Abstract
We tested the hypotheses that: (1) neutrophil accumulation after contraction-induced muscle injury is dependent on the β2 integrin CD18, (2) neutrophils contribute to muscle injury and oxidative damage after contraction-induced muscle injury, and (3) neutrophils aid the resolution of contraction-induced muscle injury. These hypotheses were tested by exposing extensor digitorum longus (EDL) muscles of mice deficient in CD18 (CD18−/−; Itgb2tm1Bay) and of wild type mice (C57BL/6) to in situ lengthening contractions and by quantifying markers of muscle inflammation, injury, oxidative damage and regeneration/repair. Neutrophil concentrations were significantly elevated in wild type mice at 6 h and 3 days post-lengthening contractions; however, neutrophils remained at control levels at these time points in CD18−/− mice. These data indicate that CD18 is required for neutrophil accumulation after contraction-induced muscle injury. Histological and functional (isometric force deficit) signs of muscle injury and total carbonyl content, a marker of oxidative damage, were significantly higher in wild type relative to CD18−/− mice 3 days after lengthening contractions. These data show that neutrophils exacerbate contraction-induced muscle injury. After statistically controlling for differences in the force deficit at 3 days, wild type mice also demonstrated a higher force deficit at 7 days, a lower percentage of myofibres expressing embryonic myosin heavy chain at 3 and 7 days, and a smaller cross sectional area of central nucleated myofibres at 14 days relative to CD18−/− mice. These observations suggest that neutrophils impair the restoration of muscle structure and function after injury. In conclusion, neutrophil accumulation after contraction-induced muscle injury is dependent on CD18. Furthermore, neutrophils appear to contribute to muscle injury and impair some of the events associated with the resolution of contraction-induced muscle injury.
Skeletal muscle injury, induced by lengthening contractions (Best et al. 1999; Pizza et al. 2002; McLoughlin et al. 2003a; Tsivitse et al. 2003), trauma (Papadimitriou et al. 1990; Orimo et al. 1991), and the mechanical loading of atrophic muscle (Tidball et al. 1999; Frenette et al. 2002), causes neutrophils to accumulate in skeletal muscle. Interestingly, neutrophils are elevated when ultrastructural, histological and functional signs of muscle injury worsen (Newham et al. 1983; Faulkner et al. 1989) and when the injured muscle begins to show signs of muscle regeneration/repair (e.g. myoblast proliferation, myotube formation and removal of cellular debris) (Darr & Schultz, 1987; Papadimitriou et al. 1990; Grounds et al. 1992; Rosenblatt & Woods, 1992; Robertson et al. 1993; Hawke & Garry, 2001). The mechanism for the entry of neutrophils into injured skeletal muscle and their function in injured skeletal muscle, however, is poorly understood.
Neutrophils enter into tissue via a complex series of events that begins with their adhesion to vascular endothelial cells and culminates with diapedesis (Kishimoto & Rothlein, 1994; Muller, 2003). Firm adhesion of neutrophils to endothelial cells, a prerequisite for diapedesis, is mediated by the interaction of a β2 integrin (αM/β2; CD11b/CD18) on neutrophils with vascular ligands such as intracellular adhesion molecule-1 (Kishimoto & Rothlein, 1994; Walzog & Gaehtgens, 2000). After firm adhesion, neutrophils pass between endothelial cells by interacting with adhesion molecules in the intercellular junction between endothelial cells and with extracellular matrix proteins (Sixt et al. 2001; Muller, 2003). Whether the accumulation of neutrophils in skeletal muscle after contraction-induced muscle injury is CD18 dependent, however, has yet to be determined.
The contribution of neutrophils to events associated with contraction-induced muscle injury and its resolution is largely unknown. Previous investigators have speculated that neutrophils cause muscle dysfunction and cytoskeletal disruptions after lengthening contractions. Support for this contention is derived from our own studies that demonstrated that neutrophils injure cultured skeletal muscle cells (myotubes) via mechanisms that are dependent on CD18-mediated neutrophil adhesion and reactive oxygen species (ROS) production (Pizza et al. 2001; McLoughlin et al. 2003b). Neutrophils could delay the resolution of the injury by damaging myotubes (Pizza et al. 2001; McLoughlin et al. 2003b) and/or by releasing cytokines (e.g. tumour necrosis factor-α (TNF-α) and interferon-γ (IFN-γ)) that are known to impair myoblast differentiation, myotube formation and/or protein synthesis (Kalovidouris et al. 1993; Frost et al. 1997; Cassatella, 1999; Langen et al. 2002). On the other hand, neutrophils could also facilitate the resolution of the injury by removing injured tissue via phagocytosis (Papadimitriou et al. 1990), by releasing cytokines (e.g. hepatocyte growth factor (HGF) and interleukin-6 (IL-6)) that could enhance myogenesis (Austin & Burgess, 1991; Allen et al. 1995; Cassatella, 1999; Miller et al. 2000), and/or by promoting the accumulation of macrophages, which are known to cause myoblast proliferation in vitro (Merly et al. 1999; Cantini et al. 2002), via the release of chemoattractants for monocytes (Grounds & Davies, 1996; Cassatella, 1999). Thus, in theory, neutrophils could impair and/or aid the resolution of a contraction-induced muscle injury via multiple mechanisms.
In the present study, we tested the hypothesis that the accumulation of neutrophils after contraction-induced muscle injury is dependent on CD18. To test this hypothesis, we exposed CD18-deficient (CD18−/−) and wild type mice to in situ lengthening contractions and quantified neutrophil and macrophage concentrations in skeletal muscle for 14 days after the injury. Because the CD18 deficiency prevented neutrophil accumulation after lengthening contractions, we also tested whether neutrophils contribute to muscle injury and aid its resolution after lengthening contractions. This hypothesis was tested by comparing markers of muscle injury, oxidative damage (carbonyl content) and muscle regeneration/repair between CD18−/− and wild type mice. Although the components of our second hypothesis may seem incongruent, we hypothesized that the injury induced by neutrophils is a necessary consequence for restoring normal structure and function to skeletal muscle after contraction-induced muscle injury.
Methods
Animals
Male wild type (C57BL/6; n = 31) and CD18−/− (Itgb2tm1Bay; C57BL/6 background; n = 34) mice were commercially obtained (Jackson Laboratory, Benton Harbour, MI, USA). The CD18−/− mice had a hypomorphic rather than a null allele for CD18 and unlike the null mutants, do not exhibit any known pathology nor die prematurely (Wilson et al. 1993). Mice were fed standard laboratory chow and had access to water ad libitum. Experimental procedures were approved by the animal care and use committees at the University of Illinois at Chicago and The University of Toledo.
In situ muscle preparation
Mice were anaesthetized with an intraperitoneal injection of 2% Avertin (tribromoethanol; 0.015 ml (g body mass)−1) with supplemental doses (0.1 ml) given as needed. Under anaesthesia, the distal tendon of the right and/or left extensor digitorum longus (EDL) muscle was exposed and tied to the lever arm of a servomotor (Aurora Scientific, Richmond Hill, ON, Canada) (Koh & Brooks, 2001). The incision site was kept moist with sterile physiological saline. Needle electrodes, placed around the peroneal nerve, were used to stimulate contraction of the EDL (Grass Instruments, Model S48; West Warwick, RI, USA). Pulse duration was kept constant (0.2 ms) whereas voltage, frequency and optimal muscle length (Lo) for isometric force development were determined separately for each animal as previously described (Koh & Brooks, 2001). Optimal fibre length (Lf) was determined by multiplying Lo by the Lf/Lo ratio of 0.44 (McCully & Faulkner, 1985).
The injury protocol consisted of lengthening EDL muscles through 20% strain relative to Lf with the muscles stimulated at 150 Hz. The protocol consisted of 75 repetitions performed at 0.25 Hz for a total exercise duration of 5 min. The incision was sutured closed and covered with betadine ointment. Mice recovered from the anaesthesia on a heated (37°C) platform.
At selected time points after lengthening contractions, maximal isometric force was redetermined as previously described. Maximal isometric force was then expressed as a deficit relative to values obtained prior to lengthening contractions. Mice were killed via cervical dislocation under anaesthesia at either 6 h, 3 days, 7 days or 14 days after lengthening contractions. The EDL muscles were excised with tendons intact, weighed, coated with optimal cutting temperature compound (Fisher Scientific), frozen in melting isopentane cooled on dry ice, and stored at −70°C. Because we have previously demonstrated that muscle function, histology and inflammatory cell concentrations were not influenced by sham surgical procedures (Pizza et al. 2002), control muscles consisted of contralateral muscles from mice in which the ipsilateral muscle had been exposed to the lengthening contraction protocol and from mice that had normal cage activity.
Inflammatory cells
Transverse sections (10 μm) were cut from the mid-belly of the muscles and were prepared for immunohistochemistry as previously described (Pizza et al. 2002). Neutrophils were identified using an anti-mouse Ly6G antibody (clone RB6-8C5; 1: 100 in phosphate buffered saline (PBS); PharMingen, Franklin Lake, NJ, USA; whereas macrophages were recognized using an anti-mouse F4/80 antibody (clone CI:A3-1; 1: 100 in PBS; Serotec Inc., Raleigh, NC, USA). Slides serving as negative controls received PBS instead of primary antibody. After a 2 h incubation at room temperature with the primary antibody, sections were washed in PBS, incubated with biotinylated mouse absorbed anti-rat IgG (1: 200 in PBS; Vector Laboratories Inc., Burlingame, CA, USA) followed by avidin D horseradish peroxidase (1: 1000 in PBS). Sections were then developed with 3-amino-9-ethylcarbazole (Vector).
Sections were viewed with a light microscope (Olympus IX-70) with Nomarski optics. Inflammatory cells in two entire sections for each muscle were manually counted and the total area of the section was measured using a calibrated square grid. The volume of muscle sampled was calculated as the product of the cross-sectional area of the section and the section thickness (10 μm). Inflammatory cells were expressed as number per cubic millimetre (mm3). The number of fibres invaded by neutrophils or macrophages were also counted and expressed as a percentage of the total number of fibres within the section.
Histology
Transverse sections (10 μm) were cut from the mid-belly of the muscles, stained with haematoxylin and eosin, and examined for signs of both injury and regeneration. Myofibres that showed a pale or discontinuous cytoplasmic staining, were substantially swollen in appearance, or were invaded by cells were classified as injured (Koh & Brooks, 2001). The number of injured myofibres in two entire sections for each muscle were counted and then expressed as a percentage of the total number of myofibres within each section. The number of myofibres in each section was manually counted.
The number of central nucleated myofibres was determined and used as a marker of muscle regeneration (Anderson, 1991; Thaloor et al. 1999). The number of central nucleated myofibres in two entire sections for each muscle were counted and then expressed as a percentage of the total number of myofibres within each section. Digital images were captured and the cross-sectional area (CSA) of central nucleated myofibres at 7 and 14 days post-lengthening contractions was determined in one entire section of each muscle using image analysis software (NIH Image; Version 1.62). We also determined the CSA of myofibres without centrally located nuclei (i.e. normal myofibres) to test whether the influence of the CD18 deficiency was restricted to regenerating myofibres.
Carbonyl content
Total carbonyl content, a measure of oxidative damage, was determined in EDL muscles obtained from control mice and from wild type and CD18−/− mice 3 days after lengthening contractions (Reznick & Packer, 1994). Muscles were homogenized in 50 mm phosphate buffer containing protease inhibitors (1 mm EDTA, 5 μg ml−1 leupeptin, 5 μg ml−1 aprotinin, and 100 μg ml−1 phenylmethylsulphonyl fluoride). Homogenates were centrifuged (2000 g, 4°C, 10 min) and protein content in the supernatants was determined via the filter paper dye-binding assay (Minamide & Bamburg, 1990). Protein in aliquots (100–150 μg) were then precipitated using 20% trichloroacetic acid (TCA, 10% final concentration) at 4°C for 1 h. Following centrifugation (15 000 g, 4°C, 20 min), pellets were washed with cold acetone, centrifuged, air dried and 2 m hydrochloric acid (HCl) or 10 mm 2,4-dinitrophenylhydrazine (DNPH) in 2 m HCl was added to blank and duplicate reaction tubes, respectively. Tubes were then incubated at room temperature and mixed every 15 min for 1 h. Proteins were then precipitated using 20% TCA (10% final concentration) and the pellets were washed with 10% TCA. To remove un-reacted DNPH, pellets were washed three times with ethanol: ethylacetate (1: 1). For each wash, pellets were vortexed, sonicated for 10 min, centrifuged (15 000 g, 4°C, 15 min), and the supernatants were discarded. The final pellet was resuspended in 6 m guanidine hydrochloride and 20 mm potassium phosphate (pH 2.3). Reaction tubes were spectrophotometrically read at a wavelength of 375 nm, using the blank tube as the reference. Total carbonyl content was calculated using the molar extinction coefficient of 22 000 m cm−1 and expressed as nmol carbonyl (mg protein)−1). The interassay coefficient of variance was 12%(n = 6).
To assess the localization of carbonyl groups after lengthening contractions, we performed immunohistochemistry procedures according to Smith et al. (1998). Briefly, muscle sections were fixed in acetone, treated with 0.2% H2O2, covered with 0.1% DNPH in 2 n HCl for 1 h, and blocked with 3% bovine albumin, 5% Tween 20 and 2% gelatin. Sections were rinsed with PBS between each of these steps. Control slides were not treated with H2O2 because of its potential to cause the formation carbonyl groups as a result of its application to the slide (Smith et al. 1998). Rabbit anti-DNP (1: 100 in PBS: Sigma) was then applied to each section and incubated for 16 h at 4°C. Slides serving as negative controls received PBS instead of primary antibody. Sections were then washed in PBS, incubated with biotinylated anti-rabbit IgG (1: 200 in PBS; Vector) followed by avidin D horseradish peroxidase (1: 1000 in PBS). Sections were then developed with 3-amino-9-ethylcarbazole (Vector). In general, the labelling appeared to be more specific when slides were not treated with H2O2.
Embryonic myosin heavy chain expression (eMHC)
The number of myofibres expressing eMHC was determined via immunohistochemistry and used as an additional marker of regeneration (Silberstein et al. 1986; Cho et al. 1994; Thaloor et al. 1999). Briefly, muscle sections were air dried, fixed with 2% formaldehyde, and blocked with 3% bovine albumin, 5% Tween 20 and 2% gelatin. Sections were washed with PBS and then incubated with a mouse antibody against human eMHC overnight at 4°C (clone F1.1652, 1: 2 in PBS; Developmental Studies Hybridoma Bank, University of Iowa, Iowa City, IA, USA). Slides serving as negative controls received PBS instead of primary antibody. To block detection of endogenous IgG, sections were treated with Fab fragment anti-mouse IgG (1: 70 in PBS; Jackson ImmunoResearch; West Groove, PA) and subsequently washed. Sections were then treated with biotinylated anti-mouse IgG (1: 200 in PBS; Vector) followed by avidin D horseradish peroxidase (1: 1000 in PBS). Sections were then developed with 3-amino-9-ethylcarbazole (Vector). The number of myofibres expressing eMHC were counted and expressed as a percentage of the total number of fibres within the section.
Protein content
Muscles were homogenized in reducing sample buffer (2% sodium dodecyl sulphate, 1.5% dithiothreitol, 1 m Tris-HCl and 10% glycerol) containing protease inhibitors (1 mm EDTA, 5 μg ml−1 leupeptin, 5 μg ml−1 aprotinin and 100 μg ml−1 phenylmethylsulphonyl fluoride). Homogenates were centrifuged, and the amount of protein in supernatants was determined via the filter paper dye-binding assay (Minamide & Bamburg, 1990) and expressed as μg mg−1 of EDL mass.
Statistical analyses
Dependent measures were analysed using two-way analysis of variance (SigmaStat; Sigma Chemical Corp., St Louis, MO, USA). Because changes in markers of injury resolution at 7 and 14 days post-lengthening contractions would probably be influenced by the magnitude of the injury at 3 days, we also statistically compared responses between groups of mice using an analysis of covariance. For this analysis, the isometric force deficit at 3 days of recovery, a measure of the totality of the injury (Faulkner & Brooks, 1994), was used as the covariate. The Newman-Keuls post hoc test was used to locate the differences between means when the observed F ratio was statistically significant (P < 0.05). Data are reported as mean and standard error (s.e.m.).
Results
Prior to lengthening contractions, body mass (26.2 ± 2.1 g, 26.6 ± 1.3 g), EDL mass (10.6 ± 0.2 mg, 10.2 ± 0.2 mg) and CSA of normal myofibres (1308 ± 129 μm, 1373 ± 126 μm) were not significantly different between wild type and CD18−/− mice, respectively. Baseline muscle function was also not influenced by the CD18 deficiency as indicated by a similar tetanic tension between wild type (375 ± 18 mN) and CD18−/− (385 ± 7 mN) mice. Consistent with their phenotype (Wilson et al. 1993), CD18−/− mice demonstrated an elevation in blood leucocytes (11.2 ± 0.3 × 106 ml−1) relative to wild type (6.5 ± 0.7 × 106 ml−1) mice prior to lengthening contractions.
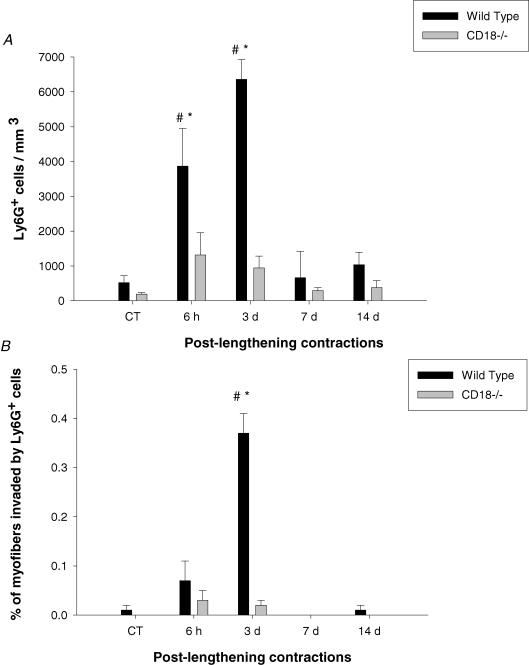
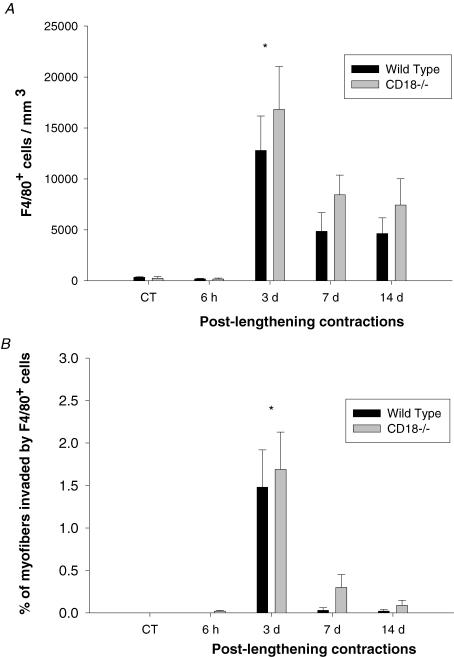
In support of our hypothesis that neutrophils enter skeletal muscle after contraction-induced muscle injury via a CD18-dependent mechanism, neutrophil concentrations were 4- and 7-fold higher in wild type relative to CD18−/− mice at 6 h and 3 days after lengthening contractions, respectively (Fig. 1A). In CD18−/− mice, neutrophils remained at control levels for 14 days after lengthening contractions. The percentage of myofibres that were invaded by neutrophils 3 days after lengthening contractions was 16-fold higher in wild type relative to CD18−/− mice (Fig. 1B). Macrophage concentrations and the percentage of myofibres invaded by macrophages at 3 days of recovery were not influenced by the CD18 deficiency (Fig. 2). Although differences between the groups of mice were not statistically significant (interaction P = 0.86, main effect for group P = 0.20), macrophages were ∼1.5-fold higher in CD18−/− relative to wild type mice at 3, 7 and 14 days after lengthening contractions. The macrophage data are in agreement with previous investigators who have reported that diapedesis of monocytes is largely dependent on a α4β1 integrin-dependent mechanism (Meerschaert & Furie, 1994; Issekutz, 1995; Meerschaert & Furie, 1995).
Figure 1.
A, neutrophil (Ly6G+ cells) concentrations, and B, percentage of fibres invaded by neutrophils after lengthening contractions. #Significantly higher for wild type relative to CD18−/− mice at the specified time point (interaction). *Significantly different from control levels (CT) for wild type mice only (time effect).
Figure 2.
A, macrophage (F4/80+ cells) concentrations, and B, percentage of fibres invaded by macrophages after lengthening contractions. *Significantly different from control levels (CT) for both wild type and CD18−/− mice (time effect).
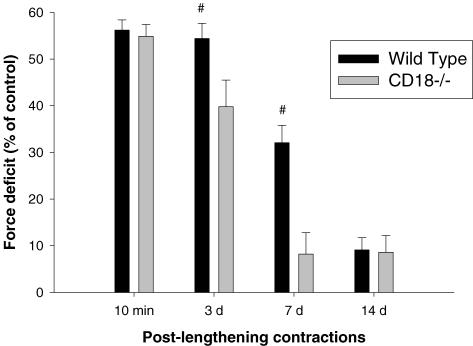
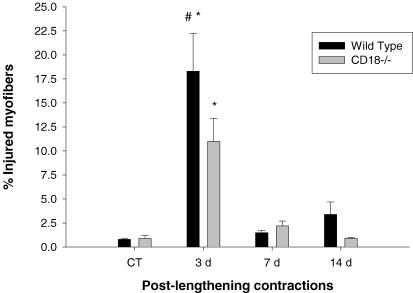
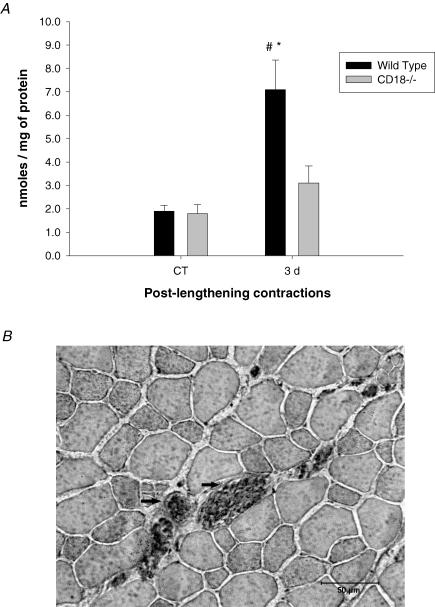
As expected, the force deficit 10 min after lengthening contractions was similar between wild type and CD18−/− mice (Fig. 3). Consistent with the hypothesis that neutrophils contribute to the injury, the isometric force deficit (Fig. 3), the per cent of injured fibres (Fig. 4), and total carbonyl content (Fig. 5A) were higher in wild type relative to CD18−/− mice 3 days after lengthening contractions. Immunohistochemistry revealed that carbonyl groups were found predominantly within myofibres of both CD18−/− and wild type (Fig. 5B) mice.
Figure 3. Force deficits.
Force deficits calculated relative to values obtained prior to lengthening contractions, during recovery from lengthening contractions. #Significantly higher for wild type relative to CD18−/− mice at the specified time point (interaction).
Figure 4. Percentage of injured myofibres.
#Significantly higher for wild type relative to CD18−/− mice at 3 days post-lengthening contractions (interaction). *Significantly different from control levels (CT) for both wild type and CD18−/− mice (time effect).
Figure 5.
A, total carbonyl content. #Significantly higher for wild type relative to CD18−/− mice at 3 days post-lengthening contractions (interaction). *Significantly different from control levels (CT) for wild type mice only (time effect). B, carbonyl groups were found predominantly in the sarcoplasm of myofibres (arrow) (magnification 400 ×).
Contrary to our hypothesis that neutrophils aid the resolution of contraction-induced muscle injury, the force deficit at 7 days post-lengthening contractions was higher in wild type relative to CD18−/− mice (Fig. 3). The lower deficit for CD18−/− mice at 7 days does not appear to be attributable to reduced injury because the initial injury (force deficit at 10 min) was similar between the CD18−/− and wild type mice. Furthermore, significant differences in the force deficit at 7 days were still apparent after statistically controlling for the lower deficit in CD18−/− mice at 3 days post-lengthening contractions. Histological abnormalities indicative of injury were resolved by 7 days for both CD18−/− and wild type mice (Fig. 4).
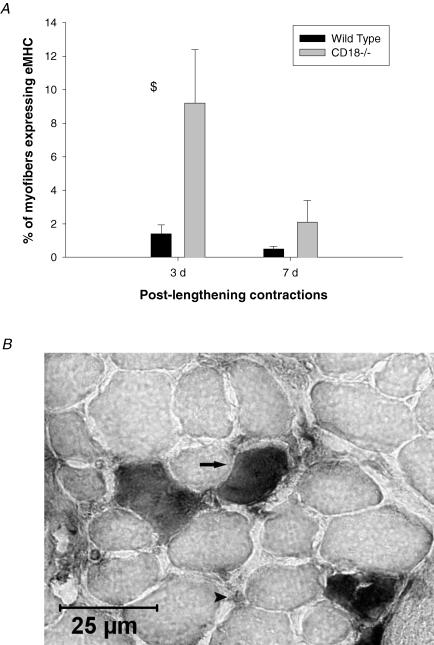
To further explore the role of neutrophils in the resolution of contraction-induced muscle injury, muscle sections were analysed for eMHC expression. Control muscles from both CD18−/− and wild type mice showed no labelling for eMHC. The percentages of myofibres expressing eMHC were significantly lower in wild type relative to CD18−/− mice at 3 and 7 days post-lengthening contractions (Fig. 6A). Differences were still apparent after statistically controlling for the lower injury at 3 days in CD18−/− mice. Very few myofibres from muscles obtained 14 days after lengthening contractions were positive for eMHC (data not reported). Most of the myofibres expressing eMHC in both CD18−/− and wild type mice at 3 days post-lengthening contractions were of normal size (Fig. 6B), some of which had morphological characteristics indicative of muscle injury. Although the observed expression of eMHC in normal sized myofibres at 3 days is difficult to interpret, other investigators have observed a similar phenomenon after contraction-induced muscle injury (Smith et al. 1999; Peters et al. 2003). Myofibres expressing eMHC at 7 days post-lengthening contractions tended to be smaller in size and angular in shape and, thus, exhibited characteristics of developing myotubes and/or immature myofibres.
Figure 6.
A, percentage of myofibres expressing eMHC. $Significantly higher for CD18−/− relative to wild type at 3 and 7 days post-lengthening contractions (group effect). B, localization of eMHC in a CD18−/− mouse 3 days after lengthening contractions. eMHC was found in normal sized myofibres (arrow), some of which had morphological characteristics of injury. Labelling was also found in apparent myotubes and/or immature myofibres (arrowhead) (magnification 600 ×).
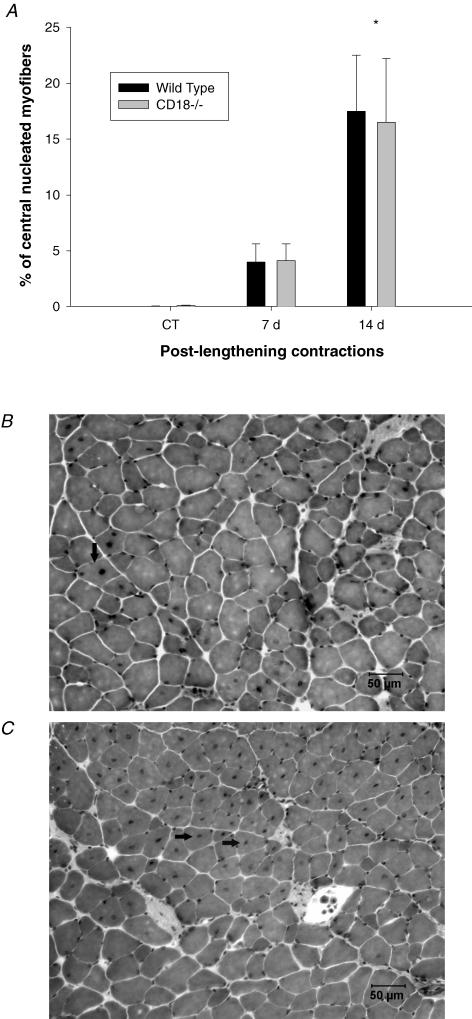
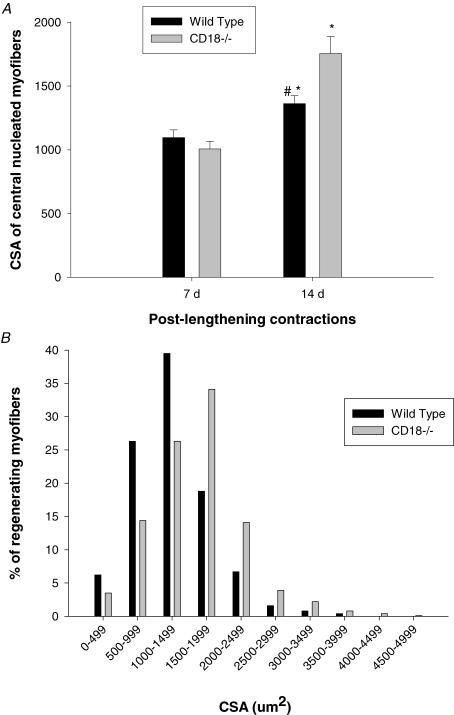
The percentage of central nucleated myofibres was not significantly different between CD18−/− and wild type mice at 7 and 14 days post-lengthening contractions even after statistically controlling for differences in the force deficit at 3 days (Fig. 7). Interestingly, the CSA of central nucleated myofibres in wild type mice was significantly smaller at 14 days post-lengthening contractions relative to CD18−/− mice (Fig. 8). When statistically controlling for muscle injury at 3 days, significant differences in CSA of central nucleated myofibres at 14 days were still apparent. The influence of the CD18 deficiency on CSA, however, was restricted to central nucleated myofibres because the CSA of normal myofibres was not different (P = 0.18) between CD18−/− (1691.2 ± 141.4 μm2) and wild type (1463.1 ± 62.9 μm2) mice at 14 days post-lengthening contractions. In CD18−/− mice at 14 days post-lengthening contractions, CSA of regenerating myofibres was similar to the CSA of normal myofibres. In contrast, CSA of regenerating myofibres of wild type mice at 14 days post-lengthening contractions was significantly smaller relative to the CSA of normal myofibres.
Figure 7.
A, percentage of central nucleated myofibres. *Significantly different from control levels (CT) for both wild type and CD18−/− mice (time effect). Cross sections of EDL muscles from wild type (B) and CD18−/− (C) collected 14 days after lengthening contractions that were stained with haematoxylin and eosin. Note the prevalence of central nucleated myofibres (arrows) (magnification 200 ×)).
Figure 8.
A, CSA of central nucleated myofibres. #Significantly higher for CD18−/− relative to wild type at 14 days post-lengthening contractions (interaction) *Significantly different from 7 days post-lengthening contractions for both wild type and CD18−/− mice (time effect). B, frequency distribution of the CSA of central nucleated myofibres.
Differences in CSA of central nucleated myofibres 14 days after lengthening contractions were not accompanied by differences in muscle protein content or EDL muscle mass. Specifically, protein content (μg mg−1 of EDL mass) was similar between CD18−/− (103.8 ± 5.6) and wild type (101.5 ± 5.2) mice at 14 days post-lengthening contractions whereas EDL muscle masses were at control levels in both CD18−/− (10.2 ± 0.5 mg) and wild type (10.3 ± 0.7 mg) mice at 14 days of recovery.
Discussion
The mechanisms for the entry of neutrophils into skeletal muscle after contraction-induced muscle injury and their functions within injured skeletal muscle are poorly understood. In the current study, we demonstrated that increased neutrophil concentrations in skeletal muscle after lengthening contractions are dependent on the β2 integrin, CD18. The absence of neutrophil accumulation in CD18−/− mice was associated with reductions in histological and functional signs of muscle injury and total carbonyl content 3 days after lengthening contractions. These data indicate that neutrophils may cause secondary muscle injury by oxidatively modifying skeletal muscle proteins after contraction-induced muscle injury. Interestingly, CD18−/− mice also had a lower force deficit at 7 days, a higher percentage of myofibres expressing eMHC, and a larger CSA of central nucleated myofibres at 14 days relative to wild type mice. These differences were still apparent after statistically controlling for the lower injury in CD18−/− mice. These preliminary observations indicate that neutrophils may also impair some of the events associated with the resolution of contraction-induced muscle injury.
The present study demonstrates for the first time that CD18 is critical for the accumulation of neutrophils in skeletal muscle injured by lengthening contractions. The absence of neutrophil accumulation in CD18−/− mice after lengthening contractions is consistent with the established role of CD18 in the diapedesis of neutrophils into a variety of injured and/or inflamed tissues including skeletal muscle. Specifically, previous investigators have reported that neutrophil accumulation in skeletal muscle after treatment with TNF-α or during the reperfusion of ischaemic muscle is dependent on CD18 (Palazzo et al. 1998; Zhang et al. 2000). Frenette et al. (2003) has recently reported P- and E-selectins, which cause rolling of neutrophils in post-capillary venules prior to the firm adhesion via CD18 (Kishimoto & Rothlein, 1994), are also required for the accumulation of neutrophils during mechanical loading of atrophic skeletal muscle. Thus it appears that the mechanism for the entry of neutrophils into skeletal muscle injured by increased muscle use is similar to the established protocol for their entry into other tissues after parenchymal cell injury (Kishimoto & Rothlein, 1994; Walzog & Gaehtgens, 2000).
Neutrophils are thought to contribute to the accumulation of macrophages in injured skeletal muscle by releasing cytokines (e.g. macrophage inflammatory protein-1 and monocyte chemoattractant protein-1) that cause monocyte chemotaxis. Macrophage concentrations, however, were similar between CD18−/− and wild type mice 3, 7 and 14 days after lengthening contractions. Whether differences in macrophage concentrations between CD18−/− and wild type mice occurred at other sampling time points (e.g. 1 and/or 2 days post-lengthening contractions) remains to be determined. The similarity in macrophage concentrations between CD18−/− and wild type mice after lengthening contraction may indicate that neutrophils do not contribute significantly to the accumulation of macrophages in skeletal muscle after contraction-induced muscle injury. Other cell types such as skeletal muscle cells (Chazaud et al. 2003) and endothelial cells (Krishnaswamy et al. 1999) may serve as the source of chemoattractants for monocytes after contraction-induced muscle injury.
Several mechanisms have been proposed to explain structural and functional abnormalities after lengthening contractions including mechanical factors, excitation-contraction coupling failure, ROS production and neutrophils (Faulkner & Brooks, 1994; Clarkson & Hubal, 2002; Warren et al. 2002). The similarity in the isometric force deficit 10 min after lengthening contractions is consistent with previous investigators who have concluded that the initial force deficit is attributable to mechanical forces generated during lengthening contractions and to excitation-coupling failure (Faulkner & Brooks, 1994; Warren et al. 2002). Reductions in the force deficit, percentage of injured myofibres and total carbonyl content in CD18−/− relative to wild type mice at 3 days post-lengthening contractions may indicate that neutrophils cause further injury by oxidatively modifying skeletal muscle proteins. Whether the increased carbonyl content in wild type mice was the result of a direct action of neutrophil-derived ROS or an indirect action such as neutrophil-derived TNF-α promoting oxidant production from other cell types (e.g. myofibres), remains to be determined.
The observation that CD18−/− mice are protected from contraction-induced muscle injury and oxidative damage in the present study are in agreement with Brickson et al. (2003) who reported that the administration of a blocking antibody for neutrophils reduced histological signs of muscle injury in rabbits 24 h after a single lengthening contraction. On the other hand, Lowe et al. (1995) reported that neutrophils do not cause muscle injury after lengthening contractions based on observations made after administering a blocking antibody for neutrophils. However, the blocking antibody did not reduce neutrophil accumulation in injured muscle, as measured by myeloperoxidase activity. In a broader context, our observations are also consistent with previous investigators who have established that neutrophils cause injury during the reperfusion of ischaemic skeletal muscle (Rubin et al. 1996; Palazzo et al. 1998) and with the recent work of Grounds et al. (Grounds & Torrisi, 2004) who reported that inflammatory cells exacerbate muscle pathology in mdx mice, a model of Duchenne muscular dystrophy.
The role of neutrophils in restoring normal structure and function to injured skeletal muscle is largely unknown. Based on their ability to remove injured tissue via phagocytosis (Papadimitriou et al. 1990; Edward, 1994) and to secrete cytokines (e.g. HGF and IL-6) (Cassatella, 1999) that could promote myogenesis (Austin & Burgess, 1991; Allen et al. 1995; Miller et al. 2000), we hypothesized that neutrophils contribute to the resolution of a contraction-induced muscle injury. Contrary to our hypothesis, CD18−/− mice had a lower force deficit at 7 days, a greater percentage of myofibres expressing eMHC, and a larger CSA of central nucleated myofibres at 14 days relative to wild type mice. Because the need for muscle regeneration/repair is probably dependent on the magnitude of injury, we also analysed these data via an analysis of covariance to statistically control for differences in muscle injury between CD18−/− and wild type mice (force deficit at 3 days served as the covariate). Results from this analysis suggest that differences in the force deficit at 7 days, eMHC expression and CSA of central nucleated myofibres at 14 days between CD18−/− and wild type mice were not attributable to the lower injury in CD18−/− mice. Interestingly, the percentage of central nucleated myofibres, muscle mass and protein content were similar between CD18−/− and wild type mice. As the numbers of central nucleated myofibres were a small fraction of the total number of myofibres (∼17%), the larger CSA of central nucleated myofibres in CD18−/− at 14 days of recovery may not have been of a sufficient magnitude to result in significant differences between CD18−/− and wild type mice in protein content of muscle homogenates. Taken together, these preliminary data indicate that neutrophils may delay some of the events associated with the resolution of contraction-induced muscle injury.
Several potential mechanisms exist for how neutrophils could impair the restoration of muscle structure and function after contraction-induced muscle injury. For example, neutrophils could delay the resolution of contraction-induced muscle injury by injuring myotubes as we have previously reported (Pizza et al. 2001; McLoughlin et al. 2003b). However, because central nucleated myofibres are presumed to be developing myotubes and/or immature myofibres (Anderson, 1991; Rosenblatt & Woods, 1992; Thaloor et al. 1999), the similarity in the percentage of central nucleated myofibres between wild type and CD18−/− may indicate that neutrophils do not influence the number of myotubes and/or immature myofibres after contraction-induced muscle injury. An alternative mechanism by which neutrophils could delay the resolution of the injury is via the release of cytokines (e.g. transforming growth factor-β1, TNF-α, IFN-γ, IL-1β and IL-12) (Cassatella, 1999) that have been reported to inhibit differentiation of cultured skeletal muscle cells and/or to promote skeletal muscle protein catabolism in vivo (Allen & Boxhorn, 1989; Kalovidouris et al. 1993; Hawke & Garry, 2001; Langen et al. 2001; Reid & Li, 2001).
In conclusion, we demonstrated that neutrophil accumulation after contraction-induced muscle injury is dependent on CD18. Furthermore, neutrophils appear to cause further muscle injury and impair some of the events associated with restoring structure and function to skeletal muscle after contraction-induced muscle injury. Further work is needed to confirm our preliminary observations that neutrophils impair the resolution of contraction-induced injury and to determine the mechanisms for the impairment. Once the mechanisms have been revealed, therapeutic and/or pharmacologic strategies could be developed to manipulate the inflammation biology of skeletal muscle to prevent any ill effects of neutrophils in injured skeletal muscle.
Acknowledgments
This project was funded through National Institute of Arthritis and Musculoskeletal and Skin Diseases grant (AR-47599; F.X.P.).
References
- Allen RE, Boxhorn LK. Regulation of skeletal muscle satellite cell proliferation and differentiation by transforming growth factor-beta, insulin-like growth factor I, and fibroblast growth factor. J Cell Physiol. 1989;138:311–315. doi: 10.1002/jcp.1041380213. [DOI] [PubMed] [Google Scholar]
- Allen RE, Sheehan SM, Taylor RG, Kendall TL, Rice GM. Hepatocyte growth factor activates quiescent skeletal muscle satellite cells in vitro. J Cell Physiol. 1995;165:307–312. doi: 10.1002/jcp.1041650211. [DOI] [PubMed] [Google Scholar]
- Anderson JE. Dystrophic changes in mdx muscle regenerating from denervation and devascularization. Muscle Nerve. 1991;14:268–279. doi: 10.1002/mus.880140311. 10.1002/mus.880140311. [DOI] [PubMed] [Google Scholar]
- Austin L, Burgess AW. Stimulation of myoblast proliferation in culture by leukaemia inhibitory factor and other cytokines. J Neurol Sci. 1991;101:193–197. doi: 10.1016/0022-510x(91)90045-9. 10.1016/0022-510X(91)90045-9. [DOI] [PubMed] [Google Scholar]
- Best TM, Fiebig R, Corr DT, Brickson S, Ji L. Free radical activity, antioxidant enzyme, and glutathione changes with muscle stretch injury in rabbits. J Appl Physiol. 1999;87:74–82. doi: 10.1152/jappl.1999.87.1.74. [DOI] [PubMed] [Google Scholar]
- Brickson S, Ji LL, Schell K, Olabisi R, St Pierre Schneider B, Best TM. M1/70 attenuates blood-borne neutrophil oxidants, activation, and myofiber damage following stretch injury. J Appl Physiol. 2003;95:969–976. doi: 10.1152/japplphysiol.00005.2003. [DOI] [PubMed] [Google Scholar]
- Cantini M, Giurisato E, Radu C, Tiozzo S, Pampinella F, Senigaglia D, Zaniolo G, Mazzoleni F, Vitiello L. Macrophage-secreted myogenic factors: a promising tool for greatly enhancing the proliferative capacity of myoblasts in vitro and in vivo. Neurol Sci. 2002;23:189–194. doi: 10.1007/s100720200060. [DOI] [PubMed] [Google Scholar]
- Cassatella MA. Neutrophil-Derived Proteins: Selling Cytokines by the Pound. Vol. 73. San Diego: Academic Press Inc; 1999. [DOI] [PubMed] [Google Scholar]
- Chazaud B, Sonnet C, Lafuste P, Bassez G, Rimaniol AC, Poron F, Authier FJ, Dreyfus PA, Gherardi RK. Satellite cells attract monocytes and use macrophages as a support to escape apoptosis and enhance muscle growth. J Cell Biol. 2003;163:1133–1143. doi: 10.1083/jcb.200212046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho M, Hughes SM, Karsch-Mizrachi I, Travis M, Leinwand LA, Blau HM. Fast myosin heavy chains expressed in secondary mammalian muscle fibers at the time of their inception. J Cell Sci. 1994;107:2361–2371. doi: 10.1242/jcs.107.9.2361. [DOI] [PubMed] [Google Scholar]
- Clarkson PM, Hubal MJ. Exercise-induced muscle damage in humans. Am J Phys Med Rehabil. 2002;81:S52–69. doi: 10.1097/00002060-200211001-00007. [DOI] [PubMed] [Google Scholar]
- Darr KC, Schultz E. Exercise-induced satellite cell activation in growing and mature skeletal muscle. J Appl Physiol. 1987;63:1816–1821. doi: 10.1152/jappl.1987.63.5.1816. [DOI] [PubMed] [Google Scholar]
- Edward SW. Biochemistry and Physiology of the Neutrophil. Cambridge: Cambridge University Press; 1994. [Google Scholar]
- Faulkner JA, Brooks S. An in situ single skeletal muscle model of contraction-induced injury: mechanics interpretations. BAM. 1994;4:17–23. [Google Scholar]
- Faulkner JA, Jones DA, Round JM. Injury to skeletal muscles of mice by forced lengthening during contractions. Q J Exp Physiol. 1989;74:661–670. doi: 10.1113/expphysiol.1989.sp003318. [DOI] [PubMed] [Google Scholar]
- Frenette J, Chbinou N, Godbout C, Marsolais D, Frenette PS. Macrophages, not neutrophils, infiltrate skeletal muscle in mice deficient in P/E selectins after mechanical reloading. Am J Physiol Regul Integr Comp Physiol. 2003;285:R727–732. doi: 10.1152/ajpregu.00175.2003. [DOI] [PubMed] [Google Scholar]
- Frenette J, St-Pierre M, Cote CH, Mylona E, Pizza FX. Muscle impairment occurs rapidly and precedes inflammatory cell accumulation after mechanical loading. Am J Physiol Regul Integr Comp Physiol. 2002;282:R351–357. doi: 10.1152/ajpregu.00189.2001. [DOI] [PubMed] [Google Scholar]
- Frost RA, Lang CH, Gelato MC. Transient exposure of human myoblasts to tumor necrosis factor-α inhibits serum and insulin-like growth factor-I stimulated protein synthesis. Endocrinology. 1997;138:4153–4159. doi: 10.1210/endo.138.10.5450. 10.1210/en.138.10.4153. [DOI] [PubMed] [Google Scholar]
- Grounds MD, Davies MJ. Chemotaxis in myogenesis. Basic Appl Myol. 1996;6:469–483. [Google Scholar]
- Grounds MD, Garrett KL, Lai MC, Wright WE, Beilharz MW. Identification of skeletal muscle precursor cells in vivo by use of MyoD1 and myogenin probes. Cell Tissue Res. 1992;267:99–104. doi: 10.1007/BF00318695. 10.1007/BF00318695. [DOI] [PubMed] [Google Scholar]
- Grounds MD, Torrisi J. Anti-TNFalpha (Remicade) therapy protects dystrophic skeletal muscle from necrosis. Faseb J. 2004;18:676–682. doi: 10.1096/fj.03-1024com. 10.1096/fj.03-1024com. [DOI] [PubMed] [Google Scholar]
- Hawke TJ, Garry DJ. Myogenic satellite cells: physiology to molecular biology. J Appl Physiol. 2001;91:534–551. doi: 10.1152/jappl.2001.91.2.534. [DOI] [PubMed] [Google Scholar]
- Issekutz TB. In vivo blood monocyte migration to acute inflammatory reactions, IL-1 alpha, TNF-alpha, IFN-gamma, and C5a utilizes LFA-1, Mac-1, and VLA-4. The relative importance of each integrin. J Immunol. 1995;154:6533–6540. [PubMed] [Google Scholar]
- Kalovidouris AE, Plotkin Z, Graesser D. Interferon-gamma inhibits proliferation, differentiation, and creatine kinase activity of cultured human muscle cells. II. A possible role in myositis. J Rheumatol. 1993;20:1718–1723. [PubMed] [Google Scholar]
- Kishimoto TK, Rothlein R. Integrins, ICAMs, and selectins: role and regulation of adhesion molecules in neutrophil recruitment to inflammatory sites. Adv Pharmacol. 1994;25:117–169. doi: 10.1016/s1054-3589(08)60431-7. [DOI] [PubMed] [Google Scholar]
- Koh TJ, Brooks SV. Lengthening contractions are not required to induce protection from contraction-induced muscle injury. Am J Physiol Regul Integr Comp Physiol. 2001;281:R155–161. doi: 10.1152/ajpregu.2001.281.1.R155. [DOI] [PubMed] [Google Scholar]
- Krishnaswamy G, Kelley J, Yerra L, Smith JK, Chi DS. Human endothelium as a source of multifunctional cytokines: molecular regulation and possible role in human disease. J Interferon Cytokine Res. 1999;19:91–104. doi: 10.1089/107999099314234. 10.1089/107999099314234. [DOI] [PubMed] [Google Scholar]
- Langen RC, Schols AM, Kelders MC, Van Der Velden JL, Wouters EF, Janssen-Heininger YM. Tumor necrosis factor-alpha inhibits myogenesis through redox dependent and -independent pathways. Am J Physiol Cell Physiol. 2002;283:C714–721. doi: 10.1152/ajpcell.00418.2001. [DOI] [PubMed] [Google Scholar]
- Langen RC, Schols AM, Kelders MC, Wouters EF, Janssen-Heininger YM. Inflammatory cytokines inhibit myogenic differentiation through activation of nuclear factor-kappaB. Faseb J. 2001;15:1169–1180. doi: 10.1096/fj.00-0463. 10.1096/fj.00-0463. [DOI] [PubMed] [Google Scholar]
- Lowe DA, Warren GL, Ingalls CP, Boorstein DB, Armstrong RB. Muscle function and protein metabolism after initiation of eccentric contraction-induced injury. J Appl Physiol. 1995;79:1260–1270. doi: 10.1152/jappl.1995.79.4.1260. [DOI] [PubMed] [Google Scholar]
- McCully KK, Faulkner JA. Injury to skeletal muscle fibers of mice following lengthening contractions. J Appl Physiol. 1985;59:119–126. doi: 10.1152/jappl.1985.59.1.119. [DOI] [PubMed] [Google Scholar]
- McLoughlin TJ, Mylona E, Hornberger TA, Esser KA, Pizza FX. Inflammatory cells in rat skeletal muscle are elevated after electrically stimulated contractions. J Appl Physiol. 2003a;94:876–882. doi: 10.1152/japplphysiol.00766.2002. [DOI] [PubMed] [Google Scholar]
- McLoughlin TJ, Tsivitse SK, Edwards JA, Aiken BA, Pizza FX. Deferoxamine reduces and nitric oxide synthase inhibition increases neutrophil-mediated myotube injury. Cell Tissue Res. 2003b;313:313–319. doi: 10.1007/s00441-003-0767-4. 10.1007/s00441-003-0767-4. [DOI] [PubMed] [Google Scholar]
- Meerschaert J, Furie MB. Monocytes use either CD11/CD18 or VLA-4 to migrate across human endothelium in vitro. J Immunol. 1994;152:1915–1926. [PubMed] [Google Scholar]
- Meerschaert J, Furie MB. The adhesion molecules used by monocytes for migration across endothelium include CD11a/CD18, CD11b/CD18, and VLA-4 on monocytes and ICAM-1, VCAM-1, and other ligands on endothelium. J Immunol. 1995;154:4099–4112. [PubMed] [Google Scholar]
- Merly F, Lescaudron L, Rouaud T, Crossin F, Gardahaut MF. Macrophages enhance muscle satellite cell proliferation and delay their differentiation. Muscle Nerve. 1999;22:724–732. doi: 10.1002/(sici)1097-4598(199906)22:6<724::aid-mus9>3.0.co;2-o. 10.1002/(SICI)1097-4598(199906)22:6<724::AID-MUS9>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Miller KJ, Thaloor D, Matteson S, Pavlath GK. Hepatocyte growth factor affects satellite cell activation and differentiation in regenerating skeletal muscle. Am J Physiol Cell Physiol. 2000;278:C174–181. doi: 10.1152/ajpcell.2000.278.1.C174. [DOI] [PubMed] [Google Scholar]
- Minamide LS, Bamburg JR. A filter paper dye-binding assay for quantitative determination of protein without interference from reducing agents or detergents. Anal Biochem. 1990;190:66–70. doi: 10.1016/0003-2697(90)90134-u. 10.1016/0003-2697(90)90134-U. [DOI] [PubMed] [Google Scholar]
- Muller WA. Leukocyte–endothelial–cell interactions in leukocyte transmigration and the inflammatory response. Trends Immunol. 2003;24:327–334. doi: 10.1016/s1471-4906(03)00117-0. [DOI] [PubMed] [Google Scholar]
- Newham DJ, McPhail G, Mills KR, Edwards RH. Ultrastructural changes after concentric and eccentric contractions of human muscle. J Neurol Sci. 1983;61:109–122. doi: 10.1016/0022-510x(83)90058-8. 10.1016/0022-510X(83)90058-8. [DOI] [PubMed] [Google Scholar]
- Orimo S, Hiyamuta E, Arahata K, Sugita H. Analysis of inflammatory cells and complement C3 in bupivacaine-induced myonecrosis. Muscle Nerve. 1991;14:515–520. doi: 10.1002/mus.880140605. 10.1002/mus.880140605. [DOI] [PubMed] [Google Scholar]
- Palazzo AJ, Jones SP, Girod WG, Anderson DC, Granger DN, Lefer DJ. Myocardial ischemia-reperfusion injury in CD18- and ICAM-1-deficient mice. Am J Physiol. 1998;275:H2300–2307. doi: 10.1152/ajpheart.1998.275.6.H2300. [DOI] [PubMed] [Google Scholar]
- Papadimitriou JM, Robertson TA, Mitchell CA, Grounds MD. The process of new plasmalemma formation in focally injured skeletal muscle fibers. J Struct Biol. 1990;103:124–134. doi: 10.1016/1047-8477(90)90016-6. 10.1016/1047-8477(90)90016-6. [DOI] [PubMed] [Google Scholar]
- Peters D, Barash IA, Burdi M, Yuan PS, Mathew L, Friden J, Lieber RL. Asynchronous functional, cellular and transcriptional changes after a bout of eccentric exercise in the rat. J Physiol. 2003;553:947–957. doi: 10.1113/jphysiol.2003.048462. 10.1113/jphysiol.2003.048462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizza FX, Koh TJ, McGregor SJ, Brooks SV. Muscle inflammatory cells after passive stretches, isometric contractions, and lengthening contractions. J Appl Physiol. 2002;92:1873–1878. doi: 10.1152/japplphysiol.01055.2001. 10.1063/1.1489068. [DOI] [PubMed] [Google Scholar]
- Pizza FX, McLoughlin TJ, McGregor SJ, Calomeni EP, Gunning WT. Neutrophils injure cultured skeletal myotubes. Am J Physiol Cell Physiol. 2001;281:C335–341. doi: 10.1152/ajpcell.2001.281.1.C335. [DOI] [PubMed] [Google Scholar]
- Reid MB, Li YP. Cytokines and oxidative signalling in skeletal muscle. Acta Physiol Scand. 2001;171:225–232. doi: 10.1046/j.1365-201x.2001.00824.x. 10.1046/j.1365-201x.2001.00824.x. [DOI] [PubMed] [Google Scholar]
- Reznick AZ, Packer L. Oxidative damage to proteins: spectrophotometric method for carbonyl assay. Meth Enzymol. 1994;233:357–363. doi: 10.1016/s0076-6879(94)33041-7. [DOI] [PubMed] [Google Scholar]
- Robertson TA, Papadimitriou JM, Grounds MD. Fusion of myogenic cells to the newly sealed region of damaged myofibres in skeletal muscle regeneration. Neuropathol Appl Neurobiol. 1993;19:350–358. doi: 10.1111/j.1365-2990.1993.tb00451.x. [DOI] [PubMed] [Google Scholar]
- Rosenblatt JD, Woods RI. Hypertrophy of rat extensor digitorum longus muscle injected with bupivacaine. A sequential histochemical, immunohistochemical, histological and morphometric study. J Anat. 1992;181:11–27. [PMC free article] [PubMed] [Google Scholar]
- Rubin BB, Romaschin A, Walker PM, Gute DC, Korthuis RJ. Mechanisms of postischemic injury in skeletal muscle: intervention strategies. J Appl Physiol. 1996;80:369–387. doi: 10.1152/jappl.1996.80.2.369. [DOI] [PubMed] [Google Scholar]
- Silberstein L, Webster SG, Travis M, Blau HM. Developmental progression of myosin gene expression in cultured muscle cells. Cell. 1986;46:1075–1081. doi: 10.1016/0092-8674(86)90707-5. [DOI] [PubMed] [Google Scholar]
- Sixt M, Hallmann R, Wendler O, Scharffetter-Kochanek K, Sorokin LM. Cell adhesion and migration properties of beta 2-integrin negative polymorphonuclear granulocytes on defined extracellular matrix molecules. Relevance for leukocyte extravasation. J Biol Chem. 2001;276:18878–18887. doi: 10.1074/jbc.M010898200. 10.1074/jbc.M010898200. [DOI] [PubMed] [Google Scholar]
- Smith HK, Plyley MJ, Rodgers CD, McKee NH. Expression of developmental myosin and morphological characteristics in adult rat skeletal muscle following exercise-induced injury. Eur J Appl Physiol Occup Physiol. 1999;80:84–91. doi: 10.1007/s004210050562. 10.1007/s004210050562. [DOI] [PubMed] [Google Scholar]
- Smith MA, Sayre LM, Anderson VE, Harris PL, Beal MF, Kowall N, Perry G. Cytochemical demonstration of oxidative damage in Alzheimer disease by immunochemical enhancement of the carbonyl reaction with 2,4-dinitrophenylhydrazine. J Histochem Cytochem. 1998;46:731–735. doi: 10.1177/002215549804600605. [DOI] [PubMed] [Google Scholar]
- Thaloor D, Miller KJ, Gephart J, Mitchell PO, Pavlath GK. Systemic administration of the NF-κB inhibitor curcumin stimulates muscle regeneration after traumatic injury. Am J Physiol. 1999;277:C320–329. doi: 10.1152/ajpcell.1999.277.2.C320. [DOI] [PubMed] [Google Scholar]
- Tidball JG, Berchenko E, Frenette J. Macrophage invasion does not contribute to muscle membrane injury during inflammation. J Leukoc Biol. 1999;65:492–498. [PubMed] [Google Scholar]
- Tsivitse SK, McLoughlin TJ, Peterson JM, Mylona E, McGregor SJ, Pizza FX. Downhill running in rats: influence on neutrophils, macrophages, and MyoD+ cells in skeletal muscle. Eur J Appl Physiol. 2003;90:633–638. doi: 10.1007/s00421-003-0909-0. 10.1007/s00421-003-0909-0. [DOI] [PubMed] [Google Scholar]
- Walzog B, Gaehtgens P. Adhesion molecules: the path to a new understanding of acute inflammation. News Physiol Sci. 2000;15:107–113. doi: 10.1152/physiologyonline.2000.15.3.107. [DOI] [PubMed] [Google Scholar]
- Warren GL, Ingalls CP, Lowe DA, Armstrong RB. What mechanisms contribute to the strength loss that occurs during and in the recovery from skeletal muscle injury? J Orthop Sports Phys Ther. 2002;32:58–64. doi: 10.2519/jospt.2002.32.2.58. [DOI] [PubMed] [Google Scholar]
- Wilson RW, Ballantyne CM, Smith CW, Montgomery C, Bradley A, O'Brien WE, Beaudet AL. Gene targeting yields a CD18-mutant mouse for study of inflammation. J Immunol. 1993;151:1571–1578. [PubMed] [Google Scholar]
- Zhang XW, Schramm R, Liu Q, Ekberg H, Jeppsson B, Thorlacius H. Important role of CD18 in TNF-α-induced leukocyte adhesion in muscle and skin venules in vivo. Inflamm Res. 2000;49:529–534. doi: 10.1007/s000110050627. 10.1007/s000110050627. [DOI] [PubMed] [Google Scholar]