Abstract
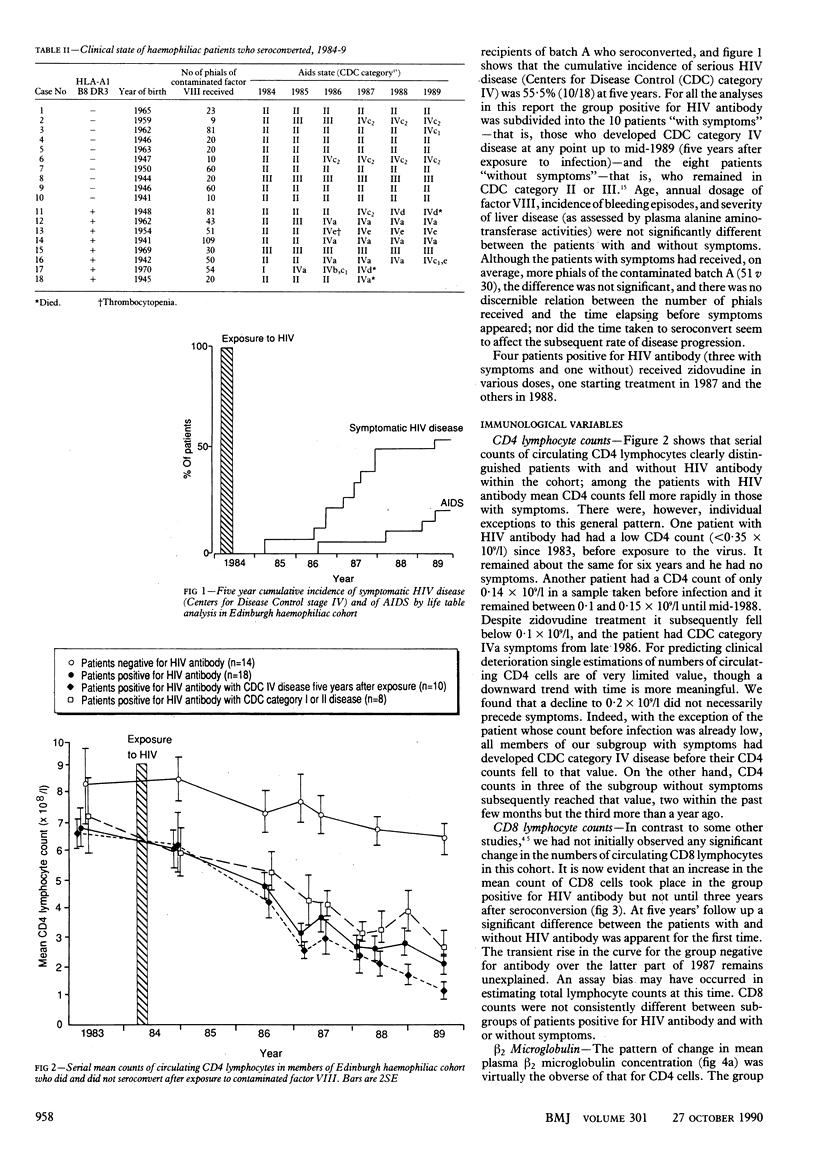
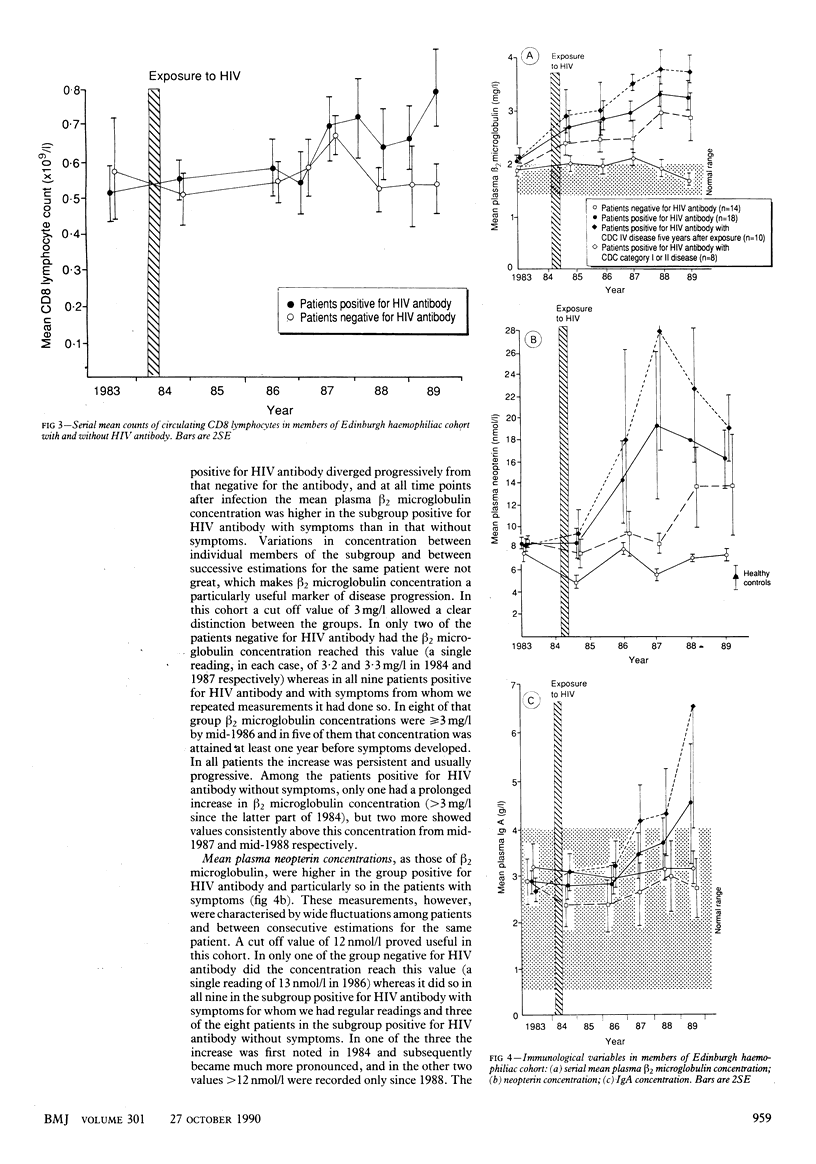
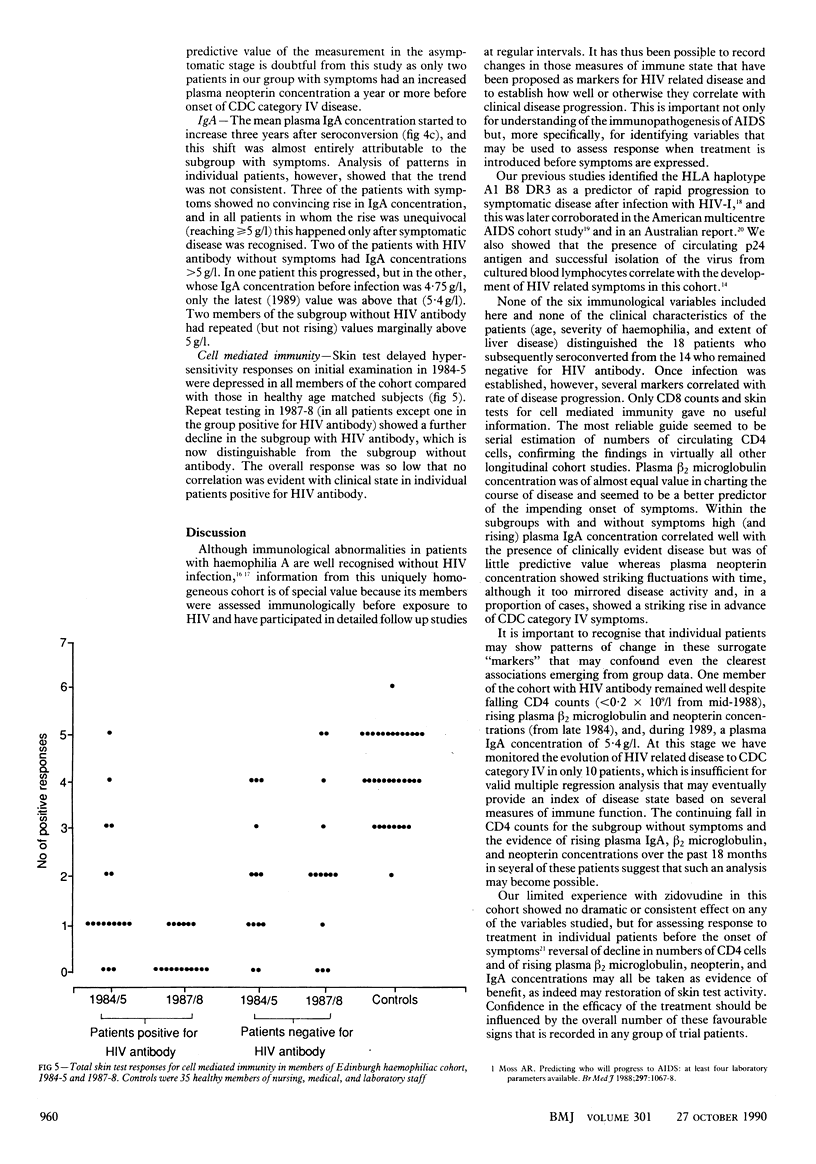
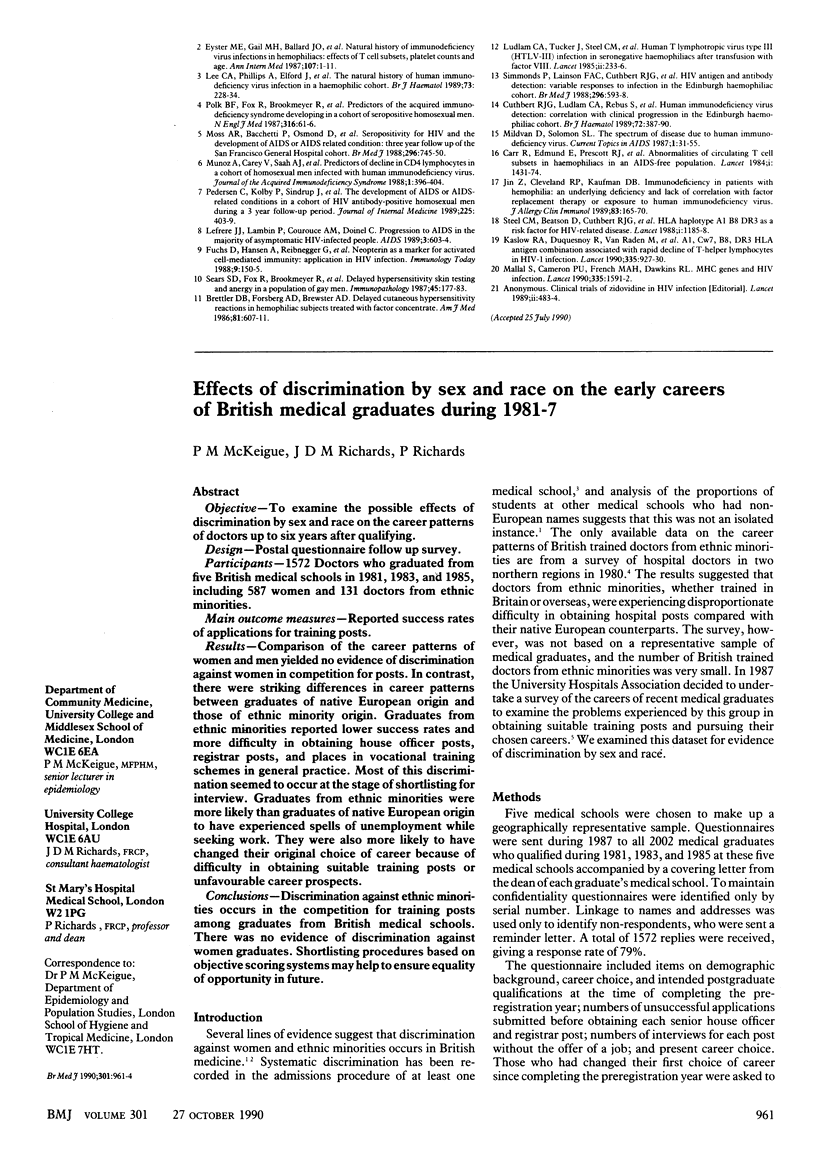
OBJECTIVE--To identify measures of immune state that reflect the course of HIV related disease in order to predict deterioration of symptoms and assess response to treatment. DESIGN--Five year longitudinal clinical and laboratory study. SETTING--Regional haemophilia centre, university virology laboratory, and Medical Research Council laboratory. PATIENTS--32 Patients with haemophilia A exposed to a single batch of HIV contaminated factor VIII concentrate from the Scottish National Blood Transfusion Service in 1984 who were followed up regularly in Edinburgh (31) or abroad (one). MAIN OUTCOME MEASURES--Counts of circulating T cell subsets (CD4 and CD8); plasma beta 2 microglobulin, neopterin, and IgA concentrations; and delayed type hypersensitivity to multiple skin test antigens. RESULTS--18 Patients who seroconverted after exposure had received significantly more contaminated factor VIII than the 14 who did not (mean 43 (range 9-109) v 15 (3-30) phials, p less than 0.01). The two groups were not distinguishable by other criteria before exposure. The group that seroconverted subsequently showed a progressive fall in mean circulating CD4 lymphocytes and an increase in plasma beta 2 microglobulin and neopterin concentrations. From 1987 patients in this group also showed an increase in mean circulating CD8 lymphocytes and in plasma IgA concentration, neither of which was seen in patients who did not seroconvert. Patients with HIV antibody who developed Centers for Disease Control category IV symptoms within five years after infection showed more extreme changes in all measures, except CD8 lymphocyte count, than those whose symptoms remained in categories II and III. Skin test reactivity declined to barely detectable levels in all patients positive for HIV antibody. CONCLUSIONS--Serial estimates of circulating CD4 lymphocytes and of plasma beta 2 microglobulin concentration are the most reliable measures of disease progression; of these, beta 2 microglobulin concentration seems to be the better predictor of impending serious symptoms. High IgA concentrations reflect rather than predict disease state. Individual variation in most measures is such that a wide range of measurements should be used in assessing the effects of trial treatment in HIV infected patients without symptoms.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brettler D. B., Forsberg A. D., Brewster F., Sullivan J. L., Levine P. H. Delayed cutaneous hypersensitivity reactions in hemophiliac subjects treated with factor concentrate. Am J Med. 1986 Oct;81(4):607–611. doi: 10.1016/0002-9343(86)90545-0. [DOI] [PubMed] [Google Scholar]
- Carr R., Veitch S. E., Edmond E., Peutherer J. F., Prescott R. J., Steel C. M., Ludlam C. A. Abnormalities of circulating lymphocyte subsets in haemophiliacs in an AIDS-free population. Lancet. 1984 Jun 30;1(8392):1431–1434. doi: 10.1016/s0140-6736(84)91931-7. [DOI] [PubMed] [Google Scholar]
- Corey L., Whitley R. J., Stone E. F., Mohan K. Difference between herpes simplex virus type 1 and type 2 neonatal encephalitis in neurological outcome. Lancet. 1988 Jan 2;1(8575-6):1–4. doi: 10.1016/s0140-6736(88)90997-x. [DOI] [PubMed] [Google Scholar]
- Cuthbert R. J., Ludlam C. A., Rebus S., Peutherer J. F., Aw D. W., Beatson D., Steel C. M., Reynolds B. Human immunodeficiency virus detection: correlation with clinical progression in the Edinburgh haemophiliac cohort. Br J Haematol. 1989 Jul;72(3):387–390. doi: 10.1111/j.1365-2141.1989.tb07720.x. [DOI] [PubMed] [Google Scholar]
- Eyster M. E., Gail M. H., Ballard J. O., Al-Mondhiry H., Goedert J. J. Natural history of human immunodeficiency virus infections in hemophiliacs: effects of T-cell subsets, platelet counts, and age. Ann Intern Med. 1987 Jul;107(1):1–6. doi: 10.7326/0003-4819-107-1-1. [DOI] [PubMed] [Google Scholar]
- Fuchs D., Hausen A., Reibnegger G., Werner E. R., Dierich M. P., Wachter H. Neopterin as a marker for activated cell-mediated immunity: application in HIV infection. Immunol Today. 1988 May;9(5):150–155. doi: 10.1016/0167-5699(88)91203-0. [DOI] [PubMed] [Google Scholar]
- Jin Z. W., Cleveland R. P., Kaufman D. B. Immunodeficiency in patients with hemophilia: an underlying deficiency and lack of correlation with factor replacement therapy or exposure to human immunodeficiency virus. J Allergy Clin Immunol. 1989 Jan;83(1):165–170. doi: 10.1016/0091-6749(89)90492-2. [DOI] [PubMed] [Google Scholar]
- Kaslow R. A., Duquesnoy R., VanRaden M., Kingsley L., Marrari M., Friedman H., Su S., Saah A. J., Detels R., Phair J. A1, Cw7, B8, DR3 HLA antigen combination associated with rapid decline of T-helper lymphocytes in HIV-1 infection. A report from the Multicenter AIDS Cohort Study. Lancet. 1990 Apr 21;335(8695):927–930. doi: 10.1016/0140-6736(90)90995-h. [DOI] [PubMed] [Google Scholar]
- Lee C. A., Phillips A., Elford J., Miller E. J., Bofill M., Griffiths P. D., Kernoff P. B. The natural history of human immunodeficiency virus infection in a haemophilic cohort. Br J Haematol. 1989 Oct;73(2):228–234. doi: 10.1111/j.1365-2141.1989.tb00257.x. [DOI] [PubMed] [Google Scholar]
- Lefrère J. J., Lambin P., Couroucé A. M., Doinel C. Progression to AIDS in the majority of asymptomatic HIV-infected people. AIDS. 1989 Sep;3(9):603–604. doi: 10.1097/00002030-198909000-00008. [DOI] [PubMed] [Google Scholar]
- Ludlam C. A., Tucker J., Steel C. M., Tedder R. S., Cheingsong-Popov R., Weiss R. A., McClelland D. B., Philp I., Prescott R. J. Human T-lymphotropic virus type III (HTLV-III) infection in seronegative haemophiliacs after transfusion of factor VIII. Lancet. 1985 Aug 3;2(8449):233–236. doi: 10.1016/s0140-6736(85)90288-0. [DOI] [PubMed] [Google Scholar]
- Mallal S., Cameron P. U., French M. A., Dawkins R. L. MHC genes and HIV infection. Lancet. 1990 Jun 30;335(8705):1591–1592. doi: 10.1016/0140-6736(90)91418-a. [DOI] [PubMed] [Google Scholar]
- Moss A. R., Bacchetti P., Osmond D., Krampf W., Chaisson R. E., Stites D., Wilber J., Allain J. P., Carlson J. Seropositivity for HIV and the development of AIDS or AIDS related condition: three year follow up of the San Francisco General Hospital cohort. Br Med J (Clin Res Ed) 1988 Mar 12;296(6624):745–750. doi: 10.1136/bmj.296.6624.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz A., Carey V., Saah A. J., Phair J. P., Kingsley L. A., Fahey J. L., Ginzburg H. M., Polk B. F. Predictors of decline in CD4 lymphocytes in a cohort of homosexual men infected with human immunodeficiency virus. J Acquir Immune Defic Syndr. 1988;1(4):396–404. [PubMed] [Google Scholar]
- Pedersen C., Kolby P., Sindrup J., Gaub J., Ullman S., Gerstoft J., Lindhardt B. O., Dickmeiss E. The development of AIDS or AIDS-related conditions in a cohort of HIV antibody-positive homosexual men during a 3-year follow-up period. J Intern Med. 1989 Jun;225(6):403–409. doi: 10.1111/j.1365-2796.1989.tb00103.x. [DOI] [PubMed] [Google Scholar]
- Polk B. F., Fox R., Brookmeyer R., Kanchanaraksa S., Kaslow R., Visscher B., Rinaldo C., Phair J. Predictors of the acquired immunodeficiency syndrome developing in a cohort of seropositive homosexual men. N Engl J Med. 1987 Jan 8;316(2):61–66. doi: 10.1056/NEJM198701083160201. [DOI] [PubMed] [Google Scholar]
- Sears S. D., Fox R., Brookmeyer R., Leavitt R., Polk B. F. Delayed hypersensitivity skin testing and anergy in a population of gay men. Clin Immunol Immunopathol. 1987 Nov;45(2):177–183. doi: 10.1016/0090-1229(87)90032-8. [DOI] [PubMed] [Google Scholar]
- Simmonds P., Lainson F. A., Cuthbert R., Steel C. M., Peutherer J. F., Ludlam C. A. HIV antigen and antibody detection: variable responses to infection in the Edinburgh haemophiliac cohort. Br Med J (Clin Res Ed) 1988 Feb 27;296(6622):593–598. doi: 10.1136/bmj.296.6622.593. [DOI] [PMC free article] [PubMed] [Google Scholar]


