Abstract
After one year Edinburgh's Community Drug Problem Service has shown that if psychiatric services offer consultation and regular support for drug users many general practitioners will share the care of such patients and prescribe for them, under contract conditions, whether the key worker is a community psychiatric nurse or a drug worker from a voluntary agency. This seems to apply whether the prescribing is part of a "harm reduction" strategy over a long period or whether it is a short period of methadone substitution treatment. Given the 50% prevalence of HIV infection among drug users in the Edinburgh area and the fact that only half of them have been tested for seropositivity, the health and care of this demanding group of young people with a chaotic lifestyle are better shared among primary care, community based drug workers, and specialist community drugs team than treated exclusively by a centralised hospital drug dependency unit. As the progression to AIDS is predictable in a larger proportion of drug users who are positive for HIV, there is an even greater need for coordinated care between specialists and community agencies in the near future.
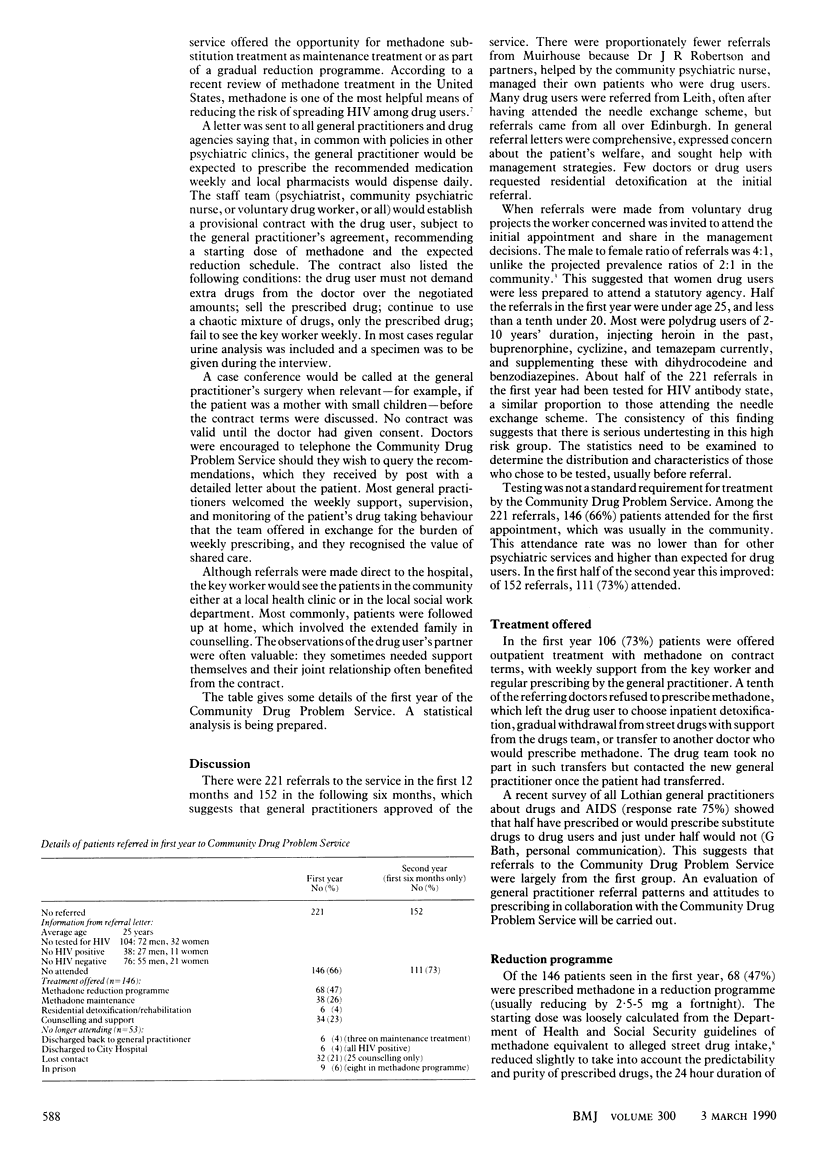
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cooper J. R. Methadone treatment and acquired immunodeficiency syndrome. JAMA. 1989 Sep 22;262(12):1664–1668. [PubMed] [Google Scholar]
- Robertson J. R., Bucknall A. B., Welsby P. D., Roberts J. J., Inglis J. M., Peutherer J. F., Brettle R. P. Epidemic of AIDS related virus (HTLV-III/LAV) infection among intravenous drug abusers. Br Med J (Clin Res Ed) 1986 Feb 22;292(6519):527–529. doi: 10.1136/bmj.292.6519.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson J. R. Drug users in contact with general practice. Br Med J (Clin Res Ed) 1985 Jan 5;290(6461):34–35. doi: 10.1136/bmj.290.6461.34. [DOI] [PMC free article] [PubMed] [Google Scholar]



