Nearly three quarters of cases of tuberculosis, HIV, and malaria reported in England, Wales, and Northern Ireland in 2004 were in people born outside the United Kingdom. This is the finding of a report on infectious diseases among migrants published by the UK Health Protection Agency.
The report analysed surveillance data for 2004 on a variety of infections in people born outside the UK. It showed that 70% of cases of tuberculosis and HIV reported in England, Wales, and Northern Ireland were in people born outside the UK. It also said that 70% of cases of malaria reported throughout the United Kingdom in 2004 were in people born outside the UK.
Most of the newly recorded cases of chronic hepatitis B in England and Wales were also in people not born in the UK.
Jane Jones, a consultant epidemiologist and head of the travel and migrant health section of the Health Protection Agency's Centre for Infections and one of the report's authors, said: “Migrants clearly have a disproportionate burden of infectious diseases.”
However, she added, “This must be seen in context: most migrants do not have these diseases. Most are healthy young adults who have come to the UK mainly to work or study.”
There is little evidence that the general population is at risk of catching disease from affected migrants, she said, although the data indicated that some people from ethnic minorities who were born in the UK may be at a higher risk. “Migrants may also continue to be at risk of infectious diseases after they have arrived in the UK, either because of exposure here or as a result of travel back to their country of origin.”
The report recommends strengthening the provision of culturally appropriate and language supported health services; increasing awareness of disease among migrant communities, people with ethnic links to migrant communities, and their healthcare practitioners; and improving surveillance systems.
Resources to support health professionals in managing the health care of patients born outside the UK should be further developed, it says. In particular, professionals in primary care should be given support to assess the range of immigrants' health needs, including those associated with infectious diseases.
Provision of an extended new check of patients in some groups of new entrants should be considered, the report says, but the risk of infectious disease should be assessed on an ongoing basis.
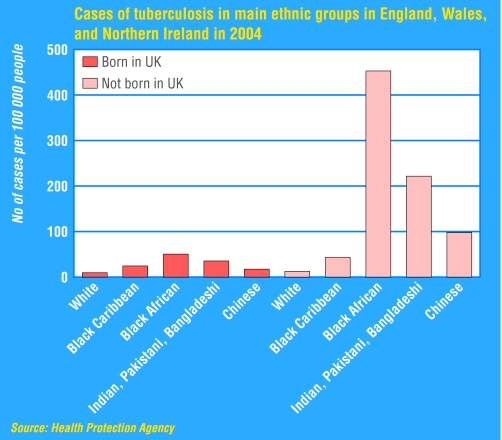
The detailed findings showed that 70% of the 6560 people in England, Wales, and Northern Ireland in 2004 who were given a diagnosis of tuberculosis and whose country of origin was known were born abroad. Nearly half (45%) came from southern Asia and 39% came from sub-Saharan Africa.
People with tuberculosis who were born abroad were generally less likely to have pulmonary (potentially infectious) disease than people with the disease who had been born in the UK, although the likelihood varied with country of birth.
People who had recently arrived in the UK were more likely to have tuberculosis than people who had been in the country longer, but most cases of tuberculosis were diagnosed two years or more after arrival. A further finding was that ethnic minority people who were born in the UK had a higher risk of tuberculosis than people not from ethnic minorities and that there was some evidence for recent transmission in this group.
The report recommends that healthcare professionals be alert to the higher risk of tuberculosis among people who were not born in the UK, even if they had lived in the UK for a long time. Primary care professionals should be supported in controlling tuberculosis in people not born in the UK, and the government should evaluate the possible benefit to public health of screening programmes for tuberculosis.
About 70% of the 4253 people in England, Wales, and Northern Ireland who were given a diagnosis of HIV in 2004 and whose country of birth was known were born outside the UK. Ninety per cent were born in sub-Saharan Africa, and around 85% of these people were thought to have become infected in Africa.
The report says that most of these cases were probably acquired through heterosexual contact. Among people born outside the UK, more heterosexual women than heterosexual men have had a diagnosis of HIV since the start of the HIV epidemic.
People born outside the UK were at risk of starting treatment too late, the report says. Up to 10% of heterosexual people born outside the UK did not start antiretroviral treatment at the appropriate time in the course of their HIV infection.
Awareness of HIV and AIDS needs to be higher in groups of people with a risk of HIV infection, the report suggests, and their healthcare professionals should be encouraged to try to make early diagnoses among their patients.
Department of Health guidelines on antenatal screening for HIV should be followed for all pregnant women, it says. Improvements to routine HIV surveillance should include better capture of information on patients' country of birth and socioeconomic status.
Migrant Health: Infectious Diseases in Non-UK Born Populations in England, Wales and Northern Ireland. A Baseline Report—2006 is accessible at www.hpa.org.uk.