Abstract
Increased release of thromboxane A2 (TXA2) has been shown to be involved in inflammatory bowel diseases. In the present study, we have investigated the effect of a stable TXA2 analogue (STA2) on the electrical parameters in isolated human colonic mucosa. In the human mucosa set between Ussing chambers, STA2 stimulated Cl− secretion in a concentration-dependent manner with an EC50 of 0.06 μm. The STA2-induced Cl− secretion was significantly inhibited by ONO-3708 (10 μm), a specific TXA2 receptor antagonist. The effect of STA2 (0.3 μm) was independent of the colonic segment from which the tissue was obtained, from caecum to rectum. Chromanol 293B, an inhibitor of the cAMP-dependent KvLQT1 channel, attenuated the STA2-induced Cl− secretion in the human colonic mucosa (IC50 value 1.18 μm). We found that KvLQT1 mRNA and protein were expressed in all the tested segments of the human colon. The STA2-induced Cl− secretion was significantly inhibited by 8-bromo-2′-monobutyryladenosine-3′,5′-cyclic monophosphorothioate (50 μm), a membrane-permeant cAMP antagonist. STA2 (0.3 μm) significantly increased the intracellular cAMP levels and the short-circuit current via TXA2 receptor in a human colonic cell line. These results suggest that the TXA2-induced Cl− secretion in the colon is mediated via the cAMP pathway in addition to the Ca2+–calmodulin pathway which was previously reported.
In an isolated rat distal colon, we found that thromboxane A2 (TXA2), a potent inducer of platelet aggregation and vasoconstriction (Coleman et al. 1994), is a novel secretagogue for Cl− secretion (Sakai et al. 1997). The anti-tumour drug irinotecan and platelet-activating factor (PAF) stimulate the release of the TXA2 from the subepithelial layer of rat colonic mucosa. Then the released TXA2 acts on the receptor of the epithelial crypt cells, resulting in the stimulation of Cl− secretion (Sakai et al. 1995, 1997, 2002b; Suzuki et al. 2000a, 2000c). These findings may explain the side-effect of irinotecan-induced diarrhoea. The stable TXA2 analogue 9,11-epithio-11,12-methano-thromboxane A2 (STA2) mimics the stimulatory effect of endogenous TXA2 in the rat colon (Sakai et al. 1997, 2002c; Suzuki et al. 2000a).
In colonic crypt cells, the apical Cl− conductance is due predominantly to the cystic fibrosis transmembrane conductance regulator (CFTR) (for review see Kunzelmann & Mall, 2002). Although the Ca2+-dependent Cl− channel (CaCC) as well as the CFTR contribute to Cl− secretion in the immortalized colonic cancer cell lines, the CaCC activity is absent in the apical membrane of the colonic crypt cells obtained from the native tissue (Kunzelmann & Mall, 2002). In the colonic cells, prostaglandin E2 (PGE2) activates Cl− secretion via the cAMP pathway, and acetylcholine via the Ca2+ pathway (McNamara et al. 1999). PGE2 increases intracellular cAMP levels via the EP2 receptor (Homaidan et al. 1995), and activates both the apical CFTR and the basolateral cAMP-dependent K+ channels (KvLQT1) (Kunzelmann et al. 2001). Acetylcholine elevates [Ca2+]i via M3 receptors (Lindqvist et al. 1998), and thus results in stimulation of the basolateral Ca2+-activated K+ channels which enhance the electrical driving force for the luminal Cl− exit (Nobles et al. 1991; Sandle et al. 1994; Strabel & Diener, 1995).
We have obtained complicated results concerning the TXA2-elicited pathway in the rat colon. STA2 elevates [Ca2+]i in rat colonic crypt cells (Ikari et al. 1999). However, the basolateral Ca2+-activated K+ channel was not stimulated (Suzuki et al. 2000b). The STA2-induced Cl− secretion was efficiently inhibited by the anti-diarrhoea drug loperamide, which may block the calmodulin system (Suzuki et al. 2000a). These results suggest that the STA2-elicited Ca2+ pathway is different from the carbachol-elicited Ca2+ pathway. On the other hand, STA2 depolarized the cells in the isolated crypt, suggesting the involvement of the cAMP pathway which triggers activation of the apical Cl− channels (Sakai et al. 1997). It has not been confirmed whether STA2 actually stimulates the cAMP production in the colonic cells. In relation to these findings, Hirata et al. (1996) reported that cloned TXA2 receptors, expressed in mammalian cultured cells, link to both adenylate cyclase and phospholipase C. The TXA2 receptors of platelets and glomerular mesangial cells are preferentially coupled to increase [Ca2+]i (for reviews see Coleman et al. 1994; Breyer & Breyer, 2000). However, the involvement of the cAMP pathway has not been elucidated.
So far, the effects of TXA2 on the Cl− secretion in the human colon have not been reported. In the present study, we examined the effect of STA2 in six different segments of human colonic mucosa derived from the caecum, ascending colon, transverse colon, descending colon, sigmoid colon and rectum. Then, we examined if the cAMP pathway is involved in the STA2-induced Cl− secretion in both the human and rat colon. We found that TXA2-induced Cl− secretion is mediated by the cAMP pathway. Some of these results have been presented to the Physiological Society (Horikawa et al. 2004; Sakai et al. 2004).
Methods
Chemicals
9,11-Epithio-11,12-methano-thromboxane A2 (STA2, ONO Pharmaceutical Co., Osaka, Japan), prostaglandin E2 (PGE2; Toray Industries, Tokyo, Japan), 7-(2α,4α-(dimethylmethano)-6β-(2-cyclopentyl-2β-hydroxyacetamido)-1α-cyclohexyl)5(Z)-heptenoic acid (ONO-3708; ONO Pharmaceutical Co.), sodium (E)-11-(2-(5,6-dimethyl-1-benzimidazolyl)ethylidene)-6,11-dihydrobenz[b,e]oxepine-2-caboxylate monohydrate (KW-3635, Kyowa Hakko Kogyo Co., Shizuoka, Japan) and chromanol 293B (Aventis Pharma Deutschland GmBH, Frankfurt, Germany) were generous gifts from the aforementioned companies. Furosemide, indomethacin, atropine monohydrate, 3-isobutyl-1-methylxanthine (IBMX) and tetrodotoxin were obtained from Wako Pure Chemical Industries (Osaka, Japan). 8-Bromo-2′-monobutyryladenosine-3′,5′-cyclic monophosphorothioate (Rp-8-Br-MB-cAMPS) and carbachol were from Sigma-Aldrich Co. (St Louis, MO, USA). Glibenclamide was from Research Biochemical International (Natick, MA, USA). STA2, PGE2, furosemide and indomethacin were dissolved in ethanol. KW-3635 and glibenclamide were dissolved in dimethyl sulphoxide. Ethanol and dimethyl sulphoxide concentrations in the final aqueous solutions never exceeded 0.5%.
Solutions
The Parsons solution for tissue preparation and Ussing chamber experiments contained (mm): 107 NaCl, 4.5 KCl, 25 NaHCO3, 1.8 Na2HPO4, 0.2 NaH2PO4, 1.25 CaCl2, 1 MgSO4 and 12 glucose. The solution was gassed with carbogen (5% CO2 in 95% O2) at a pH of 7.4. For the low-Cl− solution (7 mm Cl−), NaCl was replaced by sodium gluconate and supplemented with 4.5 mm CaSO4 in order to compensate for the Ca2+-buffering properties of gluconate.
Human tissue preparation
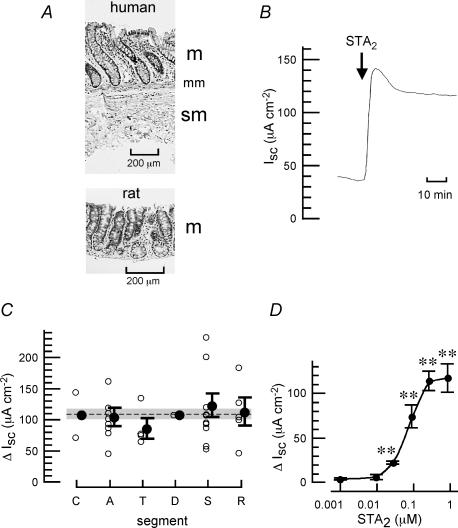
The specimens of human colorectal mucosa were obtained from surgical operations of 30 Japanese patients with colorectal adenocarcinomas (mean age, 66.1 ± 1.7 years; range, 51–82 years; 16 male and 14 female patients) in accordance with the recommendations of the Declaration of Helsinki and with ethics committee approval. Informed consents were obtained from all patients at Toyama Medical and Pharmaceutical University Hospital. In all cases, the specimens were collected at sites 5–10 cm from the carcinoma. The normal epithelial layer was isolated from the resected colon using scissors and forceps. Then, the blood vessels around the tissue were carefully removed. Part of these tissues was fixed in 10% formalin, then embedded in paraffin and cut into 4 μm thick sections to be deparaffinized in xylene and rehydrated with an alcohol gradient for usual haematoxylin and eosin staining. The tissue preparation was found to be free from the serosa and muscularis propria (Fig. 1A).
Figure 1. Increase in Isc induced by STA2, a stable TXA2 analogue, in isolated human colonic mucosa.
A, typical microscopic appearance of isolated human colonic mucosa (ascending colon) after removal of the serosa and muscularis propria (upper panel) and isolated rat colonic mucosa after removal of serosa, muscularis propria and submucosal layer (lower panel). m, mucosal layer; mm, muscularis mucosa; sm, submucosal layer. B, typical trace showing an increase in Isc induced by STA2 (0.3 μm at the serosal side). The mucosa was from human sigmoid colon. C, effect of STA2 on short-circuit current, Isc, in human colonic mucosa isolated from six different segments (C, caecum; A, ascending colon; T, transverse colon; D, descending colon; S, sigmoid colon; and R, rectum). The Isc values at the STA2 (0.3 μm)-elicited plateau phase were obtained and the results are expressed as the net increases from the control Isc measured just before the addition of STA2 (▵Isc). The values of ▵Isc from 30 patients are plotted (^). Each plot was obtained from 2 to 9 similar experiments of a patient. •, mean ± s.e.m. of the plots (^) in each segment. Dashed line with grey represents mean ± s.e.m. of all 30 plots. D, concentration-dependent effects of STA2 on Isc in the human colonic mucosa. Values are expressed as net increases from the baseline Isc before the addition of STA2 (▵Isc). n = 3–9, **P < 0.01.
Rat tissue preparation
The mucosal preparation of the distal part of the colon was obtained from female Wistar rats (140–200 g; Japan SLC, Shizuoka, Japan) in accordance with guidelines of the Animal Care and Use Committee of Toyama Medical and Pharmaceutical University. The animals had free access to water and food until the day of the experiment. Animals were killed rapidly by stunning and cervical dislocation. For the mucosal preparation, the serosa and muscularis propria were stripped away by hand. The submucosa was then carefully removed with forceps. The mucosal preparation was found to be free from serosa, muscularis propria and submucosa (Fig. 1A).
Ussing chamber experiments
The human or rat tissue was set between modified Ussing chambers and bathed with 4 ml of Parsons solution incubated at 37°C on either side of the mucosa. The exposed surface of the tissue measured 0.3 cm2. Short-circuit current (Isc) was measured continuously at a zero voltage difference with an amplifier (CEZ-9100, Nihon Kohden Co., Tokyo, Japan). The fluid resistance was compensated. The direction of Isc movement from the mucosal-to-serosal side is expressed as positive: that is, an increase in Cl− movement from the serosal-to-mucosal side (Cl− secretion) corresponded to an increase in Isc. The transepithelial potential difference (Pd) under open-circuit conditions was measured in the current-clamp mode of the amplifier. Tissue conductance (Gt) was determined from the deviation of Isc in response to the command voltage pulse of 0.5 mV (its duration was 100 ms).
Measurement of intracellular cAMP content ([cAMP]i) in the suspended colonic cells
Two human colonic cancer cell lines, HT-29 and WiDr, were used. The WiDr cell line was derived from a primary adenocarcinoma of the rectosigmoid colon from a 78-year-old female (Noguchi et al. 1979). HT-29 cells were obtained from Dainippon Pharmaceutical Co. (Osaka, Japan) and were maintained in McCoy's 5A medium supplemented with 10% fetal bovine serum (FBS). WiDr cells were obtained from the Japanese Cancer Research Resources Bank (Tokyo, Japan) and were maintained in MEM (Earle's) supplemented with non-essential amino acids and 10% FBS. These cultured cells were scraped by enzymatic digestion with trypsin (0.05%)–EDTA (0.53 mm) and were suspended in FBS-free medium (1 × 106 cells ml−1). The cell suspension (1 ml) was pre-treated with indomethacin (1 μm) and IBMX (1 mm) for 5 min at 34°C. STA2 (0.01–0.3 μm) or PGE2 (0.5 μm) was subsequently added to the suspension and incubated for 30 min at 34°C. The reaction was stopped by the addition of trichloroacetic acid (6%, w/v) and the mixture was frozen immediately in liquid nitrogen. The sample was thawed and centrifuged at 2000 g for 15 min at 4°C. The supernatant was then collected and washed four times with 2 ml of diethyl ether. Finally, it was freeze-dried for 18–20 h. The cAMP content of the preparation was determined with a cAMP enzyme immunoassay kit (Amersham Biosciences, Piscataway, NJ, USA).
The adherent human colonic cells on permeable supports
The HT-29 cells (1 × 106 cells per well) were seeded on 12-well polyester membrane transwell-clear inserts (Corning Incorporated, Corning, NY, USA). The membrane diameter and pore size were 12 mm and 0.4 μm, respectively. The cells were cultured for 24–48 h. Under the microscope, we found that the seeded cells in the well (1 × 106 cells) formed a confluent monolayer within 24–48 h. The monolayer of HT-29 cells on the permeable support was used for both the Ussing chamber experiment and the cAMP enzyme immunoassay. In the Ussing chamber experiment, the cell monolayer on the permeable support was set between the chambers and bathed with 4 ml of McCoy's 5A medium incubated at 37°C on either side of the mucosa, and Isc was measured as described above. In the cAMP enzyme immunoassay, the monolayer was pre-treated with indomethacin (1 μm at both the serosal and mucosal sides) and IBMX (1 mm at both the serosal and mucosal sides) for 10 min at 37°C in 5% CO2. STA2 (0.3 μm) or PGE2 (0.5 μm) was subsequently added to the serosal side of the monolayer and incubated for 30 min at 37°C in 5% CO2. When indicated, KW-3635 or ONO-3708 was added. For cell lysis, the monolayer was treated with 0.25% dodecyltrimethylammonium bromide (at the mucosal side) for 10 min at 25°C. The cAMP content of the extract was determined with the enzyme immunoassay kit (Amersham Biosciences).
RNA isolation and RT-PCR
Total RNAs of the isolated human colonic mucosa and human colonic cell lines were prepared using the RNAgents total RNA isolation system (Promega, Madison, WI, USA) or RNeasy midi kit (QIAGEN, Hilden, Germany). RT-PCR was carried out as described elsewhere (Sakai et al. 1999, 2001, 2003). Three sets of sense and antisense primers were used for PCR: (1) a set of primers based on the human TXA2 receptor sequence (nucleotide positions 46–68: 5′-CATGTCCAGGATGTCAGGGC-3′ and nucleotide positions 331–352: 5′-CATGTCCAGGATGTCAGGGC-3′); (2) a set of primers based on the human KvLQT1 sequence (nucleotide positions 816–840: 5′-CATGTCCAGGATGTCAGGGC-3′ and nucleotide positions 1391–1414: 5′-CATGTCCAGGATGTCAGGGC-3′); and (3) a set of primers based on the rat glyceraldehyde 3-phosphate dehydrogenase (GAPDH) sequence (nucleotide positions 443–461: 5′-CATGTCCAGGATGTCAGGGC-3′ and nucleotide positions 916–935: 5′-CATGTCCAGGATGTCAGGGC-3′). Forty cycles of PCR (95°C for 30 s, 58°C for 30 s, 68°C for 60 s) were performed.
Western blotting
Membrane fractions of the human colonic mucosa were prepared and Western blotting was carried out as described elsewhere (Sakai et al. 2002a). The blotting was performed with 80 μg of membrane protein. The anti-human KvLQT1 polyclonal antibody raised against a peptide mapping at the carboxyl terminus (C-20) of the KvLQT1 (Santa Cruz Biotechnology, Santa Cruz, CA, USA) was used at 1 : 300 dilution. The horseradish peroxidase-conjugated antigoat IgG was used as the secondary antibody (1: 2000 dilution).
Immunohistochemistry
Part of the human colonic tissues was fixed in PLP solution (2% paraformaldehyde, 75 mml-lysine, 10 mm sodium metaperiodate in phosphate-buffered saline), then embedded in Tissue-Tek O.C.T. compound (Sakura Finetechnical Co., Tokyo, Japan) and cut into 5 μm thick sections. Anti-human KvLQT1 polyclonal antibody (C-20; Santa Cruz Biotechnology) was used at 1 : 100 dilution. Rhodamine-conjugated anti-goat IgG (Chemicon International, Temecula, CA, USA) was used as the secondary antibody (1 : 100 dilution). The stained sample was observed by using a Zeiss LSM 510 confocal microscope (Carl Zeiss Co., Oberkochen, Germany).
Statistics
Results are presented as the mean ± s.e.m. Differences between groups were analysed by one-way ANOVA, and the correction for multiple comparisons was made by using Dunnett's multiple comparison test. When necessary, Tukey's multiple comparison test was used. Comparison between the two groups was made using Student's t test. Statistically significant differences were assumed at P < 0.05.
Results
Increase in Isc by a stable TXA2 analogue (STA2) in isolated human colonic mucosa
Human colonic mucosa was obtained from the caecum, ascending colon, transverse colon, descending colon, sigmoid colon or rectum of the patient. We examined the effect of STA2 on Isc across the colonic mucosa. Figure 1B shows that STA2 (0.3 μm at the serosal side) increased Isc in the mucosa of sigmoid colon with a plateau phase that was stable for at least 30 min. Similar effects of STA2 were observed in all colonic segments obtained from caecum to rectum and the magnitude of the STA2 (0.3 μm)-increased Isc (▵Isc) was not significantly dependent on the segment locations (Fig. 1C). No correlation between the size of the STA2 (0.3 μm)-induced increase in Isc and the level of baseline Isc prior to stimulation was observed (Fig. S1, in Supplementary material). STA2 increased Isc in a concentration-dependent manner with an EC50 of 0.06 μm (Fig. 1D). This EC50 value was close to the value obtained in the isolated rat colon (≥ 0.03 μm; Sakai et al. 1997). STA2 (0.3 μm) also significantly changed the values of Pd and Gt from 8.3 ± 0.9 to 13.0 ± 1.4 mV (P < 0.05) and 9.8 ± 0.4 to 14.0 ± 0.8 mS cm−2 (P < 0.01), respectively (n = 10).
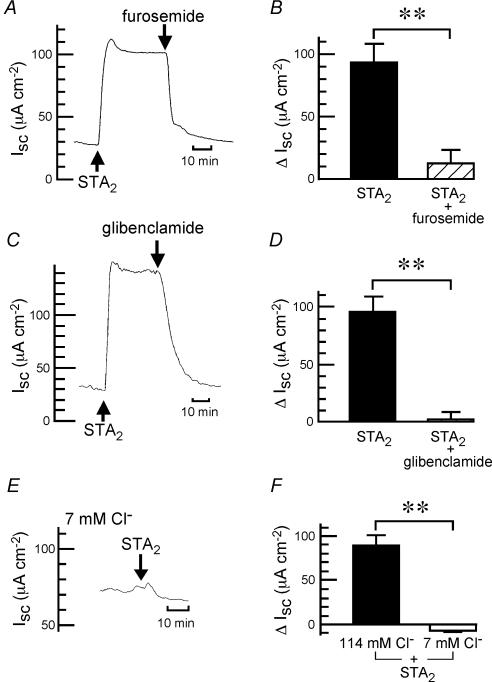
Ionic nature of the STA2-induced increase in Isc
In the human colonic mucosa, the STA2 (0.3 μm)-induced increase in Isc was significantly inhibited by furosemide (100 μm at the serosal side; Fig. 2A and B), an inhibitor of basolateral Na+–K+–2Cl− cotransporters (Chipperfield, 1986), and also by glibenclamide (500 μm at the mucosal side; Fig. 2C and D), a blocker of the apical Cl− channels in rat colon tissue (Strabel & Diener, 1995). Furthermore, the increase in Isc induced by STA2 was dependent on the presence of Cl− ions: that is, only a very small transient phase was caused by STA2 in the low-Cl− solution containing 7 mm Cl− (Fig. 2E and F). These results suggest that the STA2-induced response is caused by the secretion of Cl− ions.
Figure 2. STA2-induced Cl− secretion in isolated human colonic mucosa.
STA2 (0.3 μm) was added to the serosal side. Furosemide (100 μm at the serosal side) (A and B) or glibenclamide (500 μm at the mucosal side) (C and D) was added after the STA2-elicited plateau phase was observed. A and C, typical traces of Isc are shown. B and D, the STA2 (0.3 μm)-induced net increase in Isc was recorded just before the addition of furosemide (B) or glibenclamide (D) (filled columns). When the effect of the inhibitors reached a steady state, the Isc values were obtained, and they are expressed as ▵Isc (hatched columns). n = 4–5. **P < 0.01. E, a typical trace of Isc recorded in the low-chloride solution containing 7 mm Cl− is shown. STA2 (0.3 μm) was added as indicated. F, the STA2 (0.3 μm)-induced net increase in Isc was recorded in Parsons solution containing 114 mm Cl− (filled column) and in the low-chloride solution containing 7 mm Cl− (open column). n = 4. **P < 0.01.
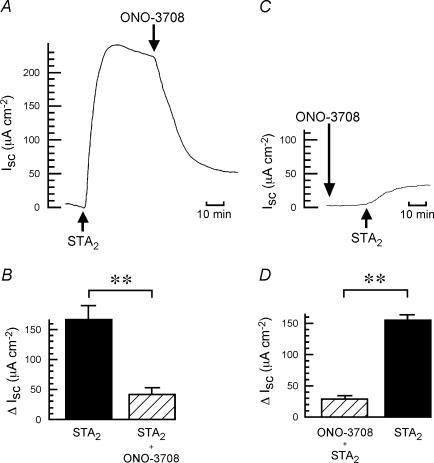
Inhibition of the STA2-induced Cl− secretion by a TXA2 receptor antagonist
We found previously that two specific TXA2 receptor antagonists, ONO-3708 and KW-3635, inhibited the Cl− secretion caused by endogenous TXA2 and exogenous STA2, while they had no inhibitory effects on the PGE2- and carbachol-induced secretion in the distal colon of the rat (Sakai et al. 1997, 2002c; Suzuki et al. 2000c). Figure 3 shows that the STA2 (0.3 μm)-induced increase in Isc was markedly inhibited by ONO-3708 (10 μm at the serosal side) in the human colon. Only a small component of the STA2-stimulated Isc was insensitive to ONO-3708 (10 μm), suggesting that STA2 may weakly bind to another receptor in addition to the TXA2 receptor. ONO-3708 (10 μm) had no effect on the baseline Isc. The values of Isc in the absence and presence of ONO-3708 were 17.9 ± 6.3 and 20.3 ± 5.7 μA cm−2, respectively (P > 0.05, n = 6).
Figure 3. Inhibitory effect of ONO-3708, a TXA2 receptor antagonist, on the STA2-induced increase in Isc.
STA2 (0.3 μm) was added to the serosal side. A, ONO-3708 (10 μm at the serosal side) was added after the STA2-elicited plateau phase was observed. A typical trace of Isc is shown. B, the STA2-induced net increase in Isc was recorded just before the addition of ONO-3708 (filled column). When the effect of the inhibitor reached a steady state, the Isc values were obtained, and they are expressed as ▵Isc (hatched column). n = 4. **P < 0.01. C, ONO-3708 (10 μm at the serosal side) was added before the addition of STA2. A typical trace of Isc is shown. D, the Isc values at the STA2-elicited plateau phase in the presence (hatched column) and absence (filled column) of ONO-3708 were obtained and the results are expressed as the net increases from the control Isc measured just before the addition of STA2 (▵Isc). n = 4. **P < 0.01.
Effect of a cAMP-dependent K+ channel blocker on the STA2- and PGE2-induced Cl− secretion in the human colonic mucosa
Kunzelmann et al. (2001) suggested that the KvLQT1 K+ channel, which is essential for the repolarization of the heart action potential, formed a component of the basolateral cAMP-activated K+ conductance in the colonic epithelium. KvLQT1 is blocked specifically by chromanol 293B (Bleich et al. 1997). Here, we examined if KvLQT1 is involved in the STA2-elicited mechanism in the human colon. The serosal addition of chromanol 293B inhibited the STA2 (0.3 μm)-increased Isc in a concentration-dependent manner (Fig. 4A and B) and its IC50 value was 1.18 μm. The PGE2 (0.5 μm)-increased Isc was also inhibited in a concentration-dependent manner by chromanol 293B (Fig. 4C), its IC50 value (1.22 μm) being close to that for the STA2-induced response (1.18 μm; Fig. 4B). To obtain the concentration–response curve (Fig. 4B and C), the effects of the time-dependent change with STA2 and PGE2 in the absence of chromanol 293B were taken into account, because Isc was not sufficiently stable over 2 h (Fig. S2, Supplementary material). As shown in Fig. 4D, chromanol 293B (10 μm) decreased the basal Isc by 10.5 ± 2.6 μA cm−2 (from 34.7 ± 5.6 to 24.2 ± 3.7 μA cm−2; n = 5). Therefore, the calculated values of IC50 may contain some errors. However, it should be noted that the size of the STA2 (0.3 μm)-increased Isc (118.8 ± 14.0 μA cm−2, n = 5) is much greater than that of the chromanol 293B-induced change of baseline Isc (10.5 ± 2.6 μA cm−2). If chromanol 293B (10 μm) was added prior to stimulation with STA2, the STA2-induced effect was almost completely inhibited (Fig. 4D and E). The specificity of chromanol 293B at high concentrations should be noted; 10 μm of 293B inhibited 30–40% of the CFTR current in Xenopus oocytes (Bachmann et al. 2001).
Figure 4. Inhibitory effect of chromanol 293B on the STA2- and PGE2-induced Cl− secretion in isolated human colonic mucosa.
In the plateau phase observed after the addition of STA2 (0.3 μm) or PGE2 (0.5 μm) in the presence of atropine (5 μm at the serosal side), chromanol 293B (0.01–10 μm at the serosal side) was added cumulatively as indicated (A–C). A, a typical trace is shown. STA2 and chromanol 293B were added as indicated. B, the concentration-dependent inhibitory effects of chromanol 293B on the STA2 (0.3 μm)-induced Cl− secretion. STA2-induced net increase in Isc was recorded when the effect of the inhibitor reached a steady state. Then the ▵Isc value was calibrated by using the time–response curve of STA2 (Fig. S2A, Supplementary material). Smaller values (%) of ▵Isc mean a greater degree of inhibition. The original value of ▵Isc measured just before the addition of chromanol 293B was 125.8 ± 12.1 μA cm−2 (n = 5). **P < 0.01, significantly different from the value in the absence of the inhibitor. C, the concentration-dependent inhibitory effects of chromanol 293B on the PGE2 (0.5 μm)-induced Cl− secretion. PGE2-induced net increase in Isc was recorded when the effect of the inhibitor reached a steady state. Then the ▵Isc value was calibrated by using the time–response curve of PGE2 (Fig. S2B, Supplementary material). The original value of ▵Isc measured just before the addition of chromanol 293B was 84.9 ± 11.7 μA cm−2 (n = 5). **P < 0.01, significantly different from the value in the absence of the inhibitor. D, chromanol 293B (10 μm at the serosal side) was added before the addition of STA2. A typical trace of Isc is shown. E, the Isc values at the STA2-elicited plateau phase in the absence (filled column) and the presence (hatched column) of chromanol 293B were obtained and the results expressed as the net increases from the control Isc measured just before the addition of STA2 (▵Isc). n = 4. **P < 0.01.
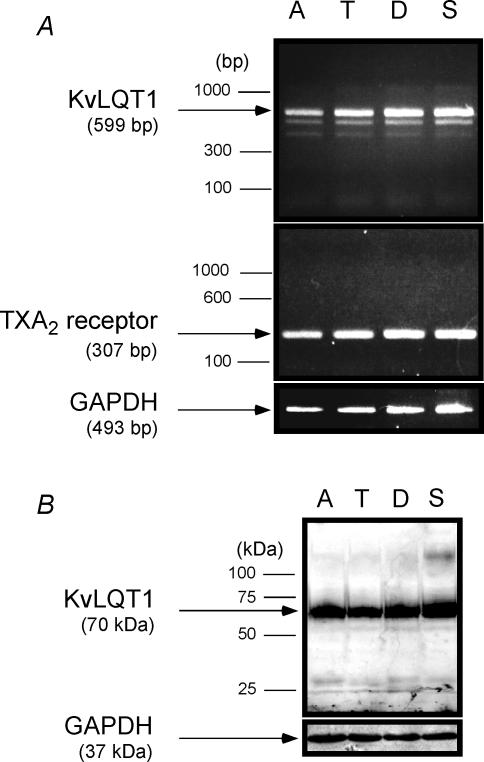
Expression of KvLQT1 in the human colonic mucosa
KvLQT1 mRNA (Fig. 5A) and protein (Fig. 5B) were confirmed as being expressed in all segments of human mucosa from ascending, transverse, descending and sigmoid colons, and no quantifiable difference in the amounts expressed was found. TXA2 receptor mRNA was also expressed in all segments without any quantifiable difference (Fig. 5A). These results may account for the reason why the STA2 response was observed in all segments along the human colon (Fig. 1C). The present immunohistochemical study showed that the KvLQT1 protein was mainly expressed in crypt cells, while no significant signal of KvLQT1 was observed in the muscularis mucosa, submucosal layer or mucosal interstitium of the tissue (Fig. S3, Supplementary material).
Figure 5. Expressions of TXA2 receptor and KvLQT1 in the human colonic mucosa.
A, gel analysis of RT-PCR products from human colonic mucosa isolated from ascending colon (A), transverse colon (T), descending colon (D) and sigmoid colon (S). Each specimen was derived from a different patient. A single band of 599 bp (KvLQT1; upper panel) and 307 bp (TXA2 receptor; middle panel) were detected by ethidium bromide staining. Amplification of GAPDH (493 bp) was used for control (lower panel). B, Western blotting for detecting the KvLQT1 protein. The blotting was performed with 80 μg of membrane protein from the same specimens as used in A. Expression of the KvLQT1 protein (70 kDa) is observed in all lanes (upper panel). As a control, expression of GAPDH protein (37 kDa) was examined (lower panel).
Effect of chromanol 293B on the STA2-, PGE2- and carbachol-induced Cl− secretion in the rat colonic mucosa
Similar to the results with human colon (Fig. 4A and B), the serosal addition of chromanol 293B inhibited the STA2 (1 μm)-increased Isc in a concentration-dependent manner in isolated rat colonic mucosa (Fig. S4A and B, Supplementary material), and its IC50 value was 0.39 μm. The PGE2-increased Isc was also inhibited in a concentration-dependent manner by chromanol 293B (Fig. S4C, Supplementary material), its IC50 value (0.36 μm) being close to that for the STA2-induced response. For estimating the IC50 values, the time control experiments with STA2 and PGE2 were performed (Fig. S5, Supplementary material). In contrast to the cases for STA2 and PGE2, chromanol 293B (1 μm) had no effect on the carbachol (50 μm)-induced increase in Isc (Fig. S6, Supplementary material), as reported previously (Greger et al. 1997).
Effect of IBMX, a phosphodiesterase inhibitor, on the STA2-induced Cl− secretion in the rat colonic mucosa
The STA2-induced Cl− secretion in isolated rat colonic mucosa was not inhibited by indomethacin, a cyclo-oxygenase (COX) inhibitor (1 μm at both the serosal and mucosal sides) plus tetrodotoxin (TTX), a neuronal inhibitor (1 μm at the serosal side), suggesting that the contribution of prostaglandins and neurotransmitters in the STA2-elicited pathway is negligibly small (Fig. S7A, B and D, Supplementary material). In the presence of indomethacin and TTX, the STA2-induced Cl− secretion was significantly stimulated by pre-treatment of the mucosa with IBMX (100 μm at both the serosal and mucosal sides), a phosphodiesterase inhibitor (Fig. S7C and D, Supplementary material). The results suggest that the STA2 response in the colonic mucosa may be mediated by the production of cAMP.
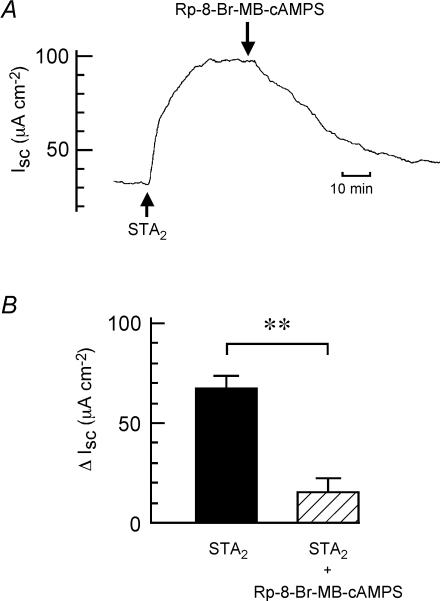
Effect of a competitive inhibitor of protein kinase A (cAMP antagonist) on the STA2-induced Cl− secretion in the human colonic mucosa
The STA2-induced Cl− secretion in isolated human colonic mucosa was significantly inhibited by Rp-8-Br-MB-cAMPS (50 μm at the serosal side), a membrane-permeant cAMP antagonist and a competitive inhibitor of protein kinase A (PKA) (Fig. 6). The results suggest that the cAMP–PKA pathway is involved in the STA2 response in the colonic mucosa.
Figure 6. Inhibitory effect of Rp-8-Br-MB-cAMPS, a membrane-permeant cAMP antagonist, on the STA2-induced increase in Isc.
STA2 (0.3 μm) was added to the serosal side. A, Rp-8-Br-MB-cAMPS (50 μm at the serosal side) was added after the STA2-elicited plateau phase was observed. A typical trace of Isc is shown. B, the STA2-induced net increase in Isc was recorded just before the addition of Rp-8-Br-MB-cAMPS (filled column). When the effect of the inhibitor reached a steady state, the Isc values were obtained and expressed as ▵Isc (hatched column). n = 4. **P < 0.01.
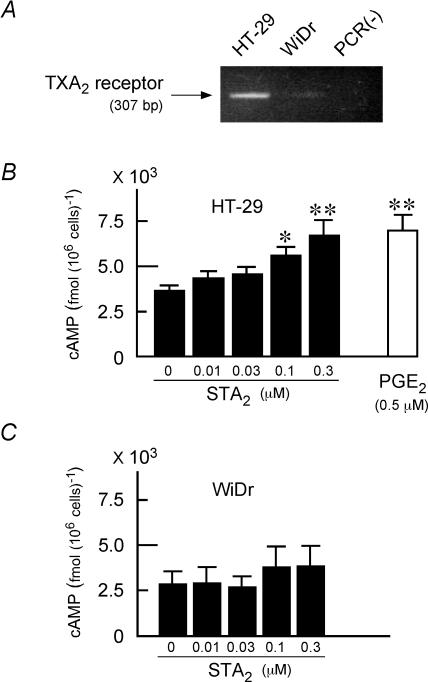
Increase in [cAMP]i by STA2 in human colonic cell lines
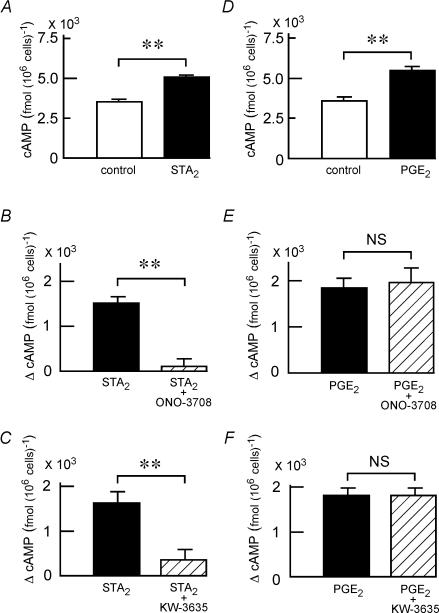
For measurement of cAMP levels in human colonic cells, we used two colonic cell lines (HT-29 and WiDr) in the present experiment. Figure 7A shows that mRNA for TXA2 receptor is highly expressed in the HT-29 cells, while it is not significantly expressed in the WiDr cells. In the suspended HT-29 cells, STA2 increased [cAMP]i in a concentration-dependent manner, and significant effects were observed at 0.1–0.3 μm (Fig. 7B). In the suspended WiDr cells, STA2 (0.01–0.3 μm) had no significant effect on [cAMP]i (Fig. 7C). The significant effect of STA2 (0.3 μm) was also observed in the adherent HT-29 cells cultured for 24–48 h on permeable supports (Fig. 8A). Two TXA2 receptor antagonists, ONO-3708 (10 μm; Fig. 8B) and KW-3635 (30 μm; Fig. 8C), significantly inhibited the STA2 (0.3 μm)-induced increase of [cAMP]i in the adherent HT-29 cells, while they had no significant effect on the PGE2 (0.5 μm)-induced increase of [cAMP]i in the cells (Fig. 8D–F). These results suggest that the STA2 response is mediated specifically via the TXA2 receptor.
Figure 7. Increase in [cAMP]i by STA2 in the suspended human colonic cells.
A, expression of TXA2 receptor mRNA in human colonic cell lines (the suspended cells of HT-29 and WiDr). Gel analysis of the RT-PCR products from HT-29 and WiDr cells. A single band of 307 bp was detected by ethidium bromide staining (HT-29 cells). No band was detected in a negative control experiment of HT-29 cells without reverse transcriptase (PCR(–)). B, the STA2-induced increase in [cAMP]i in the suspended HT-29 cells. [cAMP]i was measured as described in Methods. STA2 (0.01–0.3 μm) was used. As a positive control, PGE2 (0.5 μm) was used. n = 5. *P < 0.05 and **P < 0.01. C, no significant increase in [cAMP]i by STA2 (0.01–0.3 μm) was observed in the suspended WiDr cells.
Figure 8. Inhibition of the STA2-induced increase in [cAMP]i by TXA2 receptor antagonists in the adherent HT-29 cells.
A, the STA2-induced increase in [cAMP]i in the adherent HT-29 cells on permeable supports. STA2 (0.3 μm) was added to the serosal side (filled column). [cAMP]i was measured as described in Methods. n = 5. **P < 0.01. B, the effects of STA2 (0.3 μm; filled column) and STA2 (0.3 μm) plus ONO-3708 (10 μm) (hatched column) on [cAMP]i. Values are expressed as net increases from the baseline [cAMP]i (▵[cAMP]i) in the absence of STA2 and ONO-3708. n = 4. **P < 0.01. C, the effects of STA2 (0.3 μm; filled column) and STA2 (0.3 μm) plus KW-3635 (30 μm) (hatched column) on [cAMP]i. Values are expressed as ▵[cAMP]i. n = 4. **P < 0.01. D, the PGE2-induced increase in [cAMP]i in the adherent HT-29 cells on permeable supports. PGE2 (0.5 μm) was added to the serosal side (filled column). n = 5. **P < 0.01. E, the effects of PGE2 (0.5 μm; filled column) and PGE2 (0.5 μm) plus ONO-3708 (10 μm) (hatched column) on [cAMP]i. Values are expressed as ▵[cAMP]i. n = 4. NS, not significantly different (P > 0.05). F, the effects of PGE2 (0.5 μm; filled column) and PGE2 (0.5 μm) plus KW-3635 (30 μm) (hatched column) on [cAMP]i. Values are expressed as net ▵[cAMP]i. n = 4. NS, not significantly different (P > 0.05).
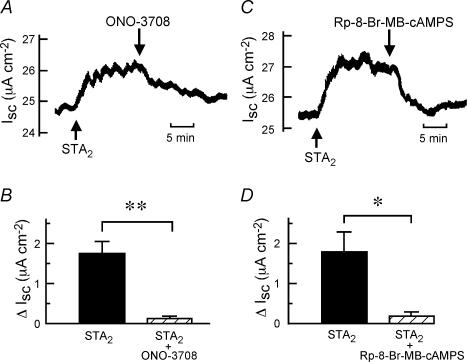
Increase in Isc by STA2 in the adherent human colonic cells on permeable supports
As expected from the results of Figs 7 and 8, STA2 (0.3 μm at the serosal side) increased Isc in the adherent HT-29 cell monolayer on permeable supports (Fig. 9). The transepithelial resistance of the layer set on the Ussing chamber was 41.02 ± 3.40 Ω cm2 (n = 5). Without the cells, the resistance of the permeable support itself was negligibly small (1.48 ± 0.03 Ω cm2, n = 5). Although the transepithelial resistance of the present preparation, cultured for 24–48 h, was smaller than that obtained with HT-29/B6 (Stockmann et al. 2000) or HT29 cL 19 A cells (Hiribarren et al. 1993), cultured for more than 7 days, we observed significant ion transport across the cell layer (Fig. 9). The STA2-induced effect was significantly inhibited by ONO-3708 (10 μm at the serosal side), a TXA2 receptor antagonist (Fig. 9A and B) and Rp-8-Br-MB-cAMPS (50 μm at the serosal side), a membrane-permeant cAMP antagonist (Fig. 9C and D).
Figure 9. Inhibitory effects of ONO-3708 and Rp-8-Br-MB-cAMPS on the STA2-induced increase in Isc in the adherent HT-29 cells.
STA2 (0.3 μm) was added to the serosal side. ONO-3708 (10 μm at the serosal side) (A and B) or Rp-8-Br-MB-cAMPS (50 μm at the serosal side) (C and D) was added after the STA2-elicited plateau phase was observed. A and C, typical traces of Isc are shown. B and D, the STA2 (0.3 μm)-induced net increase in Isc was recorded just before the addition of ONO-3708 (B) or Rp-8-Br-MB-cAMPS (D) (filled columns). When the effect of the inhibitors reached a steady state, the Isc values were obtained, and are expressed as ▵Isc (hatched columns). n = 3. *P < 0.05 and **P < 0.01.
Discussion
Here we have found that the stable TXA2 analogue STA2 induces Cl− secretion in isolated human colonic mucosa. The Cl− secretion was demonstrated by the following results: the sensitivity to furosemide, an inhibitor of the Na+–K+–2Cl− cotransporter; the sensitivity to the apical Cl− channel blocker glibenclamide; and the complete dependence of the response on the presence of Cl− (Fig. 2). In the present study, 500 μm glibenclamide was used because high concentrations of the drug (500 μm–1 mm) were required to block the forskolin-induced Cl− secretion in the rat colonic mucosa (Strabel & Diener, 1995). It should be noted that high concentrations of glibenclamide can inhibit several types of K+ channel such as ATP-sensitive K+ channels (Luzi & Pozza, 1997). The STA2 response was apparently mediated by the TXA2 receptor (Figs 3 and 5A), and was observed in all human colonic segments from caecum to rectum (Fig. 1C).
Cl− secretion in the mammalian colonic crypt cells required the coordination of: (1) opening of apical Cl− channels, (2) activation of basolateral Na+–K+–2Cl− cotransporters, (3) enhanced conductive K+ exit from the cells via basolateral K+ channels, and (4) increased pumping by Na+,K+-ATPase (Greger et al. 1997). In the cells, it has been suggested that apical Cl− channels are predominantly CFTR, which has a central role in colonic ion transport, and basolateral cAMP- and Ca2+-activated K+ channels are predominantly KvLQT1 and SK4, respectively (for review see Kunzelmann & Mall, 2002). The KvLQT1 (KCNQ1) potassium channel α-subunit interacts with the β-subunit KCNE3 in the colon (Schroeder et al. 2000; Dedek & Waldegger, 2001).
PGE2 did not increase [Ca2+]i in the cells in isolated rat colonic crypts (Ikari et al. 1999), which agrees with a report showing that the subtype of the prostaglandin E receptor in the crypt is EP2 which is linked with an adenylate cyclase–cAMP pathway (Homaidan et al. 1995). PGE2 activates basolateral cAMP-activated K+ channels with a unit conductance of < 3pS (Greger et al. 1997). In the human colon, inhibition of the basolateral K+ channels by chromanol 293B indicated the presence of KvLQT1 (Mall et al. 1998; Kunzelmann et al. 2001). Here, we have shown the presence of mRNA and the protein of KvLQT1 in human colon (Fig. 5). McNamara et al. (1999) reported involvement of basolateral K+ conductance, which is inhibited by Ba2+(IC50= 5.6 mm) and tetrapentylammonium (IC50= 5.1 μm), in cAMP-mediated Cl− secretion of isolated human colonic mucosa. We infer that this K+ conductance may be derived from KvLQT1 channels, based on the fact found later that the KvLQT1/KCNE3 expressed in Xenopus oocytes was inhibited by Ba2+ (IC50= 400 μm; Boucherot et al. 2001) and the KvLQT1 expressed in CHO cells was inhibited by tetrapentylammonium (IC50= 12.3 μm; Unsöld et al. 2000). The complete inhibition of PGE2-induced Cl− secretion by chromanol 293B (Fig. 4C and S4C) can be explained by the fact that PGE2 induces a marked depolarization of the crypt cells (Greger et al. 1997). This depolarization inhibits the basolateral Ca2+-activated K+ channels due to the depolarization-induced inhibition of Ca2+ influx into the cells (Greger et al. 1997; Schultheiß & Diener, 1997).
It has been suggested that the dominant effect of carbachol in intact rat colonic mucosa is an activation of basolateral Ca2+-activated K+ channels, leading to hyperpolarization of the crypt cells, and resulting in an increase in the driving force for the Cl− secretion if there are spontaneously open apical Cl− channels owing to sufficient basal production of cAMP (Strabel & Diener, 1995). There is no clear evidence that Ca2+ directly activates the apical Cl− channels in the colonic crypt cells of the native tissue (Strabel & Diener, 1995; Mall et al. 1998) and in the morphologically differentiated colonic cell line that expresses the epithelial Na+ channel (Currid et al. 2004). Chromanol 293B had no effect on basolateral Ca2+-activated K+ channels of the crypt cells (Greger et al. 1997), and cAMP-activated K+ channels have relatively little input during Ca2+-mediated stimulation of secretion (Kunzelmann & Mall, 2002). These results explain why the carbachol-stimulated Cl− secretion is not inhibited by chromanol 293B in the colonic mucosa (Fig. S6).
In the present study using human and rat colonic mucosa, we found that chromanol 293B inhibited the STA2-induced Cl− secretion and its IC50 value was very close to that for the PGE2-induced Cl− secretion (Fig. 4 and S4). The IC50 values for 293B inhibition of Isc were higher in human colon (∼1.2 μm; Fig. 4) than in rat colon (∼0.4 μm; Fig. S4), which agrees with the previous reports with human isolated colon (IC50≈ 5 μm; Mall et al. 1998) and with isolated rat colon (IC50≈ 0.1 μm; Diener et al. 1996). The STA2-induced Cl− secretion in human colonic mucosa was inhibited by a membrane-permeant cAMP antagonist (Fig. 6). These results suggest that the STA2 response is mediated by the cAMP–PKA pathway. In fact, the STA2 response was observed even in the presence of indomethacin and tetrodotoxin in the isolated rat mucosa (Fig. S7), and STA2 depolarized the cells in isolated rat colonic crypts (Sakai et al. 1997). STA2 stimulated the cAMP production (Figs 7 and 8) and increased Isc (Fig. 9) in the human colonic cell line. These effects were inhibited by TXA2 receptor antagonists (Figs 8 and 9).
Previously we found that STA2 elevates [Ca2+]i specifically via TXA2 receptors in rat colonic crypt cells (Ikari et al. 1999). In addition, the STA2-induced Cl− secretion in the rat colonic mucosa was inhibited completely by the anti-diarrhoea drug loperamide, which may block the calmodulin system (Suzuki et al. 2000a). In the mucosa, loperamide inhibited the STA2-induced secretion (IC50= 1.2 μm) more efficiently than the PGE2-induced secretion (IC50= 23 μm) (Suzuki et al. 2000a). These results suggest that the STA2 response was also mediated by the Ca2+–calmodulin pathway. In fact, cloned TXA2 receptors expressed in the cultured cells linked to both the adenylate cyclase and phospholipase C (Hirata et al. 1996). The STA2-elicited Ca2+ pathway may be distinct from the carbachol-elicited Ca2+ pathway because STA2 does not activate the basolateral Ca2+-activated K+ conductance in the rat colon (Suzuki et al. 2000b). It remains unclear why the STA2 response consists of a transient initial peak followed by a sustained plateau phase (Fig. 1B and S4A). It will be necessary to clarify whether STA2-induced Cl− secretion in human tissues reflects a synergistic interaction between cAMP- and Ca2+-pathways in a future study.
Our present finding that the TXA2 response in the colon is mediated by the cAMP pathway seems to be distinct from previous reports in platelets and glomerular mesangial cells. In these cells, the IP3-dependent Ca2+ mobilization and activation of protein kinase C were essential for the response (Coleman et al. 1994; Breyer & Breyer, 2000) and the physiological significance of the cAMP pathway remained unclear (Hirata et al. 1996).
Interestingly, the amount of endogenous TXA2, released from the colon under normal physiological conditions is minimal and it does not significantly contribute to the basal colonic Cl− secretion of rats (Sakai et al. 1997) and humans (Fig. 3C). In the rat colon, we found that TXA2 is released by the anti-tumour drug irinotecan, which causes severe diarrhoea as a side-effect, and by platelet-activating factor (PAF), which is closely associated with inflammatory bowel diseases (Sakai et al. 1997, 2002c; Suzuki et al. 2000c). Clinically, excess production of thromboxanes were observed in human ulcerative colitis, and oral administration of a thromboxane synthase inhibitor for the patients had been reported to be effective (Rampton & Collins, 1993; Casellas et al. 1995). Therefore TXA2 may act as a pathophysiological mediator in the colonic mucosa.
In summary, we found that the STA2 induces cAMP-mediated Cl− secretion in human and rat colonic mucosa and the response is mediated by a dual signalling mechanism in which the cAMP- and Ca2+-pathway are linked. The TXA2/STA2-cAMP pathway can be inhibited by at least two possible manoeuvres; one is through inhibition of cAMP-dependent K+ channel, KvLQT1, and another is through inhibition of the calmodulin system.
Acknowledgments
We thank Drs Judy G. Lee and Brandee A. Hara (University of Southern California, Los Angeles, USA) for their careful reading of this manuscript. This work was supported in part by Grants-in-Aid from the Japan Society for the Promotion of Science (to H.S. and N.T.) and the Ministry of Education, Culture, Sports, Science and Technology of Japan (to H.S. and N.T.).
Supplementary material
The online version of this paper can be accessed at: 10.1113/Jphysiol.2004.077776
http://jp.physoc.org/cgi/content/full/jphysiol.2004.077776/Dc1 and contains supplementary material consisting of seven figures.
This material can also be found at:
http://www.blackwellpublishing.com/products/journals/suppmat/tjp/tjp694/tjp694sm.htm
References
- Bachmann A, Quast U, Russ U. Chromanol 293B, a blocker of the slow delayed rectifier K+ current (Iks), inhibits the CFTR Cl− current. Naunyn-Schmiedeberg's Arch Pharmacol. 2001;363:590–596. doi: 10.1007/s002100100410. [DOI] [PubMed] [Google Scholar]
- Bleich M, Briel M, Busch AE, Lang HJ, Gerlach U, Gögelein H, Greger R, Kunzelmann K. KvLQT channels are inhibited by the K+ channel blocker 293B. Pflugers Arch. 1997;434:499–501. doi: 10.1007/s004240050427. [DOI] [PubMed] [Google Scholar]
- Boucherot A, Schreiber R, Kunzelmann K. Regulation and properties of KCNQ1 (KvLQT1) and impact of the cystic fibrosis transmembrane regulator. J Membr Biol. 2001;182:39–47. doi: 10.1007/s00232-001-0030-4. [DOI] [PubMed] [Google Scholar]
- Breyer MD, Breyer RM. Prostaglandin receptors: their role in regulating renal function. Curr Opin Nephrol Hypertens. 2000;9:23–29. doi: 10.1097/00041552-200001000-00005. [DOI] [PubMed] [Google Scholar]
- Casellas F, Papo M, Guarner F, Antolín M, Segura RM, Armengol JR, Malagelada J-R. Effects of thromboxane synthase inhibition on in vivo release of inflammatory mediators in chronic ulcerative colitis. Eur J Gastroenterol Hepatol. 1995;7:221–226. [PubMed] [Google Scholar]
- Chipperfield AR. The (Na+-K+-Cl−) co-transport system. Clin Sci. 1986;71:465–476. doi: 10.1042/cs0710465. [DOI] [PubMed] [Google Scholar]
- Coleman RA, Smith WL, Narumiya S. Classification of prostanoid receptors: properties, distribution, and structure of the receptors and their subtypes. Pharmacol Rev. 1994;46:205–229. [PubMed] [Google Scholar]
- Currid A, Ortega B, Valverde MA. Chloride secretion in a morphologically differentiated human colonic cell line that expresses the epithelial Na+ channel. J Physiol. 2004;555:241–250. doi: 10.1113/jphysiol.2003.059295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dedek K, Waldegger S. Colocalization of KCNQ1/KCNE channel subunits in the mouse gastrointestinal tract. Pflugers Arch. 2001;442:896–902. doi: 10.1007/s004240100609. 10.1007/s004240100609. [DOI] [PubMed] [Google Scholar]
- Diener M, Hug F, Strabel D, Scharrer E. Cyclic AMP-dependent regulation of K+ transport in the rat distal colon. Br J Pharmacol. 1996;118:1477–1487. doi: 10.1111/j.1476-5381.1996.tb15563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greger R, Bleich M, Riedemann N, van Driessche W, Ecke D, Warth R. The role of K+ channels in colonic Cl− secretion. Comp Biochem Physiol. 1997;118A:271–275. doi: 10.1016/s0300-9629(96)00304-0. 10.1016/S0300-9629(96)00304-0. [DOI] [PubMed] [Google Scholar]
- Hirata T, Ushikubi F, Kakizuka A, Okuma M, Narumiya S. Two thromboxane A2 receptor isoforms in human platelets. Opposite coupling to adenylyl cyclase with different sensitivity to Arg60 to Leu mutation. J Clin Invest. 1996;97:949–956. doi: 10.1172/JCI118518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiribarren A, Heyman M, L'Helgouac'h A, Desjeux JF. Effect of cytokines on the epithelial function of the human colon carcinoma cell line HT29 cl 19A. Gut. 1993;34:616–620. doi: 10.1136/gut.34.5.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homaidan FR, Zhao L, Burakoff R. Characterization of PGE2 receptors in isolated rabbit colonic crypt cells. Am J Physiol. 1995;268:G270–275. doi: 10.1152/ajpgi.1995.268.2.G270. [DOI] [PubMed] [Google Scholar]
- Horikawa N, Sakai H, Suzuki T, Tsukada K, Takeguchi N. Thromboxane-induced Cl− secretion in isolated human colorectum. J Physiol. 2004;555P:PC82. doi: 10.1113/jphysiol.2004.077776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikari A, Sakai H, Sato T, Takeguchi N. Thromboxane A2 receptor linked with the Ca2+ pathway in rat colonic crypt cells. Biochem Biophys Res Commun. 1999;258:708–712. doi: 10.1006/bbrc.1999.0674. 10.1006/bbrc.1999.0674. [DOI] [PubMed] [Google Scholar]
- Kunzelmann K, Bleich M, Warth R, Levy-Holzman R, Garty H, Schreiber R. Expression and function of colonic epithelial KvLQT1 K+ channels. Clin Exp Pharmacol Physiol. 2001;28:79–83. doi: 10.1046/j.1440-1681.2001.03407.x. 10.1046/j.1440-1681.2001.03407.x. [DOI] [PubMed] [Google Scholar]
- Kunzelmann K, Mall M. Electrolyte transport in the mammalian colon: mechanisms and implications for disease. Physiol Rev. 2002;82:245–289. doi: 10.1152/physrev.00026.2001. [DOI] [PubMed] [Google Scholar]
- Lindqvist SM, Sharp P, Johnson IT, Satoh Y, Williams MR. Acetylcholine-induced calcium signaling along the rat colonic crypt axis. Gastroenterology. 1998;115:1131–1143. doi: 10.1016/s0016-5085(98)70084-8. [DOI] [PubMed] [Google Scholar]
- Luzi L, Pozza G. Glibenclamide: an old drug with a novel mechanism of action? Acta Diabetol. 1997;34:239–244. doi: 10.1007/s005920050081. 10.1007/s005920050081. [DOI] [PubMed] [Google Scholar]
- McNamara B, Winter DC, Cuffe JE, O'Sullivan GC, Harvey BJ. Basolateral K+ channel involvement in forskolin-activated chloride secretion in human colon. J Physiol. 1999;519:251–260. doi: 10.1111/j.1469-7793.1999.0251o.x. 10.1111/j.1469-7793.1999.0251o.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mall M, Bleich M, Schürlein M, Kühr J, Seydewitz HH, Brandis M, Greger R, Kunzelmann K. Cholinergic ion secretion in human colon requires coactivation by cAMP. Am J Physiol. 1998;275:G1274–1281. doi: 10.1152/ajpgi.1998.275.6.G1274. [DOI] [PubMed] [Google Scholar]
- Nobles M, Diener M, Mestres P, Rummel W. Segmental heterogeneity of the rat colon in the response to activators of secretion on the cAMP-, the cGMP- and the Ca2+-pathway. Acta Physiol Scand. 1991;142:375–386. doi: 10.1111/j.1748-1716.1991.tb09171.x. [DOI] [PubMed] [Google Scholar]
- Noguchi P, Wallace R, Johnson J, Earley EM, O'Brien S, Ferrone S, Pellegrino MA, Milstien J, Needy C, Browne W, Petricciani J. Characterization of WiDr: a human colon carcinoma cell line. In Vitro. 1979;15:401–408. doi: 10.1007/BF02618407. [DOI] [PubMed] [Google Scholar]
- Rampton DS, Collins CE. Thromboxanes in inflammatory bowel diseases – pathogenic and therapeutic implications. Aliment Pharmacol Ther. 1993;7:357–367. [PubMed] [Google Scholar]
- Sakai H, Diener M, Gartmann V, Takeguchi N. Eicosanoid-mediated Cl− secretion induced by the antitumor drug, irinotecan (CPT-11), in the rat colon. Naunyn Schmiedebergs Arch Pharmacol. 1995;351:309–314. doi: 10.1007/BF00233252. [DOI] [PubMed] [Google Scholar]
- Sakai H, Lingueglia E, Champigny G, Mattei M-G, Lazdunski M. Cloning and functional expression of a novel degenerin-like Na+ channel gene in mammals. J Physiol. 1999;519:323–333. doi: 10.1111/j.1469-7793.1999.0323m.x. 10.1111/j.1469-7793.1999.0323m.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai H, Ohira Y, Tanaka A, Suzuki T, Ikari A, Morii M, Takeguchi N. Inhibition of small-conductance Cl− channels by the interleukin-1β-stimulated production of superoxide in rabbit gastric parietal cells? J Physiol. 2003;551:207–217. doi: 10.1113/jphysiol.2003.041921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai H, Sato T, Hamada N, Yasue M, Ikari A, Kakinoki B, Takeguchi N. Thromboxane A2, released by the anti-tumour drug irinotecan, is a novel stimulator of Cl− secretion in isolated rat colon. J Physiol. 1997;505:133–144. doi: 10.1111/j.1469-7793.1997.133bc.x. 10.1111/j.1469-7793.1997.133bc.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai H, Shimizu T, Hori K, Ikari A, Asano S, Takeguchi N. Molecular and pharmacological properties of inwardly rectifying K+ channels of human lung cancer cells. Eur J Pharmacol. 2002a;435:125–133. doi: 10.1016/s0014-2999(01)01567-9. 10.1016/S0014-2999(01)01567-9. [DOI] [PubMed] [Google Scholar]
- Sakai H, Suzuki T, Murota M, Oketani K, Uchiumi T, Murakami M, Takeguchi N. E3040 sulphate, a novel thromboxane synthase inhibitor, blocks the Cl− secretion induced by platelet-activating factor in isolated rat colon. Br J Pharmacol. 2002b;136:383–390. doi: 10.1038/sj.bjp.0704723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai H, Suzuki T, Murota M, Takahashi Y, Takeguchi N. Nitric oxide-induced Cl− secretion in isolated rat colon is mediated by the release of thromboxane A2. J Physiol. 2002c;543:261–271. doi: 10.1113/jphysiol.2002.021287. 10.1113/jphysiol.2002.021287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai H, Uchiumi T, Suzuki T, Takeguchi N. Cyclic AMP-dependent Cl− secretion induced by thromboxane A2 in isolated rat colonic mucosa. J Physiol. 2004;555P:C142. doi: 10.1113/jphysiol.2004.077776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai H, Ukai M, Ikari A, Asano S, Takeguchi N. Is rabbit CLCA1 related to the basolateral Ca2+-dependent Cl− channel of gastric parietal cells? Jpn J Physiol. 2001;51:121–125. doi: 10.2170/jjphysiol.51.121. [DOI] [PubMed] [Google Scholar]
- Sandle GI, McNicholas CM, Lomax RB. Potassium channels in colonic crypts. Lancet. 1994;343:23–25. doi: 10.1016/s0140-6736(94)90878-8. 10.1016/S0140-6736(94)90878-8. [DOI] [PubMed] [Google Scholar]
- Schroeder BC, Waldegger S, Fehr S, Bleich M, Warth R, Greger R, Jentsch TJ. A constitutively open potassium channel formed by KCNQ1 and KCNE3. Nature. 2000;403:196–199. doi: 10.1038/35003200. 10.1038/35003200. [DOI] [PubMed] [Google Scholar]
- Schultheiß G, Diener M. Regulation of apical and basolateral K+ conductances in the rat colon. Br J Pharmacol. 1997;122:87–94. doi: 10.1038/sj.bjp.0701353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockmann M, Schmitz H, Fromm M, Schmidt W, Pauli G, Scholz P, Riecken E-O, Schulzke J-D. Mechanisms of epithelial barrier impairment in HIV infection. Ann N Y Acad Sci. 2000;915:293–303. doi: 10.1111/j.1749-6632.2000.tb05257.x. [DOI] [PubMed] [Google Scholar]
- Strabel D, Diener M. Evidence against direct activation of chloride secretion by carbachol in the rat distal colon. Eur J Pharmacol. 1995;274:181–191. doi: 10.1016/0014-2999(94)00728-p. [DOI] [PubMed] [Google Scholar]
- Suzuki T, Sakai H, Ikari A, Takeguchi N. Inhibition of thromboxane A2-induced Cl− secretion by antidiarrhea drug loperamide in isolated rat colon. J Pharmacol Exp Ther. 2000a;295:233–238. [PubMed] [Google Scholar]
- Suzuki T, Sakai H, Ikari A, Takeguchi N. Mobilization of intracellular Ca2+ by thromboxane A2 does not affect Ca2+-activated K+ channels in rat colonic crypt cells. Jpn J Physiol. 2000b;50:389–393. doi: 10.2170/jjphysiol.50.389. [DOI] [PubMed] [Google Scholar]
- Suzuki T, Sakai H, Takeguchi N. Thromboxane A2-mediated Cl− secretion induced by platelet-activating factor in isolated rat colon. Eur J Pharmacol. 2000c;400:297–303. doi: 10.1016/s0014-2999(00)00405-2. [DOI] [PubMed] [Google Scholar]
- Unsöld B, Kerst G, Brousos H, Hübner M, Schreiber R, Nitschke R, Greger R, Bleich M. KCNE1 reverses the response of the human K+ channel KCNQ1 to cytosolic pH changes and alters its pharmacology and sensitivity to temperature. Pflugers Arch. 2000;441:368–378. doi: 10.1007/s004240000434. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.