Abstract
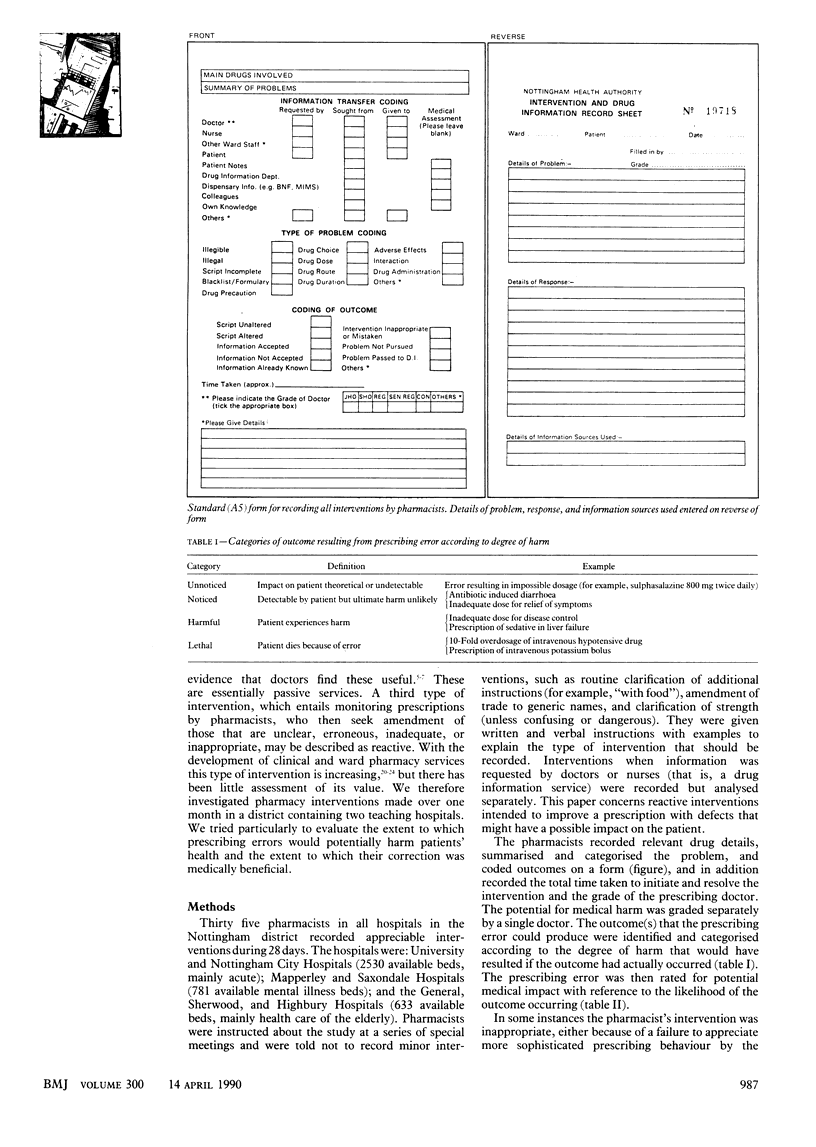
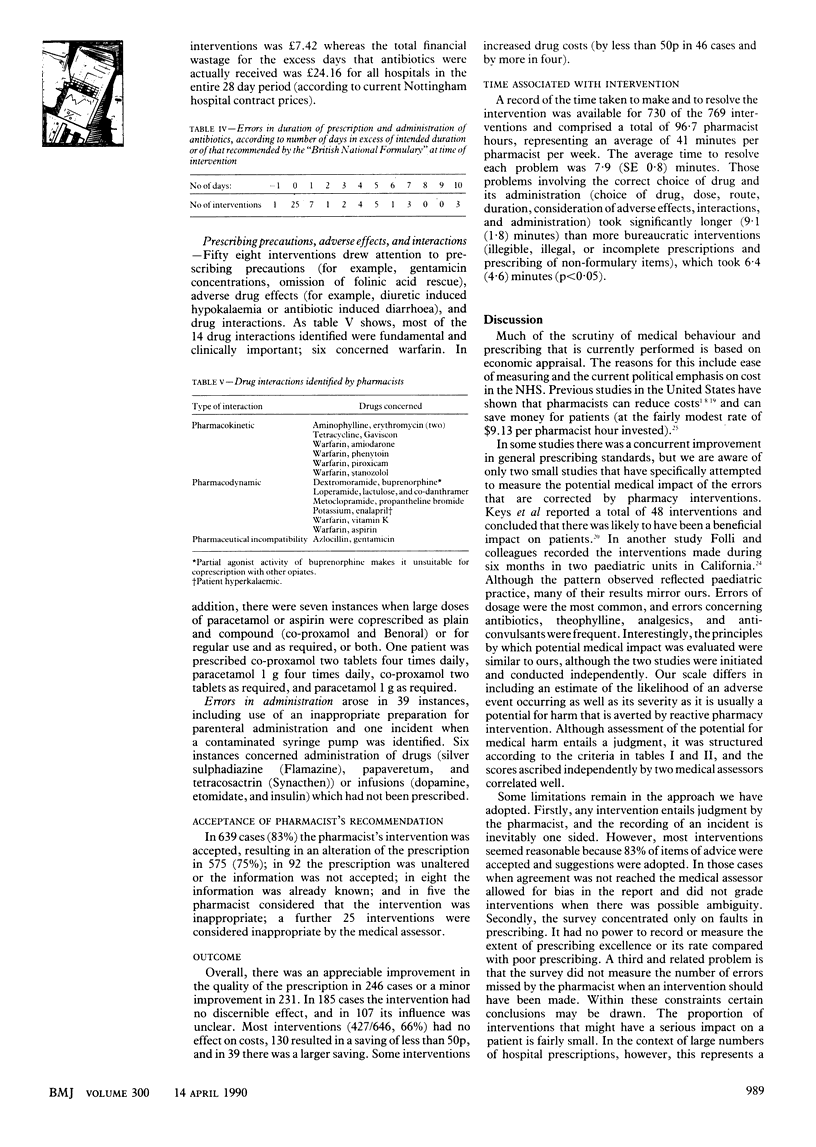
OBJECTIVE--To evaluate the medical impact of reactive pharmacy intervention. DESIGN--Analysis of all interventions during 28 days by all 35 pharmacists in hospitals in Nottingham. SETTING--All (six) hospitals in the Nottingham health authority (a teaching district), representing 2530 mainly acute beds, 781 mental illness beds, and 633 mainly health care of the elderly beds. PATIENTS--Hospital inpatients and outpatients. INTERVENTIONS--Recording of every important intervention made by pharmacists to prescriptions for both inpatients and outpatients when they perceived inadequacies of drug prescription or administration, including characterisation of the problem, coding of outcome, recording of time taken to initiate and resolve intervention, and grade of prescribing doctor. The problems were independently assessed for their potential to cause medical harm. RESULTS--769 Interventions (about 2.9% of prescriptions) were made, of which 60 concerned prescriptions rated as having a major potential for medical harm. The commonest problems concerned dosage, which was wrong in 280 prescriptions (102 for antibiotics) and not stated in 50 (one for antibiotics), especially those associated with a major potential for medical harm (32 prescriptions). These concerned sedatives; analgesics; cardiovascular drugs or diuretics; and iron, vitamin, or mineral preparations. Also common were overprolonged prescription of antibiotics (48 prescriptions), confusion of drug names (nine), and inadvertent coprescription of excessive quantities of aspirin or paracetamol in plain and compound preparations (seven). The pharmacist's recommendation was accepted in 639 instances (86%), and the prescription was altered in 575, leading to an appreciable (246 cases) or minor (231 cases) improvement. Interventions had little effect on costs; 427/646 had no effect and 130 produced savings less than 50p. Pharmacy intervention (730/769 interventions) occupied on average 41 minutes per pharmacist per week. CONCLUSIONS--Most reactive pharmacy interventions concerned prescribing errors with a limited potential for medical harm, but a small number of detected errors with a major potential for medical harm; cost savings were not appreciable.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alexander M. R., Alexander B., Mustion A. L., Spector R., Wright C. B. Therapeutic use of albumin: 2. JAMA. 1982 Feb 12;247(6):831–833. [PubMed] [Google Scholar]
- Avorn J., Soumerai S. B. Improving drug-therapy decisions through educational outreach. A randomized controlled trial of academically based "detailing". N Engl J Med. 1983 Jun 16;308(24):1457–1463. doi: 10.1056/NEJM198306163082406. [DOI] [PubMed] [Google Scholar]
- Azad Khan A. K., Howes D. T., Piris J., Truelove S. C. Optimum dose of sulphasalazine for maintenance treatment in ulcerative colitis. Gut. 1980 Mar;21(3):232–240. doi: 10.1136/gut.21.3.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berbatis C. G., Maher M. J., Plumridge R. J., Stoelwinder J. U., Zubrick S. R. Impact of a drug bulletin on prescribing oral analgesics in a teaching hospital. Am J Hosp Pharm. 1982 Jan;39(1):98–100. [PubMed] [Google Scholar]
- Comer J. B. Documenting pharmacists' interventions. Am J Hosp Pharm. 1985 Mar;42(3):625–626. [PubMed] [Google Scholar]
- Evans C. E., Haynes R. B., Birkett N. J., Gilbert J. R., Taylor D. W., Sackett D. L., Johnston M. E., Hewson S. A. Does a mailed continuing education program improve physician performance? Results of a randomized trial in antihypertensive care. JAMA. 1986 Jan 24;255(4):501–504. [PubMed] [Google Scholar]
- Folli H. L., Poole R. L., Benitz W. E., Russo J. C. Medication error prevention by clinical pharmacists in two children's hospitals. Pediatrics. 1987 May;79(5):718–722. [PubMed] [Google Scholar]
- Hayman J. N., Brown T. R., Smith M. C., Liao W. Physician use and evaluation of a hospital-based drug information center. Am J Hosp Pharm. 1978 Oct;35(10):1238–1240. [PubMed] [Google Scholar]
- Keys P. W., South J. C., Duffy M. G. Quality of care evaluation applied to assessment of clinical pharmacy services. Am J Hosp Pharm. 1975 Sep;32(9):897–902. [PubMed] [Google Scholar]
- Klotz R., Steffens S. Improved pharmacy services through pharmacist participation in medical rounds. Am J Hosp Pharm. 1976 Apr;33(4):349–351. [PubMed] [Google Scholar]
- Mutchie K. D., Smith K. A., MacKay M. W., Marsh C., Juluson D. Pharmacist monitoring of parenteral nutrition: clinical and cost effectiveness. Am J Hosp Pharm. 1979 Jun;36(6):785–787. [PubMed] [Google Scholar]
- Noel M. W., Paxinos J. Cephalosporins: use review and cost analysis. Am J Hosp Pharm. 1978 Aug;35(8):933–935. [PubMed] [Google Scholar]
- Norris S. M. Evaluation of gentamicin prescribing after drug-use review. Am J Hosp Pharm. 1982 Sep;39(9):1529–1530. [PubMed] [Google Scholar]
- Ray W. A., Blazer D. G., 2nd, Schaffner W., Federspiel C. F., Fink R. Reducing long-term diazepam prescribing in office practice. A controlled trial of educational visits. JAMA. 1986 Nov 14;256(18):2536–2539. [PubMed] [Google Scholar]
- Ryan P. B., Johnson C. A., Rapp R. P. Economic justification of pharmacist involement in patient medication consultation. Am J Hosp Pharm. 1975 Apr;32(4):389–392. [PubMed] [Google Scholar]
- Schloemer J. H., Zagozen J. J. Cost analysis of an aminoglycoside pharmacokinetic dosing program. Am J Hosp Pharm. 1984 Nov;41(11):2347–2351. [PubMed] [Google Scholar]
- Seligman S. J. Reduction in antibiotic costs by restricting use of an oral cephalosporin. Am J Med. 1981 Dec;71(6):941–944. doi: 10.1016/0002-9343(81)90304-1. [DOI] [PubMed] [Google Scholar]
- Shane R., Miller J., Cohen J. Educating hospital decision-makers about pharmacists' intervention. Am J Hosp Pharm. 1985 Sep;42(9):1928–1934. [PubMed] [Google Scholar]
- Sohn C. A., Wolter H. A., McSweeney G. W. Effectiveness of a cephalosporin education program--a pharmacy education program. Drug Intell Clin Pharm. 1980 Apr;14(4):272–277. doi: 10.1177/106002808001400406. [DOI] [PubMed] [Google Scholar]



