Abstract
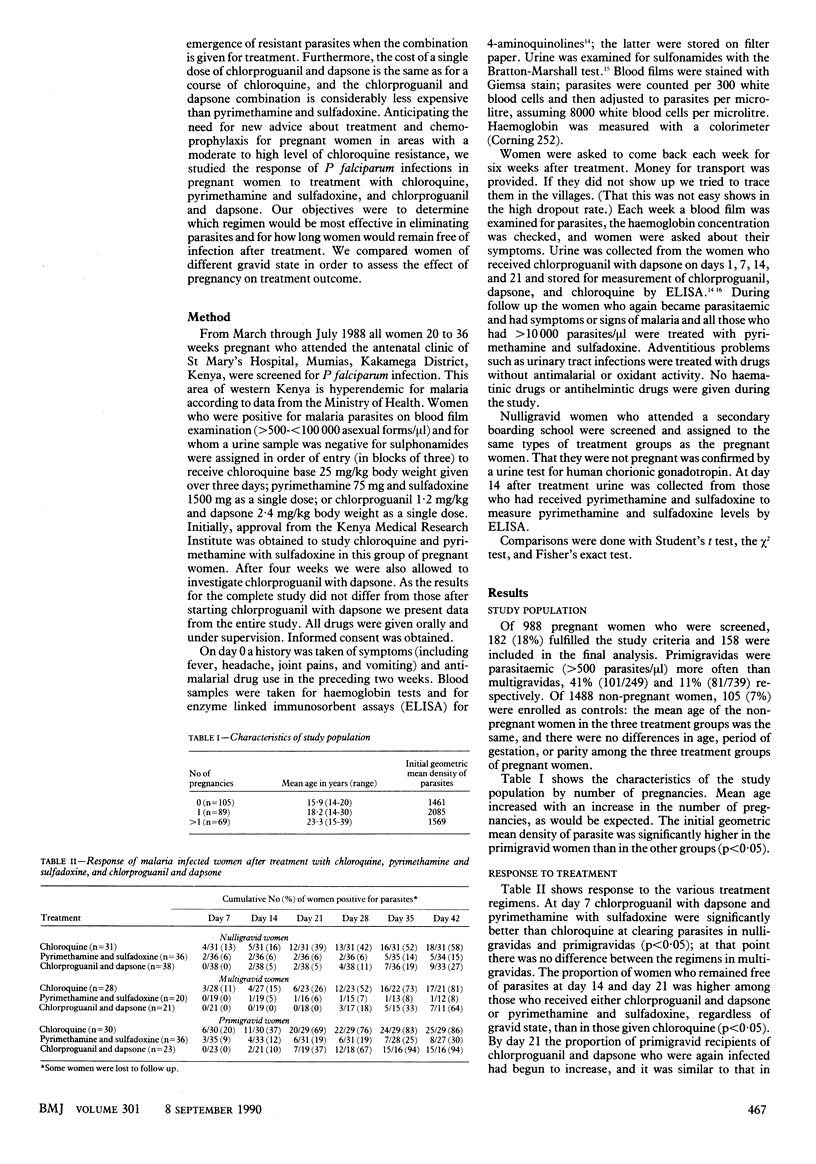
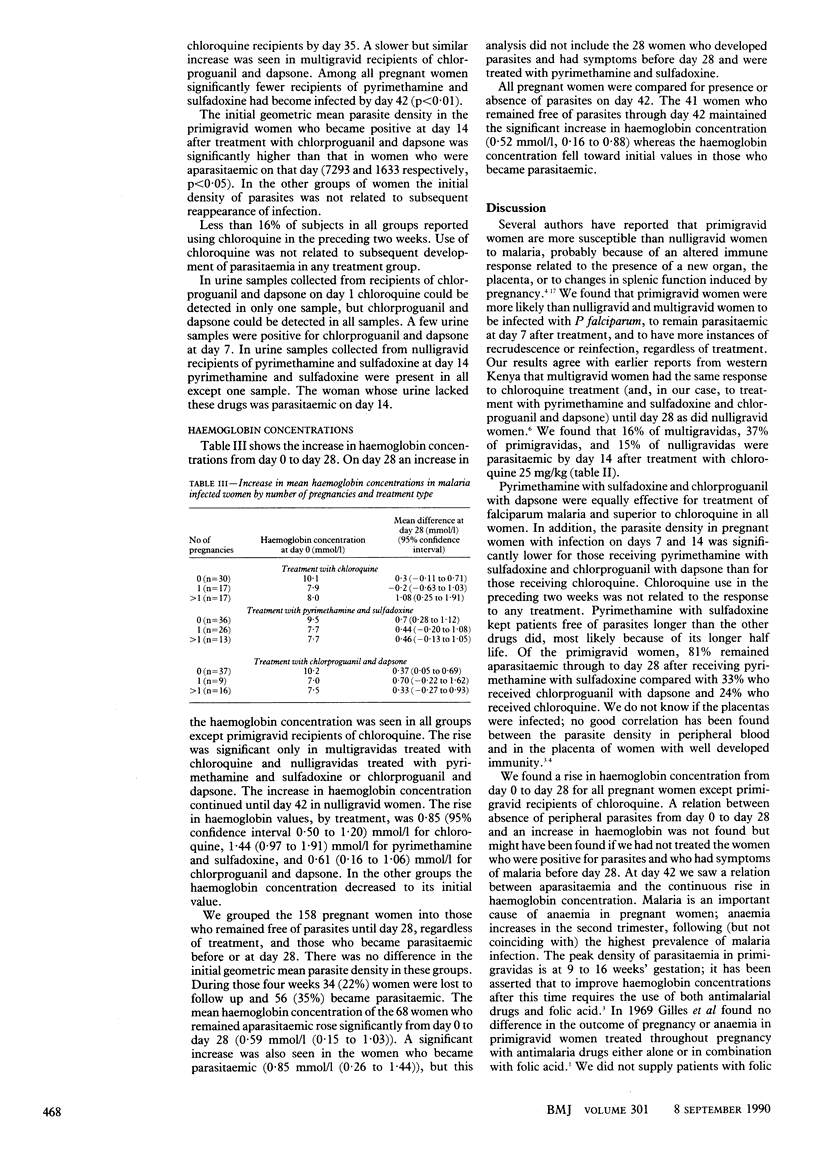
OBJECTIVE--To compare treatment and protection against falciparum malaria in pregnant and non-pregnant women with three drug regimens. DESIGN--Prospective intervention study with six weeks' follow up. Patients received one of three drug regimens in order of entry. SETTING--Primary care hospital and secondary girls' school in rural western Kenya. PATIENTS--158 of 988 pregnant women (89 primigravid and 69 multigravid) in the third trimester and 105 of 1488 non-pregnant schoolgirls of reproductive age were parasitaemic (more than 500 asexual forms/microliter. These women were divided into three treatment groups by gravid state. INTERVENTIONS--Women were treated with chloroquine base 25 mg/kg over three days or pyrimethamine 75 mg and sulfadoxine 1500 mg as a single dose or chlorproguanil 1.2 mg/kg and dapsone 2.4 mg/kg as a single dose. MAIN OUTCOME MEASURES--Parasitaemia and haemoglobin concentrations measured at seven day intervals for six weeks. RESULTS--Primigravid women were more likely to be parasitaemic on follow up than multigravidas or nulligravidas, whose response was about the same. Parasites did not clear by day 7 in primigravidas in six (20%) of 30 who received chloroquine, three (8%) of 35 treated with pyrimethamine and sulfadoxine, and none of 23 treated with chlorproguanil and dapsone. At day 28, 83%, 19%, and 67% of primigravidas in these treatment groups were parasitaemic. Haemoglobin concentrations rose in all women, but improvement was sustained only in women who remained free of parasites. CONCLUSIONS--Clearance of parasites was better with either pyrimethamine and sulfadoxine or chlorproguanil and dapsone than with chloroquine. Longest protection was obtained with pyrimethamine and sulfadoxine.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Black R. H. Malaria in the Australian army in South Vietnam: successful use of a proguanil-dapsone combination for chemoprophylaxis of chloroquine-resistant falciparum malaria. Med J Aust. 1973 Jun 30;1(26):1265–1270. doi: 10.5694/j.1326-5377.1973.tb111114.x. [DOI] [PubMed] [Google Scholar]
- Brabin B. J. An analysis of malaria in pregnancy in Africa. Bull World Health Organ. 1983;61(6):1005–1016. [PMC free article] [PubMed] [Google Scholar]
- Bray R. S., Anderson M. J. Falciparum malaria and pregnancy. Trans R Soc Trop Med Hyg. 1979;73(4):427–431. doi: 10.1016/0035-9203(79)90170-6. [DOI] [PubMed] [Google Scholar]
- Bruce-Chwatt L. J. Malaria and pregnancy. Br Med J (Clin Res Ed) 1983 May 7;286(6376):1457–1458. doi: 10.1136/bmj.286.6376.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Böhni E., Fust B., Rieder J., Schaerer K., Havas L. Comparative toxicological, chemotherapeutic and pharmacokinetic studies with sulphormethoxine and other sulphonamides in animals and man. Chemotherapy. 1969;14(4):195–226. doi: 10.1159/000220630. [DOI] [PubMed] [Google Scholar]
- DeGowin R. L. A review of therapeutic and hemolytic effects of dapsone. Arch Intern Med. 1967 Aug;120(2):242–248. [PubMed] [Google Scholar]
- Gilles H. M., Lawson J. B., Sibelas M., Voller A., Allan N. Malaria, anaemia and pregnancy. Ann Trop Med Parasitol. 1969 Jun;63(2):245–263. doi: 10.1080/00034983.1969.11686625. [DOI] [PubMed] [Google Scholar]
- Graham W. R., Jr Adverse effects of dapsone. Int J Dermatol. 1975 Sep;14(7):494–500. doi: 10.1111/j.1365-4362.1975.tb04283.x. [DOI] [PubMed] [Google Scholar]
- Grayson M. L., Yung A. P., Doherty R. R. Severe dapsone syndrome due to weekly maloprim. Lancet. 1988 Mar 5;1(8584):531–531. doi: 10.1016/s0140-6736(88)91321-9. [DOI] [PubMed] [Google Scholar]
- Hatton C. S., Peto T. E., Bunch C., Pasvol G., Russell S. J., Singer C. R., Edwards G., Winstanley P. Frequency of severe neutropenia associated with amodiaquine prophylaxis against malaria. Lancet. 1986 Feb 22;1(8478):411–414. doi: 10.1016/s0140-6736(86)92371-8. [DOI] [PubMed] [Google Scholar]
- Hengst P. Untersuchungen zur Teratogenität des Daraprim (Pyrimethamin) beim Menschen. Zentralbl Gynakol. 1972 Apr 29;94(17):551–555. [PubMed] [Google Scholar]
- Hernborg A. Stevens-Johnson syndrome after mass prophylaxis with sulfadoxine for cholera in Mozambique. Lancet. 1985 Nov 9;2(8463):1072–1073. doi: 10.1016/s0140-6736(85)90945-6. [DOI] [PubMed] [Google Scholar]
- Maurus J. N. Hansen's disease in pregnancy. Obstet Gynecol. 1978 Jul;52(1):22–25. [PubMed] [Google Scholar]
- McGregor I. A. Epidemiology, malaria and pregnancy. Am J Trop Med Hyg. 1984 Jul;33(4):517–525. doi: 10.4269/ajtmh.1984.33.517. [DOI] [PubMed] [Google Scholar]
- Milhous W. K., Weatherly N. F., Bowdre J. H., Desjardins R. E. In vitro activities of and mechanisms of resistance to antifol antimalarial drugs. Antimicrob Agents Chemother. 1985 Apr;27(4):525–530. doi: 10.1128/aac.27.4.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen-Dinh P., Spencer H. C., Chemangey-Masaba S., Churchill F. C. Susceptibility of Plasmodium falciparum to pyrimethamine and sulfadoxine/pyrimethamine in Kisumu, Kenya. Lancet. 1982 Apr 10;1(8276):823–825. doi: 10.1016/s0140-6736(82)91873-6. [DOI] [PubMed] [Google Scholar]
- Pinichpongse S., Doberstyn E. B., Cullen J. R., Yisunsri L., Thongsombun Y., Thimasarn K. An evaluation of five regimens for the outpatient therapy of falciparum malaria in Thailand 1980-81. Bull World Health Organ. 1982;60(6):907–912. [PMC free article] [PubMed] [Google Scholar]
- Pyrimethamine combinations in pregnancy. Lancet. 1983 Oct 29;2(8357):1005–1007. [PubMed] [Google Scholar]
- Shenton F. C., Bots M., Menon A., Eggelte T. A., de Wit M., Greenwood B. M. An ELISA test for detecting chloroquine in urine. Trans R Soc Trop Med Hyg. 1988;82(2):216–220. doi: 10.1016/0035-9203(88)90415-4. [DOI] [PubMed] [Google Scholar]
- Smith W. C. Are hypersensitivity reactions to dapsone becoming more frequent? Lepr Rev. 1988 Mar;59(1):53–58. doi: 10.5935/0305-7518.19880009. [DOI] [PubMed] [Google Scholar]
- Smithurst B. A., Robertson I., Naughton M. A. Dapsone-induced agranulocytosis complicated by gram-negative septicaemia. Med J Aust. 1971 Mar 6;1(10):537–539. doi: 10.5694/j.1326-5377.1971.tb87694.x. [DOI] [PubMed] [Google Scholar]
- Spencer H. C., Watkins W. M., Sixsmith D. G., Koech D. K., Chulay J. D. A new in vitro test for pyrimethamine/sulfadoxine susceptibility of Plasmodium falciparum and its correlation with in vivo resistance in Kenya. Bull World Health Organ. 1984;62(4):615–621. [PMC free article] [PubMed] [Google Scholar]
- Spencer H. C., Watkins W. W., Sixsmith D. G., Koech D. K. Response of Plasmodium falciparum to dihydrofolate reductase inhibitors in Malindi, Kenya. Trans R Soc Trop Med Hyg. 1986;80(2):201–203. doi: 10.1016/0035-9203(86)90009-x. [DOI] [PubMed] [Google Scholar]
- Steketee R. W., Brandling-Bennett A. D., Kaseje D. C., Schwartz I. K., Churchill F. C. In vivo response of Plasmodium falciparum to chloroquine in pregnant and non-pregnant women in Siaya District, Kenya. Bull World Health Organ. 1987;65(6):885–890. [PMC free article] [PubMed] [Google Scholar]
- Watkins W. M., Brandling-Bennett A. D., Nevill C. G., Carter J. Y., Boriga D. A., Howells R. E., Koech D. K. Chlorproguanil/dapsone for the treatment of non-severe Plasmodium falciparum malaria in Kenya: a pilot study. Trans R Soc Trop Med Hyg. 1988;82(3):398–403. doi: 10.1016/0035-9203(88)90133-2. [DOI] [PubMed] [Google Scholar]
- Watkins W. M., Brandling-Bennett A. D., Oloo A. J., Howells R. E., Gilles H. M., Koech D. K. Inadequacy of chlorproguanil 20 mg per week as chemoprophylaxis for falciparum malaria in Kenya. Lancet. 1987 Jan 17;1(8525):125–128. doi: 10.1016/s0140-6736(87)91966-0. [DOI] [PubMed] [Google Scholar]
- Weetman R. M., Boxer L. A., Brown M. P., Mantich N. M., Baehner R. L. In vitro inhibition of granulopoiesis by 4-amino-4'-hydroxylaminodiphenyl sulfone. Br J Haematol. 1980 Jul;45(3):361–370. doi: 10.1111/j.1365-2141.1980.tb07156.x. [DOI] [PubMed] [Google Scholar]



