Abstract
Background
To assess balance in single-limb stance, center of pressure movements can be registered by stabilometry with force platforms. This can be used for evaluation of injuries to the lower extremities. It is important to ensure that the assessment tools we use in the clinical setting and in research have minimal measurement error. Previous studies have shown that the ability to maintain standing balance is decreased by fatiguing exercise. There is, however, a need for further studies regarding possible effects of general exercise on balance in single-limb stance. The aims of this study were: 1) to assess the test-retest reliability of balance variables measured in single-limb stance on a force platform, and 2) to study the effect of exercise on balance in single-limb stance, in healthy subjects.
Methods
Forty-two individuals were examined for test-retest reliability, and 24 individuals were tested before (pre-exercise) and after (post-exercise) short-duration, sub-maximal cycling. Amplitude and average speed of center of pressure movements were registered in the frontal and sagittal planes. Mean difference between test and retest with 95% confidence interval, the intraclass correlation coefficient, and the Bland and Altman graphs with limits of agreement, were used as statistical methods for assessing test-retest reliability. The paired t-test was used for comparisons between pre- and post-exercise measurements.
Results
No difference was found between test and retest. The intraclass correlation coefficients ranged from 0.79 to 0.95 in all stabilometric variables except one. The limits of agreement revealed that small changes in an individual's performance cannot be detected. Higher values were found after cycling in three of the eight stabilometric variables.
Conclusions
The absence of systematic variation and the high ICC values, indicate that the test is reliable for distinguishing among groups of subjects. However, relatively large differences in an individual's balance performance would be required to confidently state that a change is real. The higher values found after cycling, indicate compensatory mechanisms intended to maintain balance, or a decreased ability to maintain balance. It is recommended that average speed and DEV 10; the variables showing the best reliability and effects of exercise, be used in future studies.
Background
Fatigue is caused by a combination of different physiological mechanisms occurring at both the central and peripheral levels, leading to decreased motor control [1]. It is therefore reasonable to hypothesize that fatiguing exercise will have an effect on postural control. The maintenance and control of posture and balance in a particular position, or during movement, are fundamental for physical activity. The somatosensory, visual and vestibular systems, as well as the muscle activity, contribute to the maintenance of postural control. This is a person's ability to maintain an appropriate relationship between the body segments and between the body and the environment, and to keep the body's center of mass over the base of support when performing a task [2]. To evaluate postural control in stance, center of pressure (CP) movements can be registered by stabilometry with force platforms [3].
Some authors have reported a decrease in ability to maintain balance in bilateral stance [4-6], and single-limb stance [6-8] after fatiguing exercise, and it has been suggested that individuals are therefore at increased risk of injury when fatigued [6-8]. However, others have found no effect of fatiguing exercise on postural control in single-limb stance [9-11]. In the above-mentioned studies, fatigue was induced by exercise of the lower extremities [6-8,10,11], or by general fatigue [4,5,9]. Fatigue induced by general exercise, such as cycling, running or walking, better resembles conditions in daily life and physical activities than fatigue induced by exercising the lower extremities isolated in an isokinetic device. Studies of balance in single-limb stance are of importance since movement patterns of postural control are similar during the stance phase, and many injuries to the lower extremities occur during weight-bearing on one leg [12]. The effect of general fatigue on balance in single-limb stance in healthy subjects has, to our knowledge, only been investigated in one study [9]. Therefore, there is a need for further studies regarding possible effects of fatigue induced by general exercise on postural control, measured by balance in single-limb stance.
It is important to ensure that the assessment tools we use in the clinical setting and in research have measurement error small enough (i.e. high reliability) to detect actual changes in what is being measured. The two components of measurement error are systematic bias, e.g., learning or fatigue effects on the test, and random error due to inherent subject or instrument variation [13]. There is a lack of consensus regarding which statistical tests are the most appropriate for use in reliability studies [13]. Several studies have used the intraclass correlation coefficient (ICC) as a statistical method for assessing test-retest reliability on force platforms [14-16]. However, the ICC has disadvantages; e.g., large variation between subjects results in high ICC values [13], and the ICC provides a value between 0 and 1 ("relative reliability"), which is difficult to interpret clinically. Therefore, it has been recommended that the ICC be complemented by calculations expressing the actual units of measurement ("absolute reliability"), such as the Bland and Altman graphs with limits of agreement (LOA), and the paired t-test or mean difference between test and retest with a 95% confidence interval (CI), to assess whether there is a statistically significant bias between the tests (systematic change in the mean) [13]. If several reliability statistics are used; i.e., relative reliability, absolute reliability and analysis of systematic change in the mean, this may provide us with sufficient information about the reliability of the assessment tool.
The purposes of the present study were: 1) to assess the test-retest reliability of balance in single-limb stance measured by stabilometry on a force platform as used in previous studies [3,16-19], and 2) to study the effect of short-duration, sub-maximal cycle ergometry, a standardized method of inducing fatigue [20], on balance in single-limb stance in healthy subjects.
Methods
Subjects
Two groups of healthy volunteers (group 1 and group 2), with no history of neurological disease, major orthopedic lesions, vestibular or visual disturbance were included in the study. Group 1: Forty-two subjects (22 men and 20 women) were included in the test-retest reliability part of the study. Their mean age was 24 years (SD 3 years), mean height 176 cm (SD 8 cm), mean weight 69 kg (SD 10 kg), and median activity level 5 (range 2 to 7) according to the Tegner activity level scale, equal to heavy work or recreational jogging on uneven ground twice or more per week [21]. Group 2: Twenty-four subjects (11 men and 13 women) were included in the part of the study regarding the effect of general exercise. Their mean age was 24 years (SD 3 years), mean height 176 cm (SD 8 cm), and mean weight 71 kg (SD 13 kg), and median activity level 5 (range 2 to 9) according to the Tegner activity level scale. The physical activity and age distribution of the subjects in this study were chosen in order to match patients with ligament injuries in the knee. The Research Ethics Committee at Lund University approved the study. All subjects gave their written informed consent to participate in the study.
Assessment
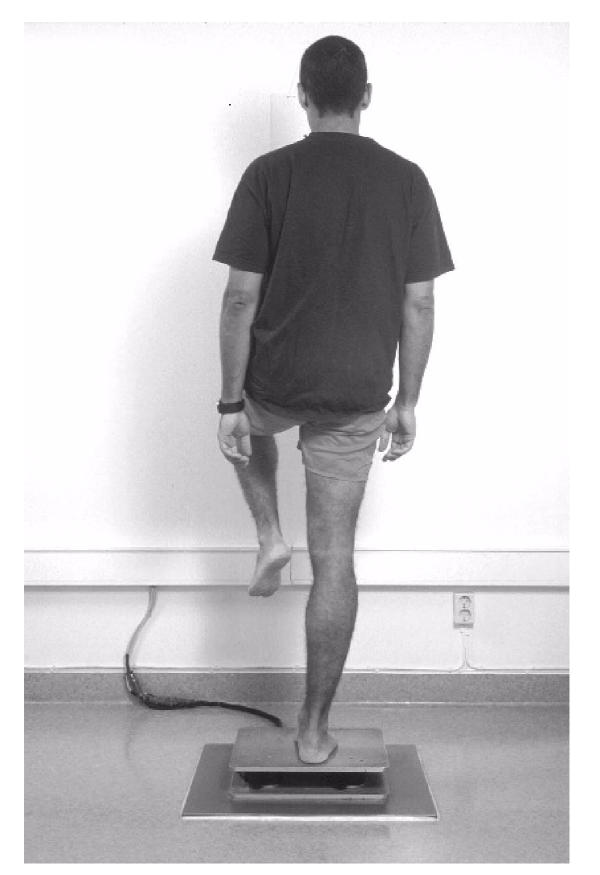
Stabilometry (group 1 and group 2)
Balance in single-limb stance was tested by means of a strain gauge force plate (33 × 38 cm) with the subject barefoot in a standardized position [3,16-19] (Figure 1). One foot was placed pointing straight forward in relation to reference lines in the frontal and sagittal planes. The other leg was flexed 90° at the hip and knee joints with both arms hanging relaxed at the sides. The subjects were instructed to stand as motionless as possible, looking straight ahead at a point on the wall 65 cm away; they were allowed to practice maintaining this position for about 20 s before three measurements were made on each leg, with the subjects standing alternately on their right and left leg. The test order between legs was randomized. Accordingly, the assessment included three measurements taken on the right leg and three on the left leg, giving a total of six measurements on each test occasion. These six measurements lasted for approximately 3.5 minutes. If single-limb balance was not maintained for 25 seconds, the trial was not recorded and the measurement was repeated. However, all subjects in the present study successfully completed the measurements. Movements of the center of pressure (CP) in the frontal plane (FP) and sagittal plane (SP) were recorded for 25 s at a sampling frequency of 20 Hz. In bilateral stance, a frequency of CP below 1–3 Hz has been found in healthy subjects [22]. A center frequency value of CP below 2 Hz has been observed in single-limb stance in the frontal plane in uninjured subjects and in individuals with functional instability of the ankle [23]. We have found no reports on the frequency of CP in single-limb stance in the sagittal plane. However, according Winter [22] the frequency of CP is lower in the sagittal plane than in the frontal plane. Thus, it is reasonable to assume that a sampling frequency of 20 Hz is appropriate for measuring CP movements in single-limb stance. It cannot, however, be excluded that CP movements at higher frequencies than those that can be recorded at a sampling rate of 20 Hz may exist. A computer program (Viewdac 2.1, Keithley Instruments, Inc., Cleveland, Ohio, USA), was used to analyze the following variables: 1) standard deviation of the mean value of CP movements in mm, reflecting the amplitude of CP movements (amplitude); 2) average speed of CP movements in mm·s-1; 3) number of movements exceeding 5 mm from the mean value of CP (DEV 5); and 4) number of movements exceeding 10 mm from the mean value of CP (DEV 10), giving a total of eight variables (four variables in each plane). The mean value of CP is the distance (mm) between the CP and the reference lines, and the amplitude (mm) is its standard deviation. The average speed (mm·s-1) reflects the amplitude and frequency of CP movements, and is calculated as the total length of the path of CP divided by the test trial time. DEV 5 is the number of movements exceeding 5 mm but less than or equal to 10 mm from the mean value of CP, and DEV 10 is the number of movements exceeding 10 mm from the mean value of CP. DEV 5 and DEV 10 reflect the amplitude of CP (i.e., displacement of CP).
Figure 1.
Stabilometry in single-limb stance, tested by means of a strain gauge force plate. A standardized position was used. The subject is a model who did not participate in the study.
The subjects in group 1 were tested twice (test 1 and test 2), at about the same time of day with an interval of approximately one week, median value 7 days (range 4–7 days). As previously mentioned, three measurements were made on each leg. The median value of these three measurements was used in the test-retest reliability analyses. The subjects in group 2 were tested before (pre-exercise) and immediately after completion of short-duration, sub-maximal cycling (post-exercise). The median value of the three measurements and the first and third of the three post-exercise measurements were used in the analyses.
Short-duration sub-maximal exercise (group 2 only)
Short-duration, sub-maximal exercise was performed on a cycle ergometer. The subjects wore a heart-rate meter during the entire duration of the assessment. Borg's scale for Rating of Perceived Exertion (RPE) [24] was used to assess the subjective effort level during exercise. On this scale, numbers ranging from 6 to 20 are matched with descriptors (e.g., 6 = No exertion at all, 13 = Somewhat hard, 15 = Hard, 17 = Very hard, 19 = Extremely hard, and 20 = Maximal exertion). The RPE scale was designed to increase linearly with exercise intensity and heart rate while exercising on a bicycle ergometer, and correlates closely with several physiological variables, including heart rate and blood lactate concentration [24]. A linear relationship exists between heart rate and oxygen consumption with increasing rates of work. A given percentage of maximum oxygen consumption (VO2max) results in a higher percentage of maximum heart rate (HRmax); e.g., 75% of VO2max represents an intensity of 86% of the HRmax [25]. HRmax can be predicted from the following equation:
Maximum heart rate (beats/min) = 220 - age (years) [25].
Reductions in concentrations of adenosine triphosphate (ATP) and creatine phosphate (CP) in muscle, and large increases in muscle and blood lactate concentrations have been observed after a 4-min period of exercise on a cycle ergometer above 60% of VO2max [20].
The rate of pedaling was kept constant at 60 revs/min. The level of exercise was calculated to be similar to that perceived during a general exercise session. Depending on the sex and physical condition of each subject, the workload (W) was set individually aiming at reaching a heart rate above 60% of the predicted HRmax in all subjects. The cycling was stopped when the subjects had reached a heart rate exceeding 60% of the predicted HRmax, perceived the exercise as hard or very hard (values of 14–17 on the RPE scale), and had reached steady-state heart rate; i.e., after approximately 5 min. The exercise on the stationary bicycle took place beside the force platform, so that the test after exercise could be commenced within 10 s.
Statistical analysis
Since no statistically significant difference was found between the right and left legs in the stabilometric variables, the average of the right and left legs; i.e., (right+left)/2, for each stabilometric variable was used for statistical analyses. The use of the mean value of both legs when performing parametric statistics can be questioned, since this may affect the data variability. It cannot, however, be excluded that a dominance of one or the other side exists, which is difficult to define [17], and therefore it is hard to determine which leg to use in comparison with patients. For this reason we used the average of the right and left legs. However, the results were confirmed using the right and left legs separately in the analyses.
Test-retest reliability (group 1)
A number of statistical methods of assessing test-retest reliability were used: 1) mean difference and 95% confidence interval (CI), 2) the two-way random effect model (absolute agreement definition), average measure ICC and 95% CI (ICC2,2 according to Shrout & Fleiss [26]), and 3) the Bland and Altman method of assessing agreement, which includes a scatter plot of the differences between test 1 and test 2 against their mean with 95% limits of agreement (LOA) (i.e., mean difference ± 2 SD of the difference) [27].
Effects of exercise (group 2)
The paired t-test was used for the intra-group comparisons. The median value of the three measurements was used to compare pre- and post-exercise values. In addition, the first and third of the post-exercise measurements were compared, to evaluate the instantaneous value of the ability to maintain postural control in single-limb stance (first measurement) and the possible recovery (third measurement).
A level of P < 0.05 was chosen to indicate statistical significance. Since the present study has an exploratory character, no correction for multiple comparisons was made. The statistical analyses were performed using the program package SPSS 11.0 (SPSS Inc., Chicago, Ill, USA).
Results
Test-retest reliability
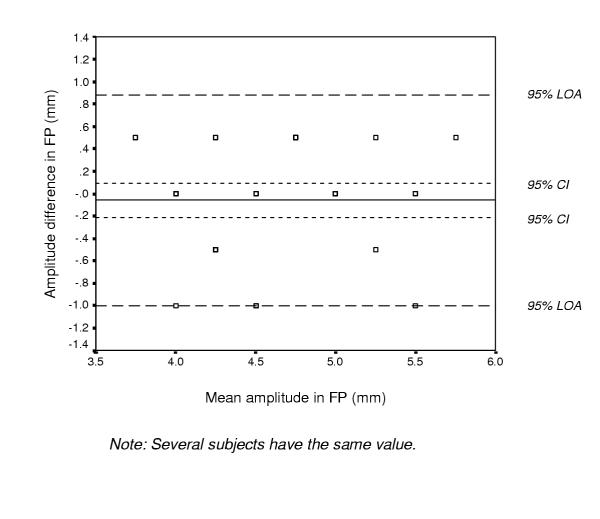
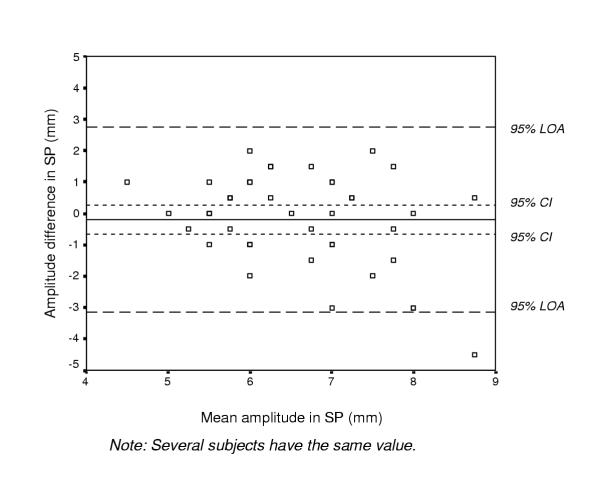
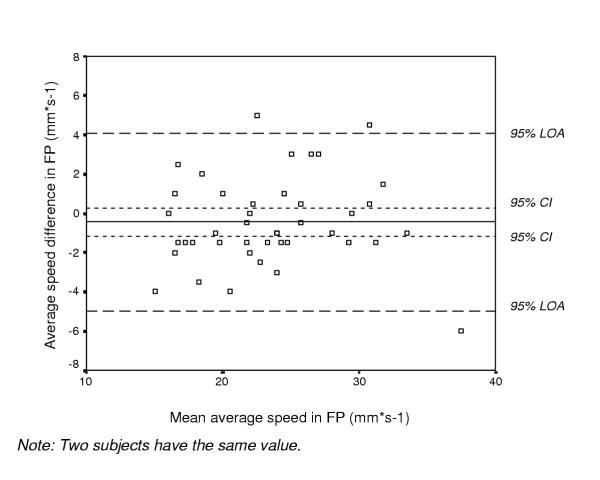
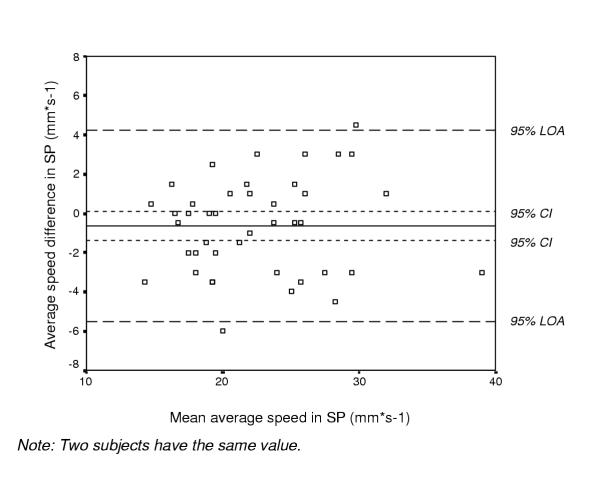
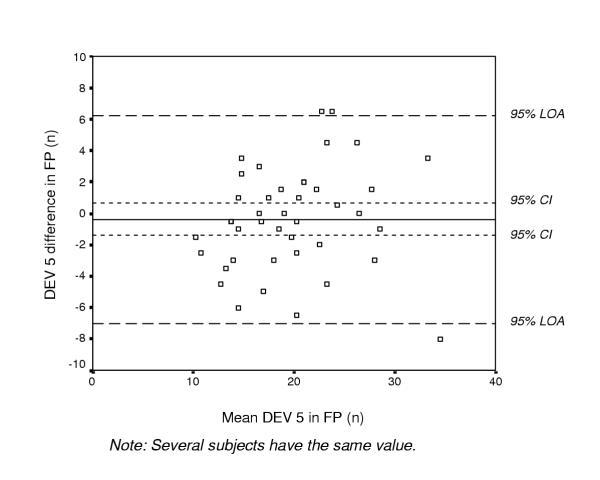
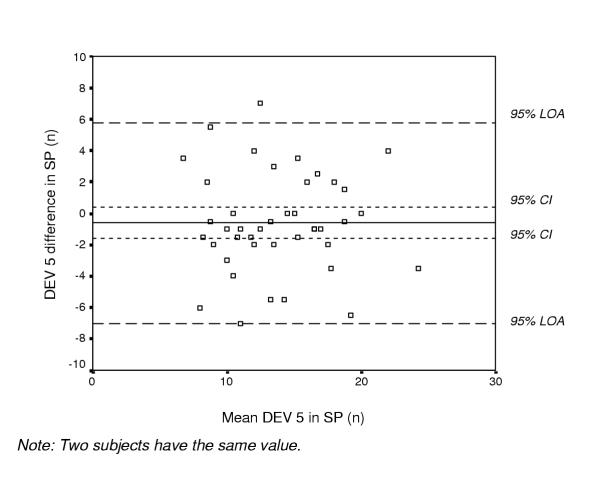
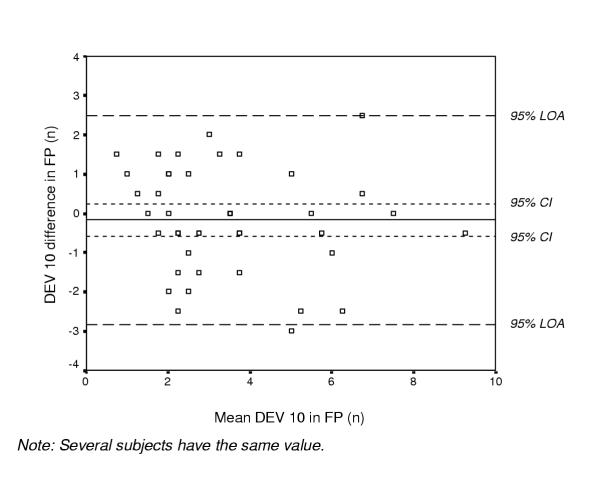
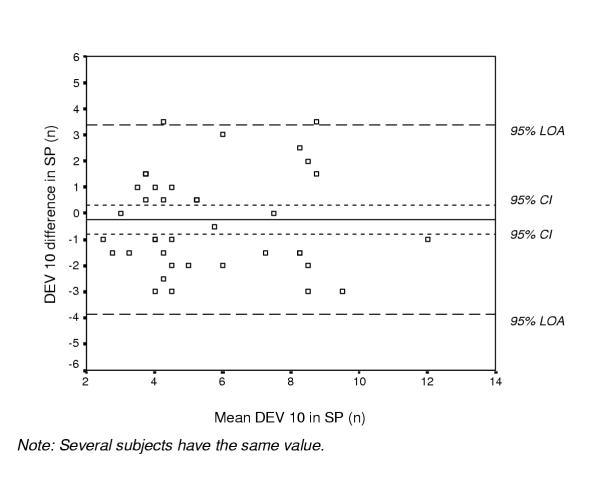
The mean (SD) for test sessions 1 and 2, mean difference with 95% CI, ICC values, and 95% LOA between test 1 and test 2, are given in Table 1. ICC values between 0.79 and 0.95 were found in the stabilometric variables, except for the amplitude in the SP (ICC 0.47). The mean difference and 95% CI revealed no statistically significant difference between test 1 and test 2 (zero is included in each interval). Figures 2, 3, 4, 5, 6, 7, 8 and 9 show the differences between test sessions 1 and 2 (test 2 minus test 1) plotted against their mean for each subject with 95% CI and 95% LOA (see also Table 1). The variables in the FP tended to have smaller mean differences between the test sessions, higher ICC values, and narrower LOAs than the variables in the SP (Table 1).
Table 1.
Test-retest reliability in the stabilometric variables, in 42 healthy subjects.
| Test session 1 Mean (SD) | Test session 2 Mean (SD) | Mean difference (95% CI) | ICC (95% CI) | 95% LOA | |
| Frontal plane | |||||
| Amplitude (mm) | 4.57 (0.55) | 4.51 (0.59) | -0.06 (-0.21 – 0.09) | 0.79 (0.61 – 0.89) | -1.00 – 0.88 |
| Average speed (mm·s-1) | 23.68 (5.38) | 23.23 (5.51) | -0.45 (-1.16 – 0.26) | 0.95 (0.92 – 0.98) | -4.99 – 4.09 |
| DEV 5 (n) | 19.94 (5.71) | 19.57 (6.16) | -0.37 (-1.40 – 0.67) | 0.92 (0.84 – 0.95) | -6.99 – 6.25 |
| DEV 10 (n) | 3.55 (2.14) | 3.38 (1.96) | -0.17 (-0.58 – 0.25) | 0.88 (0.78 – 0.94) | -2.83 – 2.49 |
| Sagittal plane | |||||
| Amplitude (mm) | 6.70 (1.44) | 6.51 (1.02) | -0.19 (-0.65 – 0.27) | 0.47 (0.01 – 0.71) | -3.13 – 2.75 |
| Average speed (mm·s-1) | 22.84 (5.25) | 22.21 (5.47) | -0.63 (-1.39 – 0.13) | 0.94 (0.89 – 0.97) | -5.49 – 4.23 |
| DEV 5 (n) | 14.10 (4.41) | 13.49 (4.40) | -0.61 (-1.60 – 0.39) | 0.85 (0.72 – 0.92) | -7.01 – 5.79 |
| DEV 10 (n) | 5.63 (2.44) | 5.38 (2.39) | -0.25 (-0.81 – 0.31) | 0.84 (0.70 – 0.91) | -3.87 – 3.37 |
Mean (SD) for test sessions 1 and 2, mean difference (95% confidence interval) (test 2 minus test 1), intraclass correlation coefficient (ICC) (95% confidence interval), and 95% limits of agreement (LOA) between test sessions 1 and 2 (test 2 minus test 1) in the stabilometric variables (amplitude in mm, average speed in mm·s-1, and number of movements exceeding 5 mm (DEV 5) and 10 mm (DEV 10)) in the frontal and sagittal planes.
Figure 2.
Bland and Altman graph with limits of agreement (LOA). The differences between test sessions 1 and 2 (test 2 minus test 1) plotted against their mean for each subject for the amplitude in mm in the frontal plane (FP) in 42 healthy subjects, together with the 95% confidence interval (CI) and the 95% LOA.
Figure 3.
Bland and Altman graph with limits of agreement (LOA). The differences between test sessions 1 and 2 (test 2 minus test 1) plotted against their mean for each subject for the amplitude in mm in the sagittal plane (SP) in 42 healthy subjects, together with the 95% confidence interval (CI) and the 95% LOA.
Figure 4.
Bland and Altman graph with limits of agreement (LOA). The differences between test sessions 1 and 2 (test 2 minus test 1) plotted against their mean for each subject for the average speed in mm·s-1 in the frontal plane (FP) in 42 healthy subjects, together with the 95% confidence interval (CI) and the 95% LOA.
Figure 5.
Bland and Altman graph with limits of agreement (LOA). The differences between test sessions 1 and 2 (test 2 minus test 1) plotted against their mean for each subject for the average speed in mm·s-1 in the sagittal plane (SP) in 42 healthy subjects, together with the 95% confidence interval (CI) and the 95% LOA.
Figure 6.
Bland and Altman graph with limits of agreement (LOA). The differences between test sessions 1 and 2 (test 2 minus test 1) plotted against their mean for each subject for the number of movements exceeding 5 mm (DEV 5) in the frontal plane (FP) in 42 healthy subjects, together with the 95% confidence interval (CI) and the 95% LOA.
Figure 7.
Bland and Altman graph with limits of agreement (LOA). The differences between test sessions 1 and 2 (test 2 minus test 1) plotted against their mean for each subject for the number of movements exceeding 5 mm (DEV 5) in the sagittal plane (SP) in 42 healthy subjects, together with the 95% confidence interval (CI) and the 95% LOA.
Figure 8.
Bland and Altman graph with limits of agreement (LOA). The differences between test sessions 1 and 2 (test 2 minus test 1) plotted against their mean for each subject for the number of movements exceeding 10 mm (DEV 10) in the frontal plane (FP) in 42 healthy subjects, together with the 95% confidence interval (CI) and the 95% LOA.
Figure 9.
Bland and Altman graph with limits of agreement (LOA). The differences between test sessions 1 and 2 (test 2 minus test 1) plotted against their mean for each subject for the number of movements exceeding 10 mm (DEV 10) in the sagittal plane (SP) in 42 healthy subjects, together with the 95% confidence interval (CI) and the 95% LOA.
Effects of exercise
Short-duration sub-maximal cycling
All subjects exceeded the 60% value of the predicted HRmax; the mean value being 81% (SD 7%, range 68 to 99%). The median power output produced by the subjects at the end of cycling was 150 W (range 100 to 200 W), and the mean value of perceived exertion, rated according to the RPE scale, was 15.4 (SD 0.9). The final heart rate attained was 159 beats/min (SD 14 beats/min), and the heart rate after the stabilometric assessment, approximately 3.5 minutes after the exercise, was 117 beats/min (SD 16 beats/min).
Amplitude of CP movements
No difference was found in the amplitude in the frontal plane (FP) between pre- and post-exercise values. In the sagittal plane (SP) the amplitude was higher post- than pre-exercise (P = 0.02). The mean (SD) for pre- and post-exercise values, mean difference with 95% CI (post-exercise minus pre-exercise), and P-values are given in Table 2. Five (21%) subjects had a difference between pre- and post-exercise measurements in the FP outside the LOA, and in the SP, 2 (8%) subjects had a difference between the measurements outside the LOA. Analysis of the first and third of the post-exercise measurements showed no difference in the FP or SP (Table 3).
Table 2.
Effects of exercise in the stabilometric variables, in 24 healthy subjects.
| Pre-exercise Mean (SD) | Post-exercise Mean (SD) | Mean difference (95% CI) | P-value | |
| Frontal plane | ||||
| Amplitude (mm) | 4.71 (0.66) | 4.88 (0.59) | 0.17 (-0.88 – 0.42) | 0.19 |
| Average speed (mm·s-1) | 23.19 (5.19) | 24.42 (5.20) | 1.23 (0.29 – 2.17) | 0.01 |
| DEV 5 (n) | 19.13 (5.87) | 19.90 (5.37) | 0.77 (-0.69 – 2.23) | 0.29 |
| DEV 10 (n) | 3.48 (1.84) | 4.38 (2.35) | 0.90 (0.11 – 1.68) | 0.03 |
| Sagittal plane | ||||
| Amplitude (mm) | 7.08 (1.12) | 7.77 (1.10) | 0.69 (0.13 – 1.24) | 0.02 |
| Average speed (mm·s-1) | 24.02 (5.01) | 25.19 (6.17) | 1.17 (-0.19 – 2.53) | 0.09 |
| DEV 5 (n) | 15.98 (4.53) | 14.96 (4.39) | -1.02 (-2.43 – 0.39) | 0.15 |
| DEV 10 (n) | 6.50 (2.47) | 6.58 (2.53) | 0.08 (-0.52 – 0.68) | 0.78 |
Numbers in bold face represent P-values that are statistically significant. Mean (SD), mean difference (95% confidence interval) (post-exercise minus pre-exercise) and P-value (paired t-test) before (pre-exercise) and after (post-exercise) exercise, in the stabilometric variables (amplitude in mm, average speed in mm·s-1, and number of movements exceeding 5 mm (DEV 5) and 10 mm (DEV 10)) in the frontal and sagittal planes.
Table 3.
Instantaneous ability to maintain balance and possible recovery after exercise, in 24 healthy subjects.
| Measurement 1 Mean (SD) | Measurement 3 Mean (SD) | Mean difference (95% CI) | P-value | |
| Frontal plane | ||||
| Amplitude (mm) | 5.02 (0.77) | 5.15 (0.88) | 0.13 (-0.21 – 0.46) | 0.45 |
| Average speed (mm·s-1) | 24.83 (6.22) | 24.25 (5.54) | -0.58 (-1.60 – 0.44) | 0.25 |
| DEV 5 (n) | 20.94 (5.67) | 19.39 (5.97) | -1.54 (-3.32 – 0.23) | 0.09 |
| DEV 10 (n) | 4.83 (2.55) | 4.46 (2.70) | -0.38 (-1.02 – 0.27) | 0.24 |
| Sagittal plane | ||||
| Amplitude (mm) | 7.81 (1.44) | 7.52 (1.34) | -0.29 (-1.01 – 0.43) | 0.41 |
| Average speed (mm·s-1) | 25.29 (6.35) | 25.02 (6.20) | -0.27 (-1.13 – 0.59) | 0.52 |
| DEV 5 (n) | 14.65 (4.66) | 14.73 (5.45) | 0.08 (-1.37 – 1.53) | 0.90 |
| DEV 10 (n) | 6.77 (2.71) | 6.94 (3.23) | 0.17 (-0.91 – 1.24) | 0.75 |
Mean (SD), mean difference (95% confidence interval) (measurement 3 minus measurement 1) and P-value (paired t-test) for post-exercise measurements 1 and 3, in the stabilometric variables (amplitude in mm, average speed in mm·s-1, and number of movements exceeding 5 mm (DEV 5) and 10 mm (DEV 10)) in the frontal and sagittal planes.
Average speed of CP movements
Higher values were observed post- than pre-exercise in average speed in the FP (P = 0.01), although not in the SP (Table 2). One (4%) subject and 3 (12.5%) subjects had a difference between pre- and post-exercise measurements outside the LOA in the FP and SP, respectively. No difference was observed between the first and third of the post-exercise measurements in the FP or SP (Table 3).
Number of movements exceeding 5 mm from the mean value of CP
No difference was noted between pre- and post-exercise values in DEV 5 in the FP or SP (Table 2). One (4%) subject and 2 (8%) subjects had a difference between pre- and post-exercise measurements outside the LOA in the FP and SP, respectively. No difference was observed between the first and third of the post-exercise measurements in the FP or SP (Table 3).
Number of movements exceeding 10 mm from the mean value of CP
Higher values were found in DEV 10 post- than pre-exercise in the FP (p = 0.03), however, not in the SP (Table 2). One (4%) subject had a difference between pre- and post-exercise measurements in the FP outside the LOA. In the SP, none of the subjects had a difference between the measurements outside the LOA. No difference was observed between the first and third of the post-exercise measurements in the FP or SP (Table 3).
Discussion
We have previously reported high reproducibility in healthy subjects for the platform described [16]. However, in that study only the ICC, which is difficult to interpret clinically, was used to assess test-retest reliability. In addition, a systematic error was observed after previous studies, and the platform has therefore been calibrated. For these reasons, a new, extended test-retest reliability study was conducted.
According to the recommendations of Fleiss [28], ICC values above 0.75 represent excellent reliability, while values between 0.4 and 0.75 represent good reliability. All variables, except the amplitude in the SP, showed ICC values above 0.75, which is in accordance with our previous study [16] and those of others [14,15]. Visual analysis of the Bland and Altman graphs and interpretation of the mean difference and 95% CI between the two test sessions, showed that the values tended to be lower in test session 2, which may be interpreted as a learning process. This tendency was, however, not significant as zero was included in the 95% CI (Table 1 and Figures 2, 3, 4, 5, 6, 7, 8 and 9).
To evaluate changes over time in an individual, the magnitude of the change must exceed the inherent variability of the outcome. The LOA can be used to assess a "real" change in an individual's performance as a result of intervention; i.e., if the difference between two measurements is outside the LOA, there is a true change in performance [13]. Since the LOAs were rather wide, the test of balance in single-limb stance we used cannot detect small changes in an individual's performance. In the second part of the study, few subjects (0 – 5) had a difference between the pre- and post-exercise measurements outside the LOAs, i.e., a "real" change in their individual performance. Most subjects had a difference between the measurements within the LOAs, which does not represent a "real" change in their individual performance. This result confirms that small changes in an individual's performance cannot be detected. Relatively large individual measurement errors for balance in single-limb stance measured on a force platform have also been reported by Birmingham [14]. In that study, SEMs and 95% CIs were used as measures of absolute reliability, and the results showed that large changes could be detected, but not small changes, in an individual's score [14]. The test of balance in single-limb stance we used may be more useful and appropriate when distinguishing between groups of subjects, such as between patients and controls. To evaluate an individual's change in balance performance, a "true" change would be outside the LOAs. The tendency towards smaller mean differences between the two test sessions, higher ICC values, and narrower LOAs for the variables in the FP than in the SP, indicates that the variables in the FP may be more reliable.
The second aim of our study was to study the effect of short-duration, sub-maximal general exercise on balance in single-limb stance in healthy subjects. The results revealed higher values post- than pre-exercise in three of the eight measured variables; i.e., the amplitude in the SP, and the average speed and DEV 10 in the FP, whereas the other five variables were unaffected by exercise. In contrast to these higher values found after cycling, all variables tended to have lower values in test session two in the test-retest reliability part of the study. The results of higher values after exercise are supported by the findings of other studies [6-8]. The findings of these studies and our results seem, however, to contradict those of three studies, showing no effect of fatiguing exercise on balance standing on one leg [9-11]. Adlerton & Moritz [10] used the same force platform as that used in our study. However, their fatiguing protocol was different from ours; a local fatiguing protocol involving requesting the subjects to rise on tiptoe repeatedly, which may explain the divergent results. Rozzi et al. [11] suggested that the platform they used had sensitivity too low to detect the effects of muscular fatigue. In the third study mentioned [9], the extent or level of fatigue was not described, which makes it difficult to compare the results with those of other studies.
To evaluate the possible recovery period, the first and third of the post-exercise measurements were compared. It was assumed that the first measurement could provide us with the instantaneous value of the ability to maintain postural control in single-limb stance. No difference was found between the first and third of the measurements, which indicates that the initial ability to maintain balance was not more affected by exercise than the final measurement.
We used general exercise on an ergometer cycle, in order to resemble physical activity, with the aim of fatiguing the subjects to the same extent as that perceived during a general exercise session. All subjects in our study exceeded 60% of the predicted HRmax value; the values ranging from 68% to 99%. Since a given percentage of VO2max results in a higher percentage of HRmax [25], and since the mean value of the predicted HRmax was 81%, it may be assumed that the subjects had reached a value above 60% of the predicted VO2max; the level above which effects of fatigue have been observed after cycling for a period of four minutes [20]. A short recovery time could be assumed in people with good physical condition, and to avoid recovery, the exercise on the stationary bicycle therefore took place beside the force platform, so that the test after exercise could be commenced within 10 s. Walking or running on a treadmill could not take place beside the force platform, and was therefore impractical. In addition, we plan to study the effect of general exercise in individuals with knee injuries at different times after injury, and since the knee is loaded considerably more while running/walking than cycling, cycling was selected due to ethical reasons. We found that short-term, sub-maximal cycling had an effect on balance in single-limb stance. It is, however, possible that larger effects may be seen after running or walking than after cycling. This has been reported in studies assessing postural control while standing on both feet [4,5], indicating that increased loading on the lower extremities affects standing balance to a greater extent. Different methods of inducing fatigue by loading the lower extremities, as well as the effect of general exercise on balancing on one leg after longer durations of exercise than in the present study, need to be further investigated.
To our knowledge, no data is available as to which variables provide the best measure of postural control in single-limb stance. In a previous study on healthy subjects, we reported differences due to age in average speed in the FP and between men and women in both the FP and SP [17]. Amplitude and DEV 10 have been found to be higher among patients with anterior cruciate ligament (ACL) injury compared to a control group of healthy subjects [18]. In that study, CP movements in the FP only were recorded [18]. In the present study, effects of exercise were observed for two variables in the FP (average speed and DEV 10) and one (amplitude) in the SP. Although the amplitude in the SP was able to detect hypothesized changes after the exercise, we recommend that the amplitude variable not be used in future studies, since DEV 10 and amplitude both measure the amplitude of CP movements, and since the amplitude had poorer reliability in the SP than DEV 10 and was unaffected by exercise in the FP. DEV 5 did not add any information in the present study or in a previous one [18], and can therefore also be excluded in future studies. The results of our previous studies and the present one indicate that measurements in the FP may be more sensitive and revealing than those in the SP. Furthermore, measurements in the FP may be more useful since it is more difficult to maintain the center of mass within the narrow width of the base of support in this plane [29] than in the SP.
The changes in balance in single-limb stance found after exercise in the present study may be explained by several factors. Motor control encompasses the control of posture, balance, and movement. It is dependent on afferent information from muscle spindles, receptors located in joint structures, muscles, tendons, and skin, visual and vestibular information, as well as voluntary and reflexive muscular response [30]. The activity of joint receptors, muscle spindles and Golgi tendon organs may be reduced by fatigue, resulting in proprioceptive deficit in muscle receptors and loss of muscular reflexes responsible for dynamic joint stability [31]. Since this afferent information is also important for the maintenance of postural control [30], the decreased muscle response may lead to a poorer ability to maintain balance. Besides the effects of fatigue on standing balance, some studies have also reported increased knee joint laxity [9,32,33], decreased knee proprioception [11,34], and a delay in muscle response [33] following fatiguing exercise. The increased amplitude of CP movements observed after cycling in the present study may be explained by a decrease in muscle response and a delay in muscle reaction, and this larger sway may also explain the increased average speed. These increased values in stabilometry following exercise indicate compensatory mechanisms intended to maintain balance in single-limb stance, or a decreased ability to maintain balance.
Conclusions
No statistically significant bias between the two test sessions was found. The ICCs ranged from 0.79 to 0.95 in all stabilometric variables except one. The Bland and Altman plots with LOA revealed that small changes in an individual's performance cannot be detected. A relatively large difference in an individual's balance performance would be required to confidently state that the change is real. The stabilometric test may thus be more useful and appropriate for distinguishing between groups of subjects. The increased values of average speed and DEV 10 in the FP, and of the amplitude in the SP following cycling for a short period of time at a sub-maximal level, indicate compensatory mechanisms aimed at maintaining balance in single-limb stance, or a decreased ability to maintain balance, in young healthy subjects. Since the amplitude in the SP had poor reliability, and DEV 5 in both planes and amplitude in the FP were unaffected by exercise, these variables can be excluded in future studies. We recommend that average speed and DEV 10; the variables showing the best reliability and effects of exercise, be used in future studies. Our results indicate that measurements in the FP may be more reliable and sensitive than those in the SP.
Competing interests
None declared.
Authors' contributions
EA participated in the design of the study, participated in collecting the data, performed the statistical analysis, and drafted the manuscript. DR participated in collecting the data. EH participated in the progress and revision of the manuscript. TF participated in the design of the study, and in the progress and revision of the manuscript. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
We would like to thank all the subjects who volunteered for this study, Per-Erik Isberg at the Department of Statistics, Lund University for statistical advice, Karin Bergman and Jennie Ohlsson for testing subjects for test-retest reliability, the Swedish Foundation for Health Care Sciences and Allergy Research, the Swedish Rheumatism Association, "Vårdrådet" at Lund University Hospital, "Centrum för Idrottsforskning", and the Faculty of Medicine, Lund University.
Contributor Information
Eva Ageberg, Email: eva.ageberg@sjukgym.lu.se.
David Roberts, Email: david.roberts@ort.lu.se.
Eva Holmström, Email: eva.holmstrom@sjukgym.lu.se.
Thomas Fridén, Email: thomas.friden@ort.lu.se.
References
- Noakes TD. Physiological models to understand exercise fatigue and the adaptations that predict or enhance athletic performance. Scand J Med Sci Sports. 2000;10:123–145. doi: 10.1034/j.1600-0838.2000.010003123.x. [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A, Woollacott M. Control of posture and balance. In: Butler J, editor. Motor control. Theory and practical applications. Baltimore, Williams & Wilkins; 1995. pp. 120–121. [Google Scholar]
- Fridén T, Zätterström R, Lindstrand A, Moritz U. A stabilometric technique for evaluation of lower limb instabilities. Am J Sports Med. 1989;17:118–122. doi: 10.1177/036354658901700120. [DOI] [PubMed] [Google Scholar]
- Lepers R, Bigard AX, Diard JP, Gouteyron JF, Guezennec CY. Posture control after prolonged exercise. Eur J Appl Physiol. 1997;76:55–61. doi: 10.1007/s004210050212. [DOI] [PubMed] [Google Scholar]
- Nardone A, Tarantola J, Giordano A, Schieppati M. Fatigue effects on body balance. Electroencephalogr Clin Neurophysiol. 1997;105:309–320. doi: 10.1016/S0924-980X(97)00040-4. [DOI] [PubMed] [Google Scholar]
- Johnston RB 3rd, Howard ME, Cawley PW, Losse GM. Effect of lower extremity muscular fatigue on motor control performance. Med Sci Sports Exerc. 1998;30:1703–1707. doi: 10.1097/00005768-199812000-00008. [DOI] [PubMed] [Google Scholar]
- Lundin TM, Feuerbach JW, Grabiner MD. Effect of plantar flexor and dorsiflexor fatigue on unilateral postural control. J of Appl Biomechanics. 1993;9:191–201. [Google Scholar]
- Yaggie JA, McGregor SJ. Effects of isokinetic ankle fatigue on the maintenance of balance and postural limits. Arch Phys Med Rehabil. 2002;83:224–228. doi: 10.1053/apmr.2002.28032. [DOI] [PubMed] [Google Scholar]
- Rowe A, Wright S, Nyland J, Caborn DN, Kling R. Effects of a 2-hour cheerleading practice on dynamic postural stability, knee laxity, and hamstring extensibility. J Orthop Sports Phys Ther. 1999;29:455–462. doi: 10.2519/jospt.1999.29.8.455. [DOI] [PubMed] [Google Scholar]
- Adlerton AK, Moritz U. Does calf-muscle fatigue affect standing balance? Scand J Med Sci Sports. 1996;6:211–215. doi: 10.1111/j.1600-0838.1996.tb00093.x. [DOI] [PubMed] [Google Scholar]
- Rozzi S, Lephart S, Fu F. Effects of muscular fatigue on knee joint laxity and neuromuscular characteristics of male and female athletes. J Athl Train. 1999;34:106–114. [PMC free article] [PubMed] [Google Scholar]
- Fridén T, Erlandsson T, Zätterström R, Lindstrand A, Moritz U. Compression or distraction of the anterior cruciate injured knee. Variations in injury pattern in contact sports and downhill skiing. Knee Surg Sports Traumatol Arthrosc. 1995;3:144–147. doi: 10.1007/BF01565473. [DOI] [PubMed] [Google Scholar]
- Atkinson G, Nevill AM. Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Med. 1998;26:217–238. doi: 10.2165/00007256-199826040-00002. [DOI] [PubMed] [Google Scholar]
- Birmingham TB. Test-retest reliability of lower extremity functional instability measures. Clin J Sport Med. 2000;10:264–268. doi: 10.1097/00042752-200010000-00007. [DOI] [PubMed] [Google Scholar]
- Hoffman MA, Koceja DM. Dynamic balance testing with electrically evoked perturbation: a test of reliability. Arch Phys Med Rehabil. 1997;78:290–293. doi: 10.1016/s0003-9993(97)90036-8. [DOI] [PubMed] [Google Scholar]
- Ageberg E, Zätterström R, Moritz U. Stabilometry and one-leg hop test have high test-retest reliability. Scand J Med Sci Sports. 1998;8:198–202. doi: 10.1111/j.1600-0838.1998.tb00192.x. [DOI] [PubMed] [Google Scholar]
- Ageberg E, Zätterström R, Fridén T, Moritz U. Individual factors affecting stabilometry and one-leg hop test in 75 healthy subjects, aged 15–44 years. Scand J Med Sci Sports. 2001;11:47–53. doi: 10.1034/j.1600-0838.2001.011001047.x. [DOI] [PubMed] [Google Scholar]
- Ageberg E, Zätterström R, Moritz U, Fridén T. Influence of supervised and nonsupervised training on postural control after an acute anterior cruciate ligament rupture: A 3-year longitudinal prospective study. J Orthop Sports Phys Ther. 2001;31:632–644. doi: 10.2519/jospt.2001.31.11.632. [DOI] [PubMed] [Google Scholar]
- Zätterström R, Fridén T, Lindstrand A, Moritz U. The effect of physiotherapy on standing balance in chronic anterior cruciate ligament insufficiency. Am J Sports Med. 1994;22:531–536. doi: 10.1177/036354659402200416. [DOI] [PubMed] [Google Scholar]
- Knuttgen HG, Saltin B. Muscle metabolites and oxygen uptake in short-term submaximal exercise in man. J Appl Physiol. 1972;32:690–694. doi: 10.1152/jappl.1972.32.5.690. [DOI] [PubMed] [Google Scholar]
- Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop. 1985;198:43–49. [PubMed] [Google Scholar]
- Winter D. ABC (Anatomy, Biomechanics and Control) of balance during standing and walking. Waterloo, Waterloo Biomechanics; 1995. Balance and posture during quite standing; pp. 5–21.http://www.health.uottawa.ca/biomech/watbiom/book2.htm [Google Scholar]
- Tropp H, Odenrick P. Postural control in single-limb stance. J Orthop Res. 1988;6:833–839. doi: 10.1002/jor.1100060607. [DOI] [PubMed] [Google Scholar]
- Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health. 1990;16:55–58. doi: 10.5271/sjweh.1815. [DOI] [PubMed] [Google Scholar]
- Wilmore J, Costill D. Physiology of sport and exercise. Champaign, Ill., Human Kinetics; 1999. Prescription of exercise for health and fitness; pp. 620–624. [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- Fleiss J. Reliability of measurements. In: Fleiss J, editor. The design and analysis of clinical experiments. New York, John Wiley & Sons; 1986. pp. 2–31. [Google Scholar]
- MacKinnon CD, Winter DA. Control of whole body balance in the frontal plane during human walking. J Biomech. 1993;26:633–644. doi: 10.1016/0021-9290(93)90027-c. [DOI] [PubMed] [Google Scholar]
- Johansson H, Sjölander P, Sojka P. Receptors in the knee joint ligaments and their role in the biomechanics of the joint. Crit Rev Biomed Eng. 1991;18:341–368. [PubMed] [Google Scholar]
- Lattanzio PJ, Petrella RJ. Knee proprioception: a review of mechanisms, measurements, and implications of muscular fatigue. Orthopedics. 1998;21:463–470. doi: 10.3928/0147-7447-19980401-19. [DOI] [PubMed] [Google Scholar]
- Skinner HB, Wyatt MP, Stone ML, Hodgdon JA, Barrack RL. Exercise-related knee joint laxity. Am J Sports Med. 1986;14:30–34. doi: 10.1177/036354658601400106. [DOI] [PubMed] [Google Scholar]
- Wojtys EM, Wylie BB, Huston LJ. The effects of muscle fatigue on neuromuscular function and anterior tibial translation in healthy knees. Am J Sports Med. 1996;24:615–621. doi: 10.1177/036354659602400509. [DOI] [PubMed] [Google Scholar]
- Skinner HB, Wyatt MP, Hodgdon JA, Conard DW, Barrack RL. Effect of fatigue on joint position sense of the knee. J Orthop Res. 1986;4:112–118. doi: 10.1002/jor.1100040115. [DOI] [PubMed] [Google Scholar]