Abstract
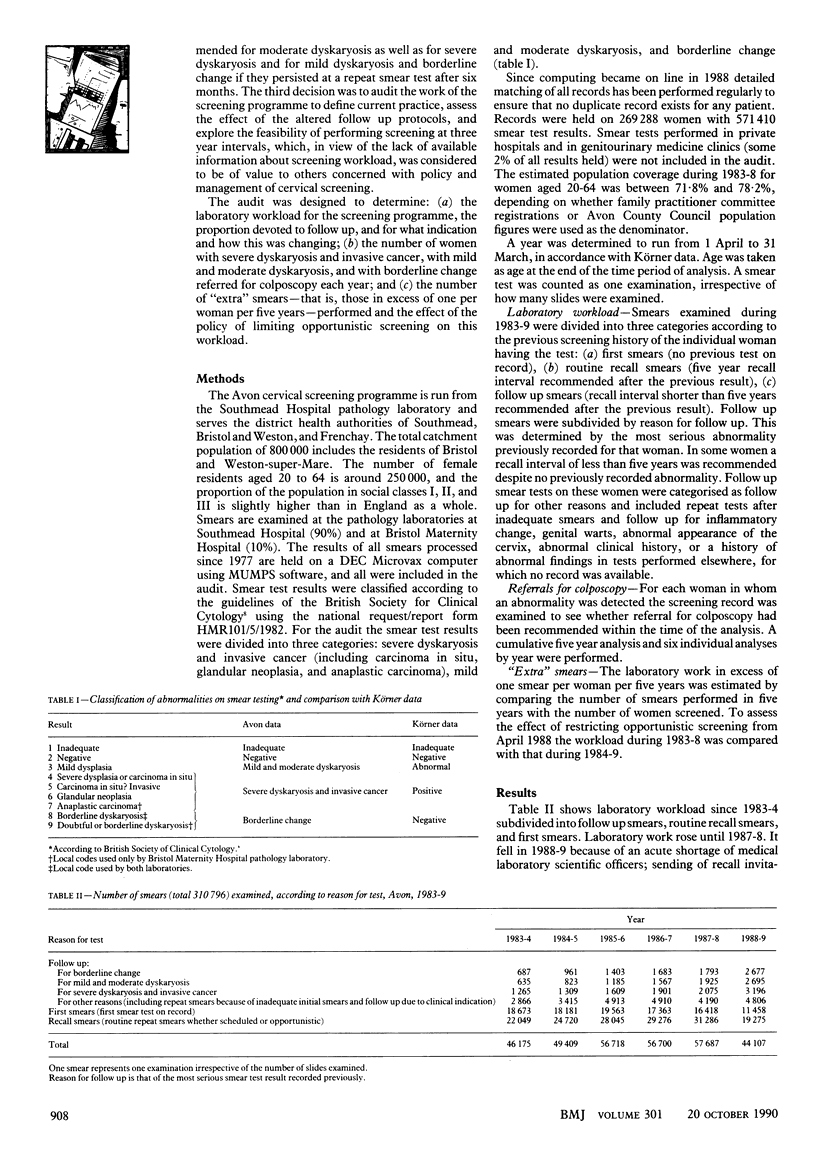
OBJECTIVE--To determine laboratory workload and rates of referral for colposcopy in a three district cervical screening programme during 1983-9 to assess the feasibility of accommodating call up of all women at risk, recall at three year intervals (now five year intervals), and investigation of women with all degrees of abnormality. DESIGN--Analysis of computerised screening histories dating back to 1977 of women screened in the Avon cervical screening programme. SETTING--Three district health authorities covering the population of Bristol and Weston-super-Mare, comprising 800,000 people, of whom 250,000 were female residents aged 20 to 64. SUBJECTS--196,977 Women aged 20 to 64 screened in cervical screening programme since 1983. RESULTS--Laboratory workload devoted to follow up of women with abnormalities increased sharply between 1987-8 and 1988-9, with increases of 54% (from 2075 to 3196) in the number of smears for follow up of severe dyskaryosis and invasive cancer, 40% (from 1925 to 2695) for mild and moderate dyskaryosis, and 49% (from 1793 to 2677) for borderline change. The increases were partly explained by the introduction in April 1988 of protocols for follow up and investigation based on guidance in an intercollegiate working party report. The proportion of women with mild and moderate dyskaryosis who were recommended for referral for colposcopy increased steadily from 9.9% in 1983-4 to 79.9% in 1988-9, and for borderline change the proportions were 3.5% and 13.6% respectively. Of all women tested in 1988-9, referral for colposcopy was recommended in 3%. CONCLUSIONS--The increase in laboratory follow up work identified, if it continued, could result in half of existing laboratory capacity in Avon being devoted to follow up work by 1993, with little prospect of maintaining call, recall, and quality control. Investigation of all women with minor cytological abnormalities is neither justifiable nor sustainable and will undermine the benefits of screening by increasing the rate of false positive results and the financial costs.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson G. H., Boyes D. A., Benedet J. L., Le Riche J. C., Matisic J. P., Suen K. C., Worth A. J., Millner A., Bennett O. M. Organisation and results of the cervical cytology screening programme in British Columbia, 1955-85. Br Med J (Clin Res Ed) 1988 Apr 2;296(6627):975–978. doi: 10.1136/bmj.296.6627.975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans D. M., Hudson E. A., Brown C. L., Boddington M. M., Hughes H. E., Mackenzie E. F., Marshall T. Terminology in gynaecological cytopathology: report of the Working Party of the British Society for Clinical Cytology. J Clin Pathol. 1986 Sep;39(9):933–944. doi: 10.1136/jcp.39.9.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts C. J., Farrow S. C., Charny M. C. How much can the NHS afford to spend to save a life or avoid a severe disability? Lancet. 1985 Jan 12;1(8420):89–91. doi: 10.1016/s0140-6736(85)91975-0. [DOI] [PubMed] [Google Scholar]
- Roberts M. M. Breast screening: time for a rethink? BMJ. 1989 Nov 4;299(6708):1153–1155. doi: 10.1136/bmj.299.6708.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson J. H., Woodend B. E., Crozier E. H., Hutchinson J. Risk of cervical cancer associated with mild dyskaryosis. BMJ. 1988 Jul 2;297(6640):18–21. doi: 10.1136/bmj.297.6640.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witcombe J. B. A licence for breast cancer screening? Br Med J (Clin Res Ed) 1988 Mar 26;296(6626):909–911. doi: 10.1136/bmj.296.6626.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodman C. B., Jordan J. A. Colposcopy services in the West Midlands region. BMJ. 1989 Oct 7;299(6704):899–901. doi: 10.1136/bmj.299.6704.899. [DOI] [PMC free article] [PubMed] [Google Scholar]


