Abstract
The environmental contaminant inorganic arsenic (iAs) is a human toxicant and carcinogen. Most mammals metabolize iAs by reducing it to trivalency, followed by oxidative methylation to pentavalency. iAs and its methylated metabolites are primarily excreted in urine within 4–5 days by most species and have a relatively low rate of bioaccumulation. Intra- and interindividual differences in the methylation of iAs may affect the adverse health effects of arsenic. Both inorganic and organic trivalent arsenicals are more potent toxicants than pentavalent forms. Several mechanisms of action have been proposed for arsenic-induced toxicity, but a scientific consensus has not been achieved. Biomarkers of exposure may be used to quantify exposure to iAs. The most common biomarker of exposure for iAs is the measurement of total urinary arsenic. However, consumption of seafood containing high concentrations of organic arsenic can confound estimation of iAs exposure. Because these organic species are thought to be relatively nontoxic, their presence in urine may not represent increased risk. Speciation of urinary arsenic into inorganic and organic forms, and even oxidation state, gives a more definitive indication of the exposure to iAs. Questions still remain, however, as to how reliably the measurement of urinary arsenic, either total or speciated, may predict arsenic concentrations at target tissues as well as how this measurement could be used to assess chronic exposures to iAs.
Keywords: arsenic, biomarker, biomonitoring, exposure, risk assessment
Background
Sources
Arsenic in the environment is from natural and anthropogenic sources. It is commonly bound to carbon, iron, oxygen, and sulfur, forming inorganic and organic arsenicals in various oxidation states. The physico-chemical properties of the many arsenic species are important determinants of their potential toxic effects.
Natural
Arsenic, primarily in its inorganic form, is ubiquitously found in soil, air, and water. More than 200 mineral species contain arsenic. Arsenic binds with iron and sulfur to form arsenopyrite. Background levels of arsenic in soil range from 1 to 40 mg/kg [World Health Organization (WHO) 2001]. Volcanic activity and soil microorganisms release arsenic into the air. Arsenic air levels vary throughout the world, with lower levels in rural areas (0.007–28 ng/m3) and higher levels in urban areas (3–200 ng/m3) (WHO 2001). Water dissolves minerals that may release arsenic. Inorganic arsenic (iAs) levels in seawater and fresh water range from 1 to 10 μg/L (WHO 2001), although levels 1,000 times greater have been recorded (Nordstrom 2002).
Anthropogenic
The major anthropogenic sources of iAs are nonferrous metal smelters and coal-burning energy producers. These processes contaminate air, water, and soil with iAs. Areas near nonferrous metal smelters may have air concentrations of arsenic > 1,000 ng/m3 (WHO 2001). The manufacture and use of arsenical pesticides and the improper handling of tailings from metal mining operations may contaminate surrounding environments.
Uses
Many commercial, medical, veterinary, and pesticide products contain arsenic. Arsenic is used in the manufacture of semiconductors and glass and as a chemotherapeutic agent, pesticide, and growth promoter in farm animals (WHO 2001).
Human Exposure to Arsenic
The diet provides the major amount of arsenic resulting from its nonoccupational human exposure. The estimated daily intake of arsenic in the United States ranges from 2 to 92 μg/day (Tao and Bolger 1998). Levels of iAs are highest in grains (74 ng/g) and produce (9 ng/g) (Schoof et al. 1999). For these foods, iAs constitutes 17–24% of total dietary arsenic. In contrast, organic arsenic (e.g., arsenobetaine) predominates in seafood. Some seafoods have levels of organic arsenic in the parts-per-million range (WHO 2001). Overall, organic arsenic appears to be the major form of dietary arsenic.
Regarding worldwide public health, the most important medium for iAs exposure is drinking water. The source of iAs in drinking water is primarily geologic (Nordstrom 2002). Approximately 98% of the U.S. population ingests drinking water containing < 10 μg As/L (Chappell et al. 1997). Chronic exposure to elevated levels of iAs in drinking water is associated with the development of cancer and other adverse outcomes (Table 1) [National Research Council (NRC) 1999, 2001; WHO 2001]. Millions of people worldwide ingest drinking water contaminated with iAs at levels > 100 μg/L (Chatterjee et al. 1995; Smith et al. 2000).
Table 1.
Range of chronic human oral exposures to iAs resulting in adverse effects.
| System or effect | LOAEL (mg/kg/day) |
|---|---|
| Cardiovascular | 0.002–0.067 |
| Dermal | 0.005–0.08 |
| Endocrine | 0.11 |
| Gastrointestinal | 0.015–0.06 |
| Hematopoietic | 0.05 |
| Hepatic | 0.006–0.1 |
| Neurologic | 0.005–0.11 |
| Respiratory | 0.015–0.08 |
| Cancer | 0.0011–3.67 |
LOAEL, lowest observable adverse effect level. Data adapted from ATSDR (2000).
Occupational and nonoccupational exposure to iAs may occur by inhalation at or near nonferrous smelters, residential and industrial burning of coal, or pesticide manufacturing plants and by dermal contact of arsenic-contaminated soil or use of arsenic-containing pesticides. Estimates of arsenic air concentrations at a Tacoma, Washington, copper smelter exceeded 1,000 μg/m3 during certain periods of its operation (Enterline et al. 1987).
Wood containing the preservative chromated copper arsenate (CCA) is of recent interest. In the United States, CCA-treated wood is found in many residences and playgrounds. Approximately 5 times more water-soluble arsenic was found on the hands of children who played on playgrounds built with CCA-treated wood than of children who played on equipment without CCA-treated wood (Kwon et al. 2004). Due in part to the concern about exposure to children, the use of CCA-treated wood in homes and playgrounds was voluntarily phased out in 2003.
Arsenic and Biomarkers
Biomarkers are classified as those of exposure, effect, and susceptibility. For arsenic, biomarkers of exposure have received the greatest attention. The most common arsenic biomarker of exposure is the analysis of total arsenic in urine. Urinary porphyrins have also been proposed as an arsenic biomarker of exposure (Wang et al. 2002). After chronic ingestion of iAs, dermatologic lesions may develop. These lesions have been used as a long-term biomarker of cumulative arsenic exposure (Chen et al. 2005). Candidate arsenic effect biomarkers include clastogenicity in peripheral lymphocytes (Maki-Paakkanen et al. 1998), micronuclei in oral mucosa and bladder cells (Biggs et al. 1997), and induction of heme oxygenase (Del Razo et al. 2001a). A potential susceptibility biomarker is variability in arsenic metabolism, which reflects polymorphisms in the genes that encode the arsenic-metabolizing enzymes (Vahter 2000).
Disposition of Arsenic
iAs is readily absorbed after oral exposure by most mammalian species. Absorption of iAs after inhalation is relatively less than after oral exposure and is more limited after dermal exposure (NRC 1999; WHO 2001). After oral absorption, iAs is primarily methylated in the liver and excreted in urine by most species. The metabolic pathway (Equation 1) of iAs involves sequential two-electron reduction of AsV species [arsenate, iAsV; monomethylarsonic acid, MMAV; dimethylarsinic acid, DMAV) followed by oxidative methylation of AsIII species (arsenite, iAsIII; monomethylarsonous acid, MMAIII; dimethylarsinous acid, DMAIII) (Thomas et al. 2001):
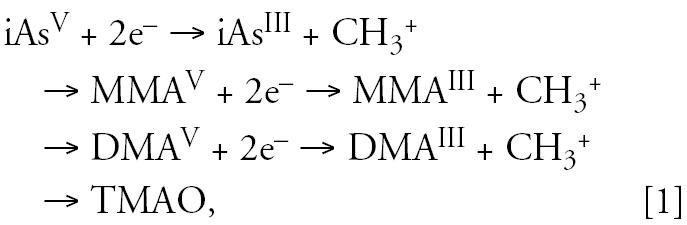 |
where TMAO is trimethylarsine oxide. The AsV species are reduced to AsIII species in vitro nonenzymatically by thiols and enzymatically by purine nucleotide phosphorylase and MMAV reductase (Aposhian et al. 2004; Thomas et al. 2001). The oxidative methylation of AsIII species is an enzymatic process. Arsenic-methylating enzymes from rabbit and rat liver have been characterized. For in vitro activity, these enzymes require a thiol and the methyl donor S-adenosylmethione (Aposhian et al. 2004; Thomas et al. 2001). The rabbit enzyme appears to have two distinct methylating activities, one each for iAsIII and MMAIII. The rat enzyme (AS3MT) has methyltransferase and reductase activities. Mice and humans have orthologues of the rat gene that encodes for AS3MT (Thomas et al. 2004). Regardless of the pathway of arsenic metabolism, exposure to iAs results in the urinary excretion of predominantly DMAV and smaller amounts of inorganic and organic AsV and AsIII species, including TMAO.
Variation in arsenic metabolism
Metabolism of iAs varies between species and human populations (Loffredo et al. 2003; Vahter 2000; Vahter et al. 1995). Dogs and mice are rapid methylators of iAs and excrete ≥ 80% of the dose as DMAV in urine. Humans excrete relatively more MMAV than other species, suggesting that humans are slower methylators of iAs. This may explain in part why humans are more sensitive to iAs than other species. Arsenic excreted by humans tends to be 10–20% MMAV, whereas that of dogs, hamsters, mice, rabbits, and rats is 1–5% MMAV (Vahter 2000). The guinea pig, marmoset monkey, and chimpanzee do not methylate iAs in vivo (Vahter 2000). The toxicologic effects of iAs in these animals are not known.
The distribution of arsenic in human urine is generally 10–30% iAs, 10–20% MMAV, and 60–70% DMAV (Vahter 2000). Some populations excrete varying amounts of MMAV, both considerably less and more, in urine (Vahter 2000; Vahter et al. 1995). This suggests that there are genetic polymorphisms in the regulation of the enzyme(s) that metabolize arsenic, which may lead to differences in toxicity related to arsenic exposure. However, the intraindividual variation of iAs metabolism, measured over a 5-day period by Concha et al. (2002), appears to be stable over time.
Biologically Active Agent
Methylation of iAs to DMAV facilitates excretion of arsenic. Historically, DMAV has been identified as being > 20-fold less acutely toxic than iAs, suggesting that methylation of iAs is a detoxication reaction. Improvements in analytical techniques have resulted in detection of MMAIII and DMAIII in the urine of individuals exposed to iAs (Aposhian et al. 2000; Del Razo et al. 2001b; Mandal et al. 2001). Thus, trivalent organic arsenicals are not the transitory intermediates previously believed, although their stability is an issue. MMAIII and DMAIII are potent in vitro and in vivo toxicants (Petrick et al. 2000, 2001; Styblo et al. 2000). DMAV, albeit at relatively high doses, is a multiorgan tumor promoter in rodents and a complete bladder carcinogen in rats (Wanibuchi et al. 2004). Methylation of iAs may not be a mechanism of detoxication but one of activation.
Arsenic Toxicity
The toxic effects of arsenic are related to its oxidation state (Hughes 2002; WHO 2001); trivalent arsenicals are more potent than pentavalent arsenicals. The mechanism of action for arsenic toxicity is not clearly known. Trivalent arsenicals react directly with sulf-hydryls, a key component of many proteins. Arsenate, pentavalent iAs, has properties similar to those of phosphate (Dixon 1997). Arsenate may replace phosphate in critical biochemical processes that could lead to a toxic effect.
Animal
The LD50 (median lethal dose) of iAs in rodents, depending on its oxidation state and route of administration, ranges from 10 to 90 mg/kg (WHO 2001). Arsenite is 3–4 times more potent than arsenate. MMAIII administered intraperitoneally is more acutely toxic than iAsIII in hamsters (Petrick et al. 2000). MMAV and DMAV are less potent than iAs in rodents, with LD50 values, depending on route of administration, ≥ 470 mg/kg (WHO 2001).
Adverse noncancerous effects of iAs include embryo and fetal toxicity, teratogenicity, genotoxicity (by indirect DNA- or chromosome-damaging mechanisms), and cardiovascular toxicity (WHO 2001).
Human
The oral LD50 of iAs in humans is estimated to be 1–2 mg/kg (Ellenhorn 1997). Chronic exposure to iAs may result in cutaneous, developmental, hematologic, reproductive, and vascular effects (Table 1) [U.S. Agency for Toxic Substances and Disease Registry (ATSDR) 2000; NRC 1999; WHO 2001]. However, the potential for iAs to cause specific birth anomalies such as neural tube defects has been questioned (DeSesso et al. 1998).
The oral reference dose (RfD; a dose considered safe for regular daily consumption without adverse health effects) for iAs is 0.3 μg/kg/day, taking into account estimates of arsenic in food (2 μg As/day) and the volume of water consumed (4.5 L/day) [U.S. Environmental Protection Agency (U.S. EPA) 1993]. This RfD was based primarily on studies of a Taiwanese population, some of whom ingested high levels of iAs (400–600 μg/L) in drinking water (Tseng 1977; Tseng et al. 1968). A no observed adverse effect level of 0.8 μg/kg/day was derived from the critical effects of hyper-pigmentation, keratosis, and potential vascular complications (U.S. EPA 1993).
Arsenic Carcinogenicity
The International Agency for Research on Cancer (1987) and the U.S. EPA (1993) have classified iAs, based on human evidence alone, as a group 1 and group A carcinogen, respectively. However, the mechanism of action for iAs-induced carcinogenicity is not known. Proposed mechanisms include genotoxicity, oxidative stress, inhibition of DNA repair, tumor promotion, cocarcinogenesis, cell proliferation, and altered signal transduction or DNA methylation (Hughes 2002; Kitchin 2001; Rossman 2003). More than one of these mechanisms may occur, and some may work together.
Animal
The results of many cancer bioassays in which several species were administered iAs in the diet or drinking water or after oral intubation have been negative (Hughes 2002; Kitchin 2001; Rossman 2003). The lack of an animal model for iAs-induced carcinogenicity has hindered determination of a mechanism for this effect. However, recent studies with iAs have used transgenic mice (Chen 2000; Germolec et al. 1997), ultraviolet radiation as a co-carcinogen (Burns et al. 2004), and in utero exposure at relatively high doses (Waalkes et al. 2004). In these studies, tumors have developed in the iAs-exposed animals.
Rats administered high levels of DMAV in the diet or drinking water developed bladder tumors (Arnold et al. 1999; Wei et al. 1999). DMAV is also a multiorgan tumor promoter in rodents (Wanibuchi et al. 2004). Hepatocellular adenomas were significantly increased over background levels in rats administered TMAO in drinking water (Shen et al. 2003b). In contrast MMAV administered in the diet (Arnold et al. 2003) or drinking water (Shen et al. 2003a) of rodents was not carcinogenic.
Human
Lung cancer from occupational exposure to arsenic in smelter workers, miners, and pesticide manufacturers has been reported (NRC 1999; WHO 2001). Exposure to drinking water contaminated with iAs can lead to the development of cancer in skin, bladder, lung, kidney, and other internal organs (NRC 1999, 2001; WHO 2001).
Quantitative estimates for the risk of development of skin cancer from oral exposure to iAs are an oral slope factor of 1.5 mg/kg/day and a drinking water unit risk of 5 × 10−5 μg/L (U.S. EPA 1993). The arsenic inhalation unit risk for cancer, based on studies of occupational exposure to iAs, is 4.3 × 10−3 μg/m3 (U.S. EPA 1993).
A National Academy of Sciences committee analyzed the health effects of iAs in drinking water and reported theoretical maximum-likelihood estimates of excess lifetime risk of bladder and lung cancer in the U.S. population (NRC 2001). At 10 μg/L of arsenic in water, the incidence per 105 people for bladder cancer was 12 for females and 23 for males. The incidence per 105 people for lung cancer was 18 for females and 14 for males. These risk estimates are greater than those used by the U.S. EPA in its decision to lower the arsenic drinking water maximum contaminant level (MCL) from 50 to 10 μg As/L.
Methodologies for Detection and Speciation of Arsenic
Many techniques are available to analyze arsenic in biological samples (B’Hymer and Caruso 2004; Francesconi and Kuehnelt 2004; Gong et al. 2002; Mandal et al. 2004; WHO, 2001). Methods to measure total arsenic include neutron activation, X-ray fluorescence, atomic absorption and fluorescence spectrometry, and inductively coupled plasma–atomic emission and –mass spectrometry. The latter two techniques are the most sensitive for total arsenic measurement (picogram range). Sample preparation can be burdensome for total arsenic measurement using the spectroscopic techniques. The organic arsenic in the matrix must be converted to iAs, usually by heating the sample to extreme temperatures in concentrated acid or by dry ashing.
Speciated analysis can differentiate inorganic from organic arsenic, and some techniques may maintain its oxidation state. Speciated analysis is performed by coupling chromatographic separation with a detector used for total arsenic analysis (Table 2). Sample preparation for speciated analysis is not as extreme as required for total arsenic analysis. In some cases, urine can be analyzed directly after removal of particulates by centrifugation.
Table 2.
Examples of analytical techniques for speciation and detection of arsenic in urine.
| Separation | Detection | Arsenic species | Level of detection | Reference |
|---|---|---|---|---|
| Cryogenic | Hydride generation–atomic absorption spectrometry | iAsIII, iAsV, MMAIII, MMAV, DMAIII, DMAV, TMAO | 0.14–0.4 ng | Devesa et al. 2004 |
| HPLC (ion pair) | Hydride generation–atomic fluorescence spectrometry | iAsIII, iAsV, MMAIII, MMAV, DMAIII, DMAV | 10–40 pg | Le et al. 2000 |
| HPLC (ion pair) | Hydride generation–inductively coupled plasma–atomic emission spectrometry | iAsIII, iAsV, MMAV, DMAV | 4–10 ng | Do et al. 2000 |
| HPLC (anion exchange) | Hydride generation–inductively coupled plasma mass spectrometry | iAsIII, iAsV, MMAIII, MMAV, DMAIII, DMAV, arsenocholine, arsenobetaine | 3–7 pg | Mandal et al. 2004 |
| HPLC (anion exchange) | Hydride generation–atomic absorption spectrometry | iAsIII, iAsV, MMAV, DMAV, TMAO | 0.11–0.26 ng | Sur and Dunemann 2004 |
HPLC, high-performance liquid chromatography.
The stability of arsenicals, particularly trivalent species, excreted in urine is a critical issue for speciated arsenic analysis. It is generally difficult to analyze urinary arsenic at a collection site. Storage of samples at 4 and −20°C appears to be suitable for maintaining the valence of some arsenicals for several months (Chen et al. 2002; Feldmann et al. 1999). Freeze-drying urine samples and storing frozen also extends stability of arsenicals (Feldmann et al. 1999; Yoshinaga et al. 2000).
Crecelius and Yager (1997) examined the variability in arsenic quantitation among several different laboratories. These laboratories analyzed standard solutions of MMAV and DMAV, a reference sample and human urine spiked with iAsIII, iAsV, MMAV, and DMAV. Different methods were used for total and speciated arsenic analysis. For samples that contained < 5 μg/L arsenic, the accuracy and precision were poor. However, the measurement of total iAs, MMAV, and DMAV improved at levels > 5 μg/L, levels relevant to human exposure.
Standard reference material for arsenic is available in biological matrices such as urine, muscle, and liver but is certified only for total arsenic. Although a certified reference material for speciated arsenic in urine has been prepared (Yoshinaga et al. 2000), it is less readily obtainable. The identity of specific arsenicals has also become an issue. Hansen et al. (2004) reported that an arsenic sulfur compound that was detected in urine has been misidentified as DMAIII. The availability of standard reference material for arsenic, which includes the trivalent methylated forms, has a tremendous impact on the ability to properly conduct an arsenic exposure analysis if biomarkers of exposure are to be used.
Biomarker Characterization
Arsenic biomarkers of exposure include the analysis of urine, blood, hair, or nails for arsenic. Detection of arsenic in these biological samples is indicative of systemic absorption after exposure to it. However, arsenic from external sources may bind to hair and nails, which can complicate the exposure analysis.
Urine
Absorbed arsenic is primarily excreted in urine, with a half-life of approximately 4 days in humans (NRC 1999; WHO 2001). Urinary arsenic is analyzed as total or speciated. Background levels of urinary arsenic range from 5 to 50 μg/L (NRC 1999). Excessive exposure to iAs in drinking water can lead to urinary arsenic levels > 700 μg/L (Buchet et al. 1999). For occupational exposure to iAs, the recommended biologic exposure determinant value is 35 μg As/L in urine (American Conference of Governmental Industrial Hygienists 2004). This level is a guideline for potential workplace health hazards and includes excreted iAs plus its methylated metabolites.
Quantitative correlations between the concentration of arsenic in urine and in air, water, or soil have been observed (Table 3). Linear relationships have been determined between urinary arsenic and iAs in water and soil. For iAs in soil, the correlations to urinary arsenic are less consistent; very high levels of iAs are generally necessary for a positive correlation to urinary arsenic (Valberg et al. 1997). This relationship is influenced by arsenic geochemistry and bioavailability of the arsenic in the soil matrix. For iAs in air, linear and nonlinear relationships have been reported with urinary arsenic. Pinto et al. (1976) reported a linear relationship up to 150 μg/m3 of arsenic, whereas Enterline et al. (1987) reported a nonlinear relationship with higher arsenic air concentrations. The nonlinear relationship was attributed to either the use of respirators by the workers at high arsenic air concentrations or changes in their arsenic storage or excretion mechanisms.
Table 3.
Quantitative relationships between the concentration of arsenic in exposure media and in urine or nails.
| Exposure media | Biologic sample | Quantitative relationship | Reference |
|---|---|---|---|
| Air (3–295 μg As/m3) | Urine (μg/L) | Cair = 0.3Curine (p < 0.01, r = 0.53) | Pinto et al. 1976 |
| Air (50–3,500 μg As/m3) | Urine (μg/L) | Cair = 0.0064(Curine)1.94 | Enterline et al. 1987 |
| Air (< 0.1–35 μg As/m3) | Nails (μg/g) | Cair = 1.79Cnail–5.9 | Agahian et al. 1990 |
| Water (8–620 μg As/L) | Urine (μg/mg creatinine) | 10−2.57(Cwater)0.63 = logCurine (p < 0.001, r = 0.655) | Calderon et al. 1999 |
| Soil (102–356 μg As/g) | Urine (μg/L) | 0.1955(logCsoil) + 0.4818 = logCurine (p < 0.001, r = 0.25) | Hwang et al. 1997 |
| Soil (9–139 μg As/g) | Urine (μg/L) | 3.025(Csoil)0.237 = Curine (p < 0.01, r = 0.21) | Ranft et al. 2003 |
Certain foods contain organic arsenicals that can confound total urinary arsenic analysis. Some seafood contains high levels of arsenobetaine, an organic arsenical that is relatively nontoxic and excreted rapidly in urine intact (Vahter et al. 1983). Seaweed and marine algae contain arsenosugars that are metabolized to DMAV after consumption and excreted in urine (Francesconi et al. 2002; Le et al. 1994; Ma and Le 1998). Aspects relating to the metabolism of arsenosugars have become more complex because of the recent identification of dimethylarsenic sulfur and acetate compounds in urine of sheep that ingested seaweed (Hansen et al. 2003, 2004). In an iAs exposure analysis for which seafood ingestion is suspected, speciation of urinary arsenic as well as determination of total urinary arsenic would be critical. If only total urinary arsenic was determined, exposure to iAs may be overestimated. For iAs exposure assessments, subjects should refrain from ingesting seafood 2–3 days before collection of urine.
Other concerns of urinary arsenic analysis are sample collection times (24 hr, spot, first morning void) and whether to adjust the data to volume of urine voided (related to urinary creatinine levels or specific gravity). Collection of urine for 24 hr can be difficult, because of quality assurance logistics, particularly if a large number of samples are to be collected. Urinary arsenic does not appear to vary over time, so spot collection or first morning void may be used (Calderon et al. 1999; Hewitt et al. 1995). In addition, intraindividual variation of iAs metabolism and its urinary excretion was low over a 5-day period (Concha et al. 2002). This suggests that methylation of arsenic may be steady over time by an individual who is continuously exposed to the same level of arsenic.
Blood
Arsenic is cleared from blood within a few hours after it is absorbed (NRC 1999). Analysis of blood for arsenic is best suited for recent high-dose exposures. Background arsenic blood levels range from 0.5 to 2 μg/L (NRC 1999). Even though blood may attain steady-state levels after chronic exposure to iAs, it may not be a reliable biomarker of arsenic exposure because it is cleared so rapidly, particularly for low levels of iAs (ATSDR 2000).
A poor relationship exists between arsenic levels in drinking water and blood (WHO 2001). For levels of iAs in drinking water that ranged from 2.5 to 31 μg/L in a group of Andean women, blood arsenic levels were < 2 μg/L, and the total urinary arsenic concentration increased from 13 to 45 μg/L. In a group exposed to 200 μg/L iAs in water, blood arsenic levels increased to 8 μg/L, but total urinary arsenic increased to 261 μg/L (Vahter et al. 1995).
Blood is a more difficult matrix to work with than urine, and collection of it is an invasive procedure. Fewer subjects may participate in a blood collection study. Total arsenic analysis in blood may also present a problem if seafood was consumed by the subjects. Thus, if blood is to be sampled for determination of arsenic for exposure analysis, careful planning and a consistent sampling strategy should be employed.
Hair and nails
Absorbed arsenic accumulates in hair and nails. This is thought to be due to the binding of AsIII to sulfhydryl groups in keratin. Because hair and nails grow slowly, their analysis may give an indication of past arsenic exposure. Background arsenic levels in hair are < 1 μg/g (Hindmarsh 2002) and in nails range from < 1.5 to 7.7 μg/g (Agahian et al. 1990; Hinwood et al. 2003). iAs is the predominant form of arsenic in hair, with small amounts of dimethylated arsenic (Yamauchi et al. 1989). Based on animal studies, arsenobetaine does not accumulate in hair (Vahter et al. 1983), so consumption of seafood should not be a complicating factor in arsenic hair analysis.
Increased concentrations of arsenic in hair are observed in populations exposed to elevated levels of iAs in drinking water (Hinwood et al. 2003; Kurttio et al. 1998), air (Yamauchi et al. 1989), and soil (Hinwood et al. 2003). Kurttio et al. (1998) reported a significant correlation between arsenic in hair with total urinary arsenic (r = 0.75, p < 0.001), arsenic in drinking water (r = 0.74, p < 0.001), and daily dose of arsenic (r = 0.77, p < 0.001). With an increase of 10 μg/L of arsenic in drinking water, arsenic in hair increased 0.1 μg/g.
Populations exposed to elevated levels of iAs in drinking water (Hinwood et al. 2003), air (Agahian et al. 1990), and soil (Hinwood et al. 2003) show increased levels of arsenic in nails. Karagas et al. (1996) reported a significant correlation between detectable levels of arsenic in drinking water (> 1 μg/L) and in toenails (r = 0.83, p = 0.0001). With a 10-fold increase in arsenic in well water, the toenail arsenic concentration increased about 2-fold. In a follow-up study with a larger sample size, a significant correlation (r = 0.46, p < 0.001) between arsenic in water (0.002–66.6 μg/L) and nails (< 0.01–0.81 μg/g) was observed (Karagas et al. 2000).
The collection of hair and nails is not as invasive as collecting blood; more subjects may be willing to participate in iAs exposure studies if hair and nails are collected. A major issue in the use of hair and nails as biomarkers of exposure is their adsorption of arsenic from external sources (Hindmarsh 2002). For someone who consumes and bathes in water or is in contact with soil with elevated levels of iAs, arsenic from internal and external exposure would most likely be detected in hair and nails. This would complicate the exposure analysis. Although washing procedures have been developed, the possibility exists that this procedure may remove arsenic in the specimens that originated from internal sources. It is also not presently possible to distinguish between externally and internally derived arsenic in hair (Hindmarsh 2002).
Exposure Assessment
Food and drinking water are the principal sources of nonoccupational exposure to iAs for most populations. The daily dietary intake of iAs for an adult in the United States ranges from 8 to 14 μg/day (Yost et al. 1998). Approximately 98% of the U.S. population ingests water containing < 10 μg As/L (Chappell et al. 1997). Thus, the nonoccupational exposure to iAs in most of the adult U.S. population (regular diet and 2 L of water/day) is < 50 μg/day. There are regions in the United States and the world where arsenic levels in drinking water are significantly elevated. If this water is regularly ingested, exposure to iAs would be significantly increased. Other sources of iAs exposure are soils at Superfund sites and where arsenical pesticides were produced or used. Wolz et al. (2003) reported on elevated levels of arsenic in and around homes constructed on or near fruit orchards in agricultural communities with historical use of lead arsenate. This study showed strong correlations between indoor and outdoor concentrations of arsenic and hence provided evidence for a “track-in” exposure pathway for residential environments. Occupational exposure of arsenic can occur at smelters, coal burning facilities, or arsenic pesticide manufacturing sites via inhalation. Populations that reside near these industries also have the potential for exposure to arsenic.
Walker and Griffin (1998) used an exposure assessment model (U.S. EPA 1989) to predict urinary arsenic concentrations of children living near a Superfund site. Using this model and site-specific data, the predicted urinary arsenic concentrations reasonably agreed with the measured urinary arsenic concentrations. The predicted risks from exposure to iAs using the site-specific data in the exposure model were less than those predicted risks using default values. The results of this study, which used biomonitoring data, show that current risk assessment approaches using default values can be conservative by overestimating risk.
Evaluation of trends in exposure
Analysis of urine and blood is typically used for recent exposure to iAs. This is because arsenic is rapidly cleared from the blood and excreted in the urine after its systemic absorption (NRC 1999). Hair and nails may be used to assess past exposure to iAs. A major question in the use of urinary arsenic as a biomarker of exposure is how to relate the recent exposure, measured by urinary arsenic, to exposures that may have occurred chronically. Sporadic episodes of higher exposures within a chronic exposure context are also difficult to determine.
Uniquely exposed populations
There are populations in India, Bangladesh, and other countries that are exposed to exceedingly high levels of iAs in their drinking water (Chatterjee et al. 1995; Nordstrom 2002). Children also represent a subgroup for unique exposure to iAs. Children differ from adults in that they are still developing and have dissimilar food and water consumption patterns and exposure to media, such as soil and CCA-treated wood, which may have a significant impact on the total exposure. Polissar et al. (1990) examined pathways of arsenic exposure in a population that resided near a copper smelter. These pathways included outdoor and indoor air, soil, and house dust. Elevated urinary arsenic levels were found primarily in children younger than 6 years who lived within 0.5 miles of the smelter. Hand-to-mouth activity appeared to be the main source of arsenic exposure to these children. In utero exposure to iAs, primarily from mothers consuming elevated iAs in drinking water, may represent another unique type of exposure. Knowledge of the effects of this type of exposure is limited, although elevated adverse pregnancy outcomes (e.g., stillbirths) have been reported in Bangladeshi women chronically exposed to iAs in drinking water (Ahmad et al. 2001).
Effectiveness of an Intervention or Regulatory Action
The actions of governmental and nongovernmental organizations (Chowdhury 2004; Smith et al. 2000) that are attempting to reduce the drinking water exposure of iAs in the Bangladesh population are an example of the confirmed relationship of arsenic exposure, biomarkers, and health effects. Because of the relationship between drinking water exposure to iAs and development of cancer, the U.S. EPA lowered the arsenic drinking water MCL from 50 to 10 μg/L (U.S. EPA 2001). The U.S. Food and Drug Administration (2005) recently revised the bottled water quality standard at the same level. The WHO lowered its recommended arsenic drinking water guideline from 50 to 10 μg/L in 1993.
Approximately 2% of the U.S. population will be above the revised MCL for arsenic in 2006. One way to follow the effectiveness of this MCL would be to analyze urinary arsenic from a segment of this population after their arsenic drinking water levels are decreased. Hopenhayn-Rich et al. (1996) analyzed urine from a population previously exposed to high iAs (600 μg/L) drinking water levels and had switched to water containing less arsenic (45 μg/L). The average urinary arsenic levels in this population decreased from 636 to 166 μg As/L.
Conclusions and Recommendations for Future Research
iAs is a ubiquitous environmental contaminant. Human exposure to it occurs from many types of media. Analytical techniques have been developed that can detect low levels of iAs in biologic samples. Based on the oral RfD and drinking water MCL, it appears that there are levels of iAs that most humans can be exposed to without the development of adverse outcomes. However, many questions about iAs still exist, and the recommendations listed below may aid in decreasing these uncertainties:
Link biomarkers of arsenic exposure to effect.
Standardize a method for arsenic species analysis in biological samples that ensures good quality assurance and control and considers stability issues after sample collection.
Determine the mechanism of action for arsenic.
Examine the intra- and interindividual variability of arsenic methylation and effect.
Assess the efficacy of lowering the arsenic drinking water MCL from 50 to 10 μg/L.
Understand the magnitude and duration of exposure to iAs.
Develop physiologically based pharmacokinetic models for iAs low-dose extrapolation.
Quantify the contribution of arsenosugars to dimethylarsenic levels in urine.
Assess contribution of arsenic in diet to overall exposure.
Many of the studies referenced here have observed a significant and positive correlation between iAs in an exposure medium and arsenic in a biologic sample, principally urine, hair, and nails. With proper precautions and recognition of their limitations, analysis of these samples can be informative regarding whether an exposure to iAs occurred. It would be ideal if the biomarkers of exposure for iAs were linked to target tissue dose and, perhaps more important, to an adverse health effect in humans. For example, Enterline et al. (1987) reported a linear relationship between respiratory cancer mortality based on standardized mortality ratios and total urinary arsenic in smelter workers. More studies like Enterline et al. (1987) as well as in other areas are needed to develop a more robust risk assessment for iAs and enhance public health protection.
Footnotes
This article is part of the mini-monograph “Use of Biomonitoring Data in Exposure and Human Health Risk Assessments.”
I thank L. Birnbaum, E. Faustman, J. Mumford, S. Robison, D. Thomas, and K. Thomas for their helpful comments.
This article has been reviewed in accordance with the policy of the National Health and Environmental Effects Research Laboratory, U.S. EPA, and approved for publication. Approval does not signify that the contents necessarily reflect the views and policies of the agency, nor does mention of trade names or commercial products constitute endorsement or recommendation for use.
References
- Agahian B, Lee JS, Nelson JH, Johns RE. Arsenic levels in fingernails as a biological indicator of exposure to arsenic. Am Ind Hyg Assoc J. 1990;51:646–651. doi: 10.1080/15298669091370293. [DOI] [PubMed] [Google Scholar]
- Ahmad SA, Sayed MHSU, Barua S, Khan MH, Faruquee MH, Jalil A, et al. Arsenic in drinking water and pregnancy outcomes. Environ Health Perspect. 2001;109:629–631. doi: 10.1289/ehp.01109629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Conference of Governmental Industrial Hygienists 2004. TLVs and BEIs. Cincinnati, OH:Signature Publications.
- Aposhian HV, Gurzau ES, Le X, Gurzau A, Healy SM, Lu X, et al. Occurrence of monomethylarsonous acid in urine of humans exposed to inorganic arsenic. Chem Res Toxicol. 2000;13:693–697. doi: 10.1021/tx000114o. [DOI] [PubMed] [Google Scholar]
- Aposhian HV, Zakharyan RA, Avram MD, Sampayo-Reyes A, Wollenberg ML. A review of the enzymology of arsenic metabolism and a new potential role of hydrogen peroxide in the detoxication of the trivalent arsenic species. Toxicol Appl Pharmacol. 2004;198:327–335. doi: 10.1016/j.taap.2003.10.027. [DOI] [PubMed] [Google Scholar]
- Arnold LL, Cano M, St John M, Eldan M, van Gemert M, Cohen SM. Effects of dietary dimethylarsinic acid on the urine and urothelium of rats. Carcinogenesis. 1999;20:2175–2179. doi: 10.1093/carcin/20.11.2171. [DOI] [PubMed] [Google Scholar]
- Arnold LL, Eldan M, van Gemert M, Capen CC, Cohen SM. Chronic studies evaluating the carcinogenicity of monomethylarsonic acid in rats and mice. Toxicology. 2003;1990:197–219. doi: 10.1016/s0300-483x(03)00165-3. [DOI] [PubMed] [Google Scholar]
- ATSDR 2000. Toxicological Profile for Arsenic. Atlanta, GA:Agency for Toxic Substances and Disease Registry. [PubMed]
- B’Hymer C, Caruso JA. Arsenic and its speciation analysis using high-performance liquid chromatography and inductively coupled plasma mass spectrometry. J Chromatogr A. 2004;1045:1–13. doi: 10.1016/j.chroma.2004.06.016. [DOI] [PubMed] [Google Scholar]
- Biggs ML, Kalman DA, Moore LE, Hopenhayn-Rich C, Smith MT, Smith AH. Relationship of urinary arsenic to intake estimates and a biomarker of effect, bladder cell micronuclei. Mutat Res. 1997;386:185–195. doi: 10.1016/s1383-5742(97)00012-4. [DOI] [PubMed] [Google Scholar]
- Buchet JP, Hoet P, Haefroid V, Lison D. 1999. Consistency of biomarkers of exposure to inorganic arsenic: review of recent data. In: Arsenic Exposure and Health Effects (Chappell WR, Abernathy CO, Calderon RL, eds). Oxford:Elsevier Science, 31–40.
- Burns FJ, Uddin AN, Wu F, Nadas A, Rossman TG. Arsenic-induced enhancement of uv radiation carcinogenesis in mouse skin: a dose-response study. Environ Health Perspect. 2004;112:599–603. doi: 10.1289/ehp.6655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calderon RL, Hudgens E, Le XC, Schreinemachers D, Thomas DJ. Excretion of arsenic in urine as a function of exposure to arsenic in drinking water. Environ Health Perspect. 1999;107:663–667. doi: 10.1289/ehp.99107663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chappell WR, Beck BD, Brown KG, Chaney R, Cothern CR, Irgolic KJ, et al. Inorganic arsenic: a need and an opportunity to improve risk assessment. Environ Health Perspect. 1997;105:1060–1067. doi: 10.1289/ehp.971051060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee A, Das D, Mandal BK, Chowdhury TR, Samanta G, Chakraborti D. Arsenic in ground water in six districts of West Bengal, India: the biggest arsenic calamity in the world. Part 1. Arsenic species in drinking water and urine of the affected people. Analyst. 1995;120:643–650. doi: 10.1039/an9952000917. [DOI] [PubMed] [Google Scholar]
- Chen C-J, Hsu L-I, Wang C-H, Shih W-L, Hsu Y-H, Tseng M-P, et al. Biomarkers of exposure, effect and susceptibility of arsenic-induced health hazards in Taiwan. Toxicol Appl Pharmacol. 2005;206:198–206. doi: 10.1016/j.taap.2004.10.023. [DOI] [PubMed] [Google Scholar]
- Chen Y. K6/ODC transgenic mice as a sensitive model for carcinogen identification. Toxicol Lett. 2000;116:27–35. doi: 10.1016/s0378-4274(00)00196-x. [DOI] [PubMed] [Google Scholar]
- Chen YC, Amarasiriwardena CJ, Hsueh YM, Christani DC. Stability of arsenic species and insoluble arsenic in human urine. Cancer Epidemiol Biomarkers Prev. 2002;11:1427–1433. [PubMed] [Google Scholar]
- Chowdhury AM. Arsenic crisis in Bangladesh. Sci Am. 2004;291:86–91. doi: 10.1038/scientificamerican0804-86. [DOI] [PubMed] [Google Scholar]
- Concha C, Vogler G, Nermell B, Vahter M. Intra-individual variation in the metabolism of inorganic arsenic. Int Arch Occup Environ Health. 2002;75:576–580. doi: 10.1007/s00420-002-0361-1. [DOI] [PubMed] [Google Scholar]
- Crecelius E, Yager J. Intercomparison of analytical methods for arsenic speciation in human urine. Environ Health Perspect. 1997;105:650–653. doi: 10.1289/ehp.97105650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Razo LM, Quintanilla-Vega B, Brambila-Colombres E, Calderon-Aranda ES, Manno M, Albores A. Stress proteins induced by arsenic. Toxicol Appl Pharmacol. 2001a;177:132–148. doi: 10.1006/taap.2001.9291. [DOI] [PubMed] [Google Scholar]
- Del Razo LM, Styblo M, Cullen WR, Thomas DJ. Determination of trivalent methylated arsenicals in biological matrices. Toxicol Appl Pharmacol. 2001b;174:282–293. doi: 10.1006/taap.2001.9226. [DOI] [PubMed] [Google Scholar]
- DeSesso JM, Jacobson CF, Scialli AR, Farr CH, Holson JF. An assessment of the developmental toxicity of inorganic arsenic. Reprod Toxicol. 1998;12:385–433. doi: 10.1016/s0890-6238(98)00021-5. [DOI] [PubMed] [Google Scholar]
- Devesa V, Del Razo LM, Adair B, Drobna Z, Waters SB, Hughes MF, et al. Comprehensive analysis of arsenic metabolites by pH-specific hydride generation atomic absorption spectrometry. J Anal At Spectrom. 2004;19:1–10. [Google Scholar]
- Dixon HBF. The biochemical action of arsonic acids especially as phosphate analogues. Adv Inorg Chem. 1997;44:191–227. [Google Scholar]
- Do B, Alet P, Pradeu D, Poupon J, Guilley-Gaillot M, Guyon F. On-line reversed-phase liquid chromatography hydride generation emission spectrometry: speciation of arsenic in urine of patients intravenously treated with As2O3. J Chromatogr B. 2000;740:179–186. doi: 10.1016/s0378-4347(00)00047-5. [DOI] [PubMed] [Google Scholar]
- Ellenhorn MJ. 1997. Ellenhorn’s Medical Toxicology: Diagnosis and Treatment of Human Poisoning. 2nd ed. Baltimore: Williams & Wilkins, 1540.
- Enterline PE, Henderson VL, Marsh GM. Exposure to arsenic and respiratory cancer—a reanalysis. Am J Epidemiol. 1987;125:929–923. doi: 10.1093/oxfordjournals.aje.a114631. [DOI] [PubMed] [Google Scholar]
- Feldmann J, Lai VM, Cullen WR, Ma M, Lu X, Le XC. Sample preparation and storage can change arsenic speciation in human urine. Clin Chem. 1999;45:1988–1997. [PubMed] [Google Scholar]
- Francesconi KA, Kuehnelt D. Determination of arsenic species: a critical review of methods and applications, 2000–2003. Analyst. 2004;129:373–395. doi: 10.1039/b401321m. [DOI] [PubMed] [Google Scholar]
- Francesconi KA, Tanggaard R, McKenzie CJ, Goessler W. Arsenic metabolites in human urine after ingestion of an arsenosugar. Clin Chem. 2002;48:92–101. [PubMed] [Google Scholar]
- Germolec DR, Spalding J, Boorman GA, Wilmer JL, Yoshida T, Simeonova PP, et al. Arsenic can mediate skin neoplasia by chronic stimulation of keratinocyte-derived growth factors. Mutat Res. 1997;386:209–218. doi: 10.1016/s1383-5742(97)00006-9. [DOI] [PubMed] [Google Scholar]
- Gong Z, Lu X, Ma M, Watt C, Le XC. Arsenic speciation analysis. Talanta. 2002;58:77–96. doi: 10.1016/s0039-9140(02)00258-8. [DOI] [PubMed] [Google Scholar]
- Hansen H, Raab A, Feldmann J. New arsenosugar metabolite determined in urine by parallel use of HPLC-ICP-MS and HPLC-ESI-MS. J Anal Atom Spectrom. 2003;18:474–479. [Google Scholar]
- Hansen HR, Raab A, Jaspars M, Milne BF, Feldmann J. Sulfur-containing arsenical mistaken for dimethylarsinous acid [DMA(III)] and identified as a natural metabolite in urine: major implications for studies on arsenic metabolism and toxicity. Chem Res Toxicol. 2004;17:1086–1091. doi: 10.1021/tx049978q. [DOI] [PubMed] [Google Scholar]
- Hewitt DJ, Millner GC, Nye AC, Simmons HF. Investigation of arsenic exposure from soil at a Superfund site. Environ Res. 1995;68:73–81. doi: 10.1006/enrs.1995.1010. [DOI] [PubMed] [Google Scholar]
- Hindmarsh T. Caveats in hair analysis in chronic arsenic poisoning. Clin Biochem. 2002;35:1–11. doi: 10.1016/s0009-9120(01)00282-x. [DOI] [PubMed] [Google Scholar]
- Hinwood AL, Sim RR, Jolley D, de Klerk N, Bastone EB, Gerostamoulos J, et al. Hair and toenail arsenic concentrations of residents living in areas with high environmental arsenic concentrations. Environ Health Perspect. 2003;111:187–193. doi: 10.1289/ehp.5455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopenhayn-Rich C, Biggs ML, Kalman DA, Moore LE, Smith AH. Arsenic methylation patterns before and after changing from high to lower concentrations of arsenic in drinking water. Environ Health Perspect. 1996;104:1200–1207. doi: 10.1289/ehp.961041200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes MF. Arsenic toxicity and potential mechanisms of action. Toxicol Lett. 2002;133:1–16. doi: 10.1016/s0378-4274(02)00084-x. [DOI] [PubMed] [Google Scholar]
- Hwang YH, Bornschein RL, Grote J, Menrath W, Roda S. Environmental arsenic exposure of children around a former copper smelter site. Environ Res. 1997;72:72–81. doi: 10.1006/enrs.1996.3691. [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer. Arsenic and arsenic compounds. IARC Monogr Eval Carcinog Risks Hum. 1987;23(suppl 7):100–103. [Google Scholar]
- Karagas MR, Morris JS, Weiss JE, Spate V, Baskett C, Greenberg ER. Toenail samples as an indicator of drinking water arsenic exposure. Cancer Epidemiol Biomarkers Prev. 1996;5:849–852. [PubMed] [Google Scholar]
- Karagas MR, Tosteson TD, Blum J, Klaue B, Weiss JE, Stannard V, et al. Measurement of low levels of arsenic exposure: a comparison of water and toenail concentrations. Am J Epidemiol. 2000;152:84–90. doi: 10.1093/aje/152.1.84. [DOI] [PubMed] [Google Scholar]
- Kitchin KT. Recent advances in arsenic carcinogenesis: modes of action, animal models and methylated arsenic metabolites. Toxicol Appl Pharmacol. 2001;172:249–261. doi: 10.1006/taap.2001.9157. [DOI] [PubMed] [Google Scholar]
- Kurttio P, Komulainen H, Hakala E, Kahelin H, Pekkanen J. Urinary excretion of arsenic species after exposure to arsenic present in drinking water. Arch Environ Contam Toxicol. 1998;34:297–305. doi: 10.1007/s002449900321. [DOI] [PubMed] [Google Scholar]
- Kwon E, Zhang H, Wang Z, Jhangri GS, Lu X, Fok N, et al. Arsenic on the hands of children after playing in playgrounds. Environ Health Perspect. 2004;112:1375–1380. doi: 10.1289/ehp.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le XC, Cullen WR, Reimer KJ. Human urinary arsenic excretion after one-time ingestion of seaweed, crab and shrimp. Clin Chem. 1994;40:617–624. [PubMed] [Google Scholar]
- Le XC, Lu X, Ma M, Cullen WR, Aposhian HV, Zheng B. Speciation of key arsenic metabolic intermediates in human urine. Anal Chem. 2000;72:5172–5177. doi: 10.1021/ac000527u. [DOI] [PubMed] [Google Scholar]
- Loffredo CA, Aposhian HV, Cebrian ME, Yamauchi H, Silbergeld EK. Variability in human metabolism of arsenic. Environ Res. 2003;92:85–91. doi: 10.1016/s0013-9351(02)00081-6. [DOI] [PubMed] [Google Scholar]
- Ma M, Le XC. Effect of arsenosugar ingestion on urinary arsenic speciation. Clin Chem. 1998;14:539–550. [PubMed] [Google Scholar]
- Maki-Paakkanen J, Kurttio P, Paldy A, Pekkanen J. Association between the clastogenic effect in peripheral lymphocytes and human exposure to arsenic through drinking water. Environ Mol Mutagen. 1998;32:301–313. doi: 10.1002/(sici)1098-2280(1998)32:4<301::aid-em3>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Mandal BK, Ogra Y, Anzai K, Suzuki KT. Speciation of arsenic in biological samples. Toxicol Appl Pharmacol. 2004;198:307–318. doi: 10.1016/j.taap.2003.10.030. [DOI] [PubMed] [Google Scholar]
- Mandal BK, Ogra Y, Suzuki KT. Identification of dimethylarsinous and monomethylarsonous acids in human urine of the arsenic-affected areas in West Bengal, India. Chem Res Toxicol. 2001;14:371–378. doi: 10.1021/tx000246h. [DOI] [PubMed] [Google Scholar]
- NRC 1999. Arsenic in Drinking Water. Washington, DC:National Research Council.
- NRC. 2001. Arsenic in Drinking Water 2001 Update. Washington, DC:National Research Council.
- Nordstrom DK. Worldwide occurrences of arsenic in groundwater. Science. 2002;296:2144–2145. doi: 10.1126/science.1072375. [DOI] [PubMed] [Google Scholar]
- Petrick JS, Ayala-Fierio F, Cullen WR, Carter DE, Aposhian HV. Monomethylarsonous acid (MMA(III)) is more toxic than arsenite in Chang human hepatocytes. Toxicol Appl Pharmacol. 2000;163:203–207. doi: 10.1006/taap.1999.8872. [DOI] [PubMed] [Google Scholar]
- Petrick JS, Jagadish B, Mash EA, Aposhian HV. Monomethylarsonous acid (MMA(III)) and arsenite: LD(50) in hamsters and in vitro inhibition of pyruvate dehydrogenase. Chem Res Toxicol. 2001;14:651–666. doi: 10.1021/tx000264z. [DOI] [PubMed] [Google Scholar]
- Pinto SS, Varner MO, Nelson KW, Labbe AL, White LD. Arsenic trioxide absorption and excretion in industry. J Occup Med. 1976;18:677–680. doi: 10.1097/00043764-197610000-00009. [DOI] [PubMed] [Google Scholar]
- Polissar L, Lowry-Coble K, Kalman DA, Hughes JP, van Belle G, Covert DS, et al. Pathways of human exposure to arsenic in a community surrounding a copper smelter. Environ Res. 1990;53:29–47. doi: 10.1016/s0013-9351(05)80128-8. [DOI] [PubMed] [Google Scholar]
- Ranft U, Miskovic P, Pesch B, Jakubis P, Fabianova E, Keegan T, et al. Association between arsenic exposure from a coal-burning power plant and urinary arsenic concentrations in Prievidza District, Slovakia. Environ Health Perspect. 2003;111:889–894. doi: 10.1289/ehp.5838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossman TG. Mechanism of arsenic carcinogenesis: an integrated approach. Mutat Res. 2003;533:37–65. doi: 10.1016/j.mrfmmm.2003.07.009. [DOI] [PubMed] [Google Scholar]
- Schoof RA, Yost LJ, Eickhoff J, Crecelius EA, Cragin DW, Meachem DM, et al. A marketbasket survey of inorganic arsenic in food. Food Chem Toxicol. 1999;37:839–846. doi: 10.1016/s0278-6915(99)00073-3. [DOI] [PubMed] [Google Scholar]
- Shen J, Wanibuchi H, Salim EI, Wei M, Doi K, Yoshida K, et al. Induction of glutathione S-transferase placental form positive foci in liver and epithelial hyperplasia in urinary bladder, but not tumor development in male Fischer 344 rats treated with monomethylarsonic acid for 104 weeks. Toxicol Appl Pharmacol. 2003a;193:335–345. doi: 10.1016/s0041-008x(03)00245-x. [DOI] [PubMed] [Google Scholar]
- Shen J, Wanibuchi H, Salim EI, Wei M, Kinoshita A, Yoshida K, et al. Liver tumorigenicity of trimethylarsine oxide in male Fischer 344 rats—association with oxidative DNA damage and enhanced cell proliferation. Carcinogenesis. 2003b;24:1827–1835. doi: 10.1093/carcin/bgg143. [DOI] [PubMed] [Google Scholar]
- Smith AH, Lingas EO, Rahman M. Contamination of drinking-water by arsenic in Bangladesh: a public health emergency. Bull World Health Organ. 2000;78:1093–1103. [PMC free article] [PubMed] [Google Scholar]
- Styblo M, Del Razo LM, Vega L, Germolec DR, LeCluyse EL, Hamilton GA, et al. Comparative toxicity of trivalent and pentavalent inorganic and methylated arsenicals in rat and human cells. Arch Toxicol. 2000;74:289–299. doi: 10.1007/s002040000134. [DOI] [PubMed] [Google Scholar]
- Sur R, Dunemann L. Method for the determination of five toxicologically relevant arsenic species in human urine by liquid chromatography-hydride generation atomic absorption spectrometry. J Chromatogr B. 2004;807:169–176. doi: 10.1016/j.jchromb.2004.03.051. [DOI] [PubMed] [Google Scholar]
- Tao SS-H, Bolger PM. Dietary arsenic intakes in the United States: FDA Total Diet Study, September 1991–December 1996. Food Addit Contam. 1998;16:465–472. doi: 10.1080/026520399283759. [DOI] [PubMed] [Google Scholar]
- Thomas DJ, Styblo M, Lin S. The cellular metabolism and systemic toxicity of arsenic. Toxicol Appl Pharmacol. 2001;176:127–144. doi: 10.1006/taap.2001.9258. [DOI] [PubMed] [Google Scholar]
- Thomas DJ, Waters SB, Styblo M. Elucidating the pathway for arsenic methylation. Toxicol Appl Pharmacol. 2004;198:319–326. doi: 10.1016/j.taap.2003.10.020. [DOI] [PubMed] [Google Scholar]
- Tseng WP. Effects and dose-response relationships of skin cancer and blackfoot disease with arsenic. Environ Health Perspect. 1977;19:109–119. doi: 10.1289/ehp.7719109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng WP, Chu HM, How SW, Fong JM, Lin CS, Yeh S. Prevalence of skin cancer in an endemic area of chronic arsenicism in Taiwan. J Natl Cancer Inst. 1968;40:453–463. [PubMed] [Google Scholar]
- U.S. EPA 1989. Risk Assessment Guidance for Superfund. Vol 1: Human Health Evaluation Manual. OSWER Directive 9285.7-01a. Washington, DC:U.S. Environmental Protection Agency.
- U.S. EPA 1993. Arsenic, Inorganic (CASRN 7440-38-2), Integrated Risk Information System. Washington, DC:U.S. Environmental Protection Agency. Available: http://www.epa.gov/iris/subst/0278.htm [31 March 2005].
- U.S. EPA (U.S. Environmental Protection Agency) 2001. National primary drinking water regulations: arsenic and clarifications to compliance and new source contaminants monitoring. Final rule. Fed Reg 66:6976–7066.
- U.S. Food and Drug Administration. Beverages: bottled water. Final rule. Fed Reg. 2005;70:33694–33701. [PubMed] [Google Scholar]
- Vahter M. Genetic polymorphisms in the biotransformation of inorganic arsenic and its role in toxicity. Toxicol Lett. 2000;112:209–217. doi: 10.1016/s0378-4274(99)00271-4. [DOI] [PubMed] [Google Scholar]
- Vahter M, Concha G, Nermell B, Nilsson R, Dulout F, Natarajan AT. A unique metabolism of inorganic arsenic in native Andean women. Eur J Pharmacol. 1995;293:455–462. doi: 10.1016/0926-6917(95)90066-7. [DOI] [PubMed] [Google Scholar]
- Vahter M, Marafante E, Dencker L. Metabolism of arsenobetaine in mice, rats and rabbits. Sci Total Environ. 1983;30:197–211. doi: 10.1016/0048-9697(83)90012-8. [DOI] [PubMed] [Google Scholar]
- Valberg PA, Beck BD, Bowers TS, Keating JL, Bergstrom PD. Issues in setting health-based cleanup levels for arsenic in soil. Regul Toxicol Pharmacol. 1997;26:219–229. doi: 10.1006/rtph.1997.1148. [DOI] [PubMed] [Google Scholar]
- Waalkes MP, Liu J, Ward JM, Diwan BA. Animal models for arsenic carcinogenesis: inorganic arsenic is a transplacental carcinogen in mice. Toxicol Appl Pharmacol. 2004;98:377–384. doi: 10.1016/j.taap.2003.10.028. [DOI] [PubMed] [Google Scholar]
- Walker S, Griffin S. Site-specific data confirm arsenic exposure predicted by the U.S. Environmental Protection Agency. Environ Health Perspect. 1998;106:133–139. doi: 10.1289/ehp.98106133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang JP, Qi L, Zheng B, Liu F, Moore MR, Ng JC. Porphyrins as early biomarkers for arsenic exposure in animals and humans. Cell Mol Biol. 2002;48:835–843. [PubMed] [Google Scholar]
- Wanibuchi H, Salim EI, Kinoshita A, Shen J, Wei M, Morimura K, et al. Understanding arsenic carcinogenicity by the use of animal models. Toxicol Appl Pharmacol. 2004;198:366–376. doi: 10.1016/j.taap.2003.10.032. [DOI] [PubMed] [Google Scholar]
- Wei M, Wanibuchi H, Yamamoto S, Li W, Fukushima S. Urinary bladder carcinogenicity of dimethylarsinic acid in male F344 rats. Carcinogenesis. 1999;20:1873–1876. doi: 10.1093/carcin/20.9.1873. [DOI] [PubMed] [Google Scholar]
- WHO 2001. Arsenic and Arsenic Compounds. 2nd ed. Environmental Health Criteria 224. Geneva:World Health Organization.
- Wolz S, Fenske RA, Simcox NJ, Palcisko G, Kissel JC. Residential arsenic and lead levels in an agricultural community with a history of lead arsenate use. Environ Res. 2003;92:293–300. doi: 10.1016/s0013-9351(03)00064-1. [DOI] [PubMed] [Google Scholar]
- Yamauchi H, Takahashi K, Mushiko M, Yamamura Y. Biological monitoring of arsenic exposure of gallium arsenide- and inorganic arsenic-exposed workers by determination of inorganic arsenic and its metabolites in urine and hair. Am Ind Hyg Assoc J. 1989;50:606–612. doi: 10.1080/15298668991375236. [DOI] [PubMed] [Google Scholar]
- Yoshinaga J, Chatterjee A, Shibata Y, Morita M, Edmonds JS. Human urine certified reference material for arsenic speciation. Clin Chem. 2000;46:1781–1786. [PubMed] [Google Scholar]
- Yost LJ, Schoof RA, Auroin R. Intake of inorganic arsenic in the North American diet. Hum Ecol Risk Assess. 1998;4:137–152. [Google Scholar]


