean section. Minerva Anestesiol. 2005;71:521–525. [PubMed] [Google Scholar]
- 3.Connolly C, Wildsmith JA. Intrathecal drug spread. Can J Anaesth. 1998;45:289–292. doi: 10.1007/BF03012016. [DOI] [PubMed] [Google Scholar]
- 4.Fassoulaki A, Gatzou V, Petropoulos G, Siafaka I. Spread of subarachnoid block, intraoperative local anaesthetic requirements and postoperative analgesic requirements in Caesarean section and total abdominal hysterectomy. Br J Anaesth. 2004;93(5):678–682. doi: 10.1093/bja/aeh258. [DOI] [PubMed] [Google Scholar]
- 5.Fettes PD, Hocking G, Peterson MK, Luck JF, Wildsmith JAW. Comparison of plain and hyperbaric solutions of ropivacaine for spinal anaesthesia. Br J Anaesth. 2005;94(1):107–111. doi: 10.1093/bja/aei008. [DOI] [PubMed] [Google Scholar]
- 6.Gautier P, de Kock M, Huberty L, Demir T, Izydorczic M, Vanderick B. Comparison of the effects of intrathecal ropivacaine, levobupivacaine, and bupivacaine for caesarean section. Br J Anaesth. 2003;91(5):684–689. doi: 10.1093/bja/aeg251. [DOI] [PubMed] [Google Scholar]
- 7.Ginosar Y, Mirikatani E, Drover DR, Cohen SE, Riley ET. ED50 and ED95 of intrathecal hyperbaric bupivacaine coadministered with opioids for cesarean delivery. Anesthesiology. 2004;100:676–682. doi: 10.1097/00000542-200403000-00031. [DOI] [PubMed] [Google Scholar]
- 8.Glosten B. Anesthesia. 5th Ed. New York: Churchill Livingstone; 2000. Anesthesia for Obstetrics; p. 2049. [Google Scholar]
- 9.Greene NM. Distribution of local anesthetic solutions within the subarachnoid space. Anesth Analg. 1985;64(7):715–730. doi: 10.1213/00000539-198507000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Kallio H, Snall EVT, Tuomas CA, Rosenberg PH. Comparison of hyperbaric and plain ropivacaine 15 mg in spinal anaesthesia for lower limb surgery. Br J Anaesth. 2004;93(5):664–669. doi: 10.1093/bja/aeh257. [DOI] [PubMed] [Google Scholar]
- 11.Kang FC, Tsai YC, Chang PJ, Chen TY. Subarachnoid fentanyl with diluted small-dose bupivacaine for cesarean section delivery. Acta Anaesthesiol Sin. 1998;36:207–214. [PubMed] [Google Scholar]
- 12.Khaw KS, Ngan KW, Wong ELY, Liu JYW, Chung R. Spinal ropivacaine for cesarean section: a dose-finding study. Anesthesiology. 2001;95:1346–1350. doi: 10.1097/00000542-200112000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Khaw KS, Ngan Kee W, Wong M, Floria N, Lee A. Spinal ropivacaine for cesarean delivery: a comparison of hyperbaric and plain solutions. Anesth Analg. 2002;94:680–685. doi: 10.1097/00000539-200203000-00037. [DOI] [PubMed] [Google Scholar]
- 14.Logan MR, McClure JH, Wildsmith JAW. Plain bupivacaine an unpredictable spinal anaesthetic agent. Br J Anaesth. 1986;58:292–296. doi: 10.1093/bja/58.3.292. [DOI] [PubMed] [Google Scholar]
- 15.Pedersen H, Santos AC, Steinberg ES, Schapiro HM, Harmon TW, Finster M. Incidence of visceral pain during cesarean section: the effect of varying doses of spinal bupivacaine. Anesth Analg. 1989;69(1):46–49. doi: 10.1213/00000539-198907000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Reisner LS, Lin D. Anesthesia for Cesarean Section, Obstetric Anesthesia: Principles and Practice. 2nd Ed. St. Louis, Mosby: 1999. p. 475. [Google Scholar]
- 17.Whiteside JB, Burke D, Wildsmith JAW. Spinal anaesthesia with ropivacaine 5 mg/ml in glucose 10 mg/ml or 50 mg/ml. Br J Anaesth. 2001;86(2):241–244. doi: 10.1093/bja/86.2.241. [DOI] [PubMed] [Google Scholar]
- 18.Wong JO, Tan TD, Leung PO. Spinal anesthesia with two different dosages of 0.75% glucose-free ropivacaine: a comparison of efficacy and safety in Chinese parturients undergoing cesarean section. Acta Anaesthesiol Sin. 2003;41:131–138. [PubMed] [Google Scholar]