Abstract
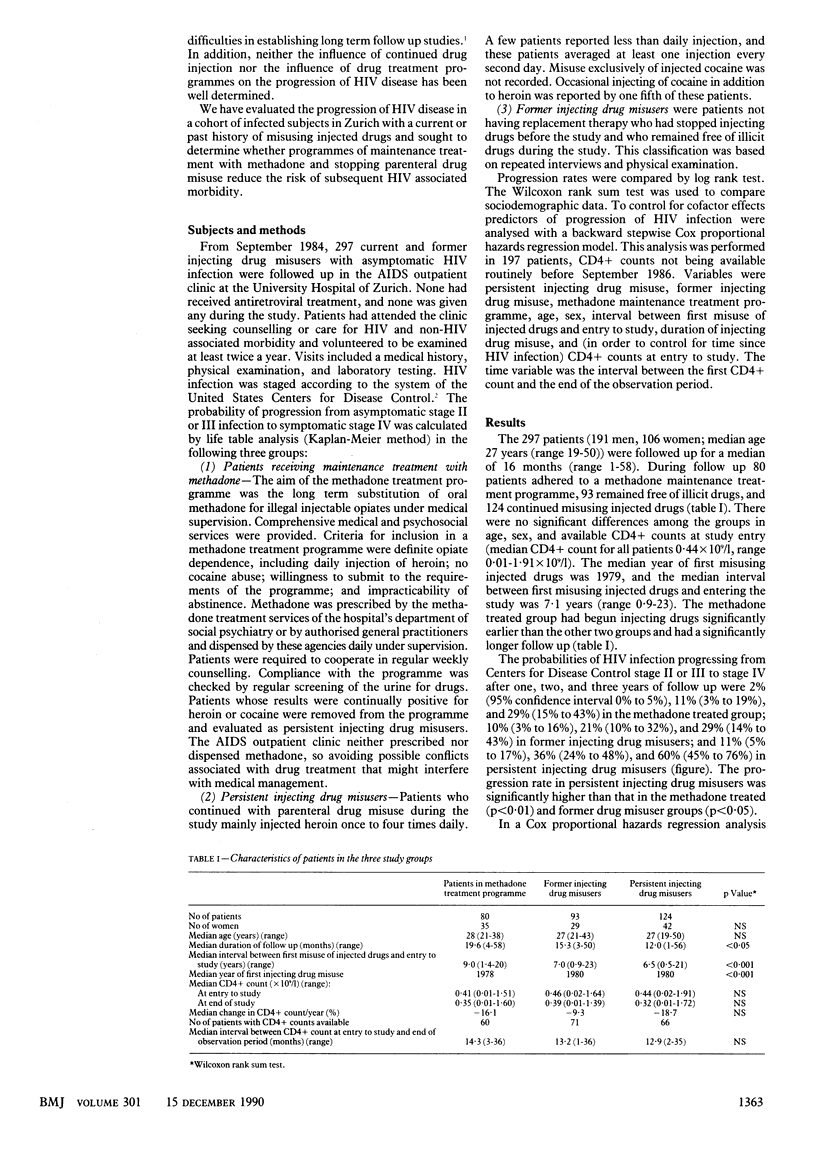
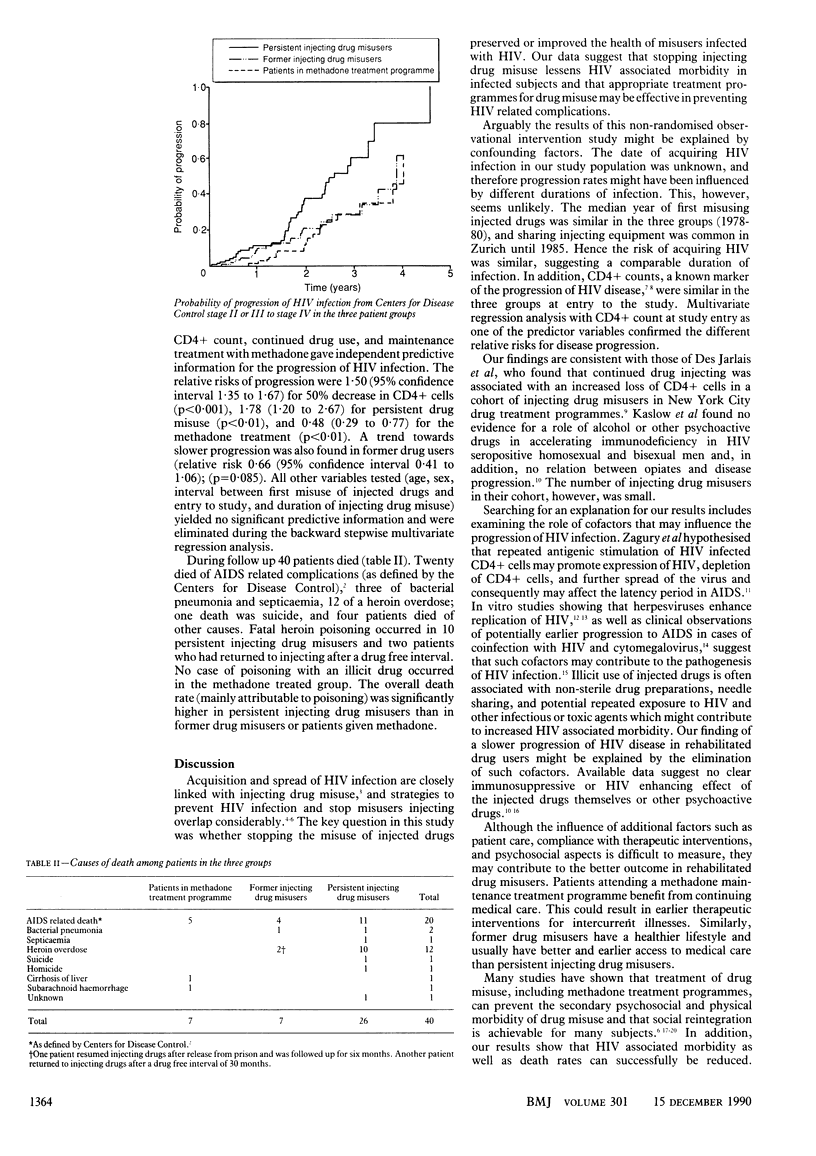
OBJECTIVE--To see whether misusers of injected drugs who stop injecting or switch to a programme of maintenance treatment with methadone have a reduced risk of progression of HIV infection when compared with a group of persistent misusers. DESIGN--Observational cohort study in HIV seropositive subjects with a current or past history of misusing injected drugs. SETTING--HIV outpatient clinic at the University Hospital of Zurich, Switzerland. PATIENTS--297 Current and former parenteral drug misusers (median age 27) with asymptomatic HIV infection. During the observation period 80 subjects adhered to a programme of maintenance treatment with methadone, 124 continued with parenteral drug misuse, and 93 former misusers remained free of illicit drugs. No antiretroviral treatment was given during the study. MAIN OUTCOME MEASURES--Probability of progression of HIV infection from asymptomatic to symptomatic (Centers for Disease Control stage IV) as calculated by life table analysis and compared in the three groups of patients by means of a log rank test, and predictors of disease progression as analysed with a Cox proportional hazards regression model. RESULTS--The 297 patients were followed up for a median of 16 months. The median duration of injecting drug misuse before enrollment was 7.1 years. There were no significant differences among the three groups with respect to CD4+ counts at the beginning of the study (median 0.44 x 10(9)/l). Life table analysis showed a significantly lower probability of progression of HIV disease in both the methadone treated group and former drug misusers than in persistent injecting drug misusers. Multivariate regression analysis showed a relative risk of progression of the disease of 1.78 (95% confidence interval 1.20 to 2.67; p less than 0.01) in persistent injecting drug misusers, 0.48 (0.29 to 0.77; p less than 0.01) in the methadone treated group, and 0.66 (0.41 to 1.06; p = 0.085) in former drug misusers. CONCLUSIONS--Stopping the misuse of injected drugs slows the progression of HIV disease in infected subjects. Drug treatment programmes are effective in secondary prevention of HIV associated morbidity.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bonetti A., Weber R., Vogt M. W., Wunderli W., Siegenthaler W., Lüthy R. Co-infection with human immunodeficiency virus-type 1 (HIV-1) and cytomegalovirus in two intravenous drug users. Ann Intern Med. 1989 Aug 15;111(4):293–296. doi: 10.7326/0003-4819-111-4-293. [DOI] [PubMed] [Google Scholar]
- Brickner P. W., Torres R. A., Barnes M., Newman R. G., Des Jarlais D. C., Whalen D. P., Rogers D. E. Recommendations for control and prevention of human immunodeficiency virus (HIV) infection in intravenous drug users. Ann Intern Med. 1989 May 15;110(10):833–837. doi: 10.7326/0003-4819-110-10-833. [DOI] [PubMed] [Google Scholar]
- Cooper J. R. Methadone treatment and acquired immunodeficiency syndrome. JAMA. 1989 Sep 22;262(12):1664–1668. [PubMed] [Google Scholar]
- Davis M. G., Kenney S. C., Kamine J., Pagano J. S., Huang E. S. Immediate-early gene region of human cytomegalovirus trans-activates the promoter of human immunodeficiency virus. Proc Natl Acad Sci U S A. 1987 Dec;84(23):8642–8646. doi: 10.1073/pnas.84.23.8642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais D. C., Friedman S. R., Marmor M., Cohen H., Mildvan D., Yancovitz S., Mathur U., el-Sadr W., Spira T. J., Garber J. Development of AIDS, HIV seroconversion, and potential co-factors for T4 cell loss in a cohort of intravenous drug users. AIDS. 1987 Jul;1(2):105–111. [PubMed] [Google Scholar]
- Des Jarlais D. C., Friedman S. R., Novick D. M., Sotheran J. L., Thomas P., Yancovitz S. R., Mildvan D., Weber J., Kreek M. J., Maslansky R. HIV-1 infection among intravenous drug users in Manhattan, New York City, from 1977 through 1987. JAMA. 1989 Feb 17;261(7):1008–1012. doi: 10.1001/jama.261.7.1008. [DOI] [PubMed] [Google Scholar]
- Fauci A. S. The human immunodeficiency virus: infectivity and mechanisms of pathogenesis. Science. 1988 Feb 5;239(4840):617–622. doi: 10.1126/science.3277274. [DOI] [PubMed] [Google Scholar]
- Hubbard R. L., Marsden M. E., Cavanaugh E., Rachal J. V., Ginzburg H. M. Role of drug-abuse treatment in limiting the spread of AIDS. Rev Infect Dis. 1988 Mar-Apr;10(2):377–384. doi: 10.1093/clinids/10.2.377. [DOI] [PubMed] [Google Scholar]
- Kaslow R. A., Blackwelder W. C., Ostrow D. G., Yerg D., Palenicek J., Coulson A. H., Valdiserri R. O. No evidence for a role of alcohol or other psychoactive drugs in accelerating immunodeficiency in HIV-1-positive individuals. A report from the Multicenter AIDS Cohort Study. JAMA. 1989 Jun 16;261(23):3424–3429. [PubMed] [Google Scholar]
- Skolnik P. R., Kosloff B. R., Hirsch M. S. Bidirectional interactions between human immunodeficiency virus type 1 and cytomegalovirus. J Infect Dis. 1988 Mar;157(3):508–514. doi: 10.1093/infdis/157.3.508. [DOI] [PubMed] [Google Scholar]
- Zagury D., Bernard J., Leonard R., Cheynier R., Feldman M., Sarin P. S., Gallo R. C. Long-term cultures of HTLV-III--infected T cells: a model of cytopathology of T-cell depletion in AIDS. Science. 1986 Feb 21;231(4740):850–853. doi: 10.1126/science.2418502. [DOI] [PubMed] [Google Scholar]
- de Wolf F., Lange J. M., Houweling J. T., Coutinho R. A., Schellekens P. T., van der Noordaa J., Goudsmit J. Numbers of CD4+ cells and the levels of core antigens of and antibodies to the human immunodeficiency virus as predictors of AIDS among seropositive homosexual men. J Infect Dis. 1988 Sep;158(3):615–622. doi: 10.1093/infdis/158.3.615. [DOI] [PubMed] [Google Scholar]



