Abstract
Bacillus anthrax lethal toxin can be engineered to deliver foreign proteins to the cytosol for antigen presentation to CD8 T cells. Vaccination with modified toxins carrying 8–9 amino acid peptide epitopes induces protective immunity in mice. To evaluate whether large protein antigens can be used with this system, recombinant constructs encoding several HIV antigens up to 500 amino acids were produced. These candidate HIV vaccines are safe in animals and induce CD8 T cells in mice. Constructs encoding gag p24 and nef stimulate gag-specific CD4 proliferation and a secondary cytotoxic T lymphocyte response in HIV-infected donor peripheral blood mononuclear cells in vitro. These results lay the foundation for future clinical vaccine studies.
Growing evidence suggests that cell-mediated immunity (CMI) plays an essential role in controlling HIV infection (1–3). Exposed but uninfected individuals often have antiviral CMI but no antibody response. The viremia of primary infection resolves coincident with the development of viral specific cytotoxic T lymphocytes (CTL), before the development of specific antibodies. These data suggest that induction of anti-HIV CMI may be an essential component of an effective AIDS vaccine (4).
Eliciting effective T cell responses with a vaccine is a challenge, both theoretically and practically. Although subunit vaccines can prime antigen-presenting cells for presentation and activation of CD4 T cell responses, they do not efficiently induce CD8 T cell responses. Because CD8 T cell priming requires antigen delivery to the cytosol of host cells for processing into the MHC class I pathway (5), the obstacle is to deliver recombinant protein antigens into the cytosol. Live vectors or naked DNA can do this, although there are safety concerns associated with these approaches. Furthermore, early clinical efforts with DNA vaccination and poxvirus vector vaccines have not produced convincing evidence that strong HIV-specific CTL responses are induced. For protein-based vaccines, efforts in the past have focused on excipients, such as immune adjuvants, or packaging the antigen into delivery vehicles, such as liposomes. This report describes a different approach to making a T cell-dependent HIV vaccine, using the natural ability of Bacillus anthracis to insert its toxin into the cytosolic compartment of mammalian cells. The engineered anthrax toxin vaccine appears unlikely to induce an antibody response at the low concentrations of protein used to optimize the T cell response. Therefore, a successful vaccine strategy for HIV will likely need to combine it with a vaccine designed to raise neutralizing antibodies.
B. anthracis is the causative agent of anthrax in animals and humans. The toxin produced by B. anthracis consists of two bipartite protein exotoxins, lethal toxin (LT) and edema toxin. LT is composed of protective antigen (PA) and lethal factor (LF), whereas edema toxin consists of PA and edema factor (EF). None of these three components, PA, LF, and EF, alone is toxic. Once combined, however, edema toxin causes edema and LT causes death by systemic shock in animals and humans. Consistent with its critical role in forming both toxins, PA has been identified as the protective component in vaccines against anthrax. The molecular mechanism of anthrax toxin action is currently hypothesized as follows: PA is a 735-amino acid (aa) polypeptide that binds to the surface of mammalian cells by cellular receptors. Once bound, PA is activated by proteolytic cleavage by cellular proteases to a 63-kDa molecule capable of forming a ring-shaped heptamer in the plasma membrane of the targeted cell (6, 7). The PA heptamer then binds either EF or LF, which are internalized by endocytosis. After endosomal acidification, PA enables EF or LF to enter the cytosol, presumably by means of a pore formed by the heptamer. Within the cytosol, EF acts as an adenylate cyclase (8) to convert ATP to cAMP. Abnormally elevated levels of cAMP perturb cellular metabolism. The action of LF in the cytosol causes the death of host cells by a mechanism that is not well understood. LF induces overproduction of a number of lymphokines (9), contributing to lethal systemic shock in host animals. Recent studies also show that LF has two enzymatic activities: it can act as a zinc metalloprotease (10), and it inactivates the mitogen-activated protein kinase (11). Although it is still not clear how these two enzymatic activities of LF are connected, both are required for LF toxicity. LF is a 796-aa polypeptide, and the functional domain for both enzymatic activities is located between amino acids 383 and 796 (12). The N-terminal truncated LF without this catalytic domain completely lacks any toxic effect when mixed with PA and added to cultured macrophages or when injected into animals. It does, however, still bind to PA effectively. The PA binding domain of LF (LFn) consists of amino acids 1–255. (12).
The combination of PA plus LFn fused to a foreign peptide can be used as a “molecular syringe” to introduce foreign proteins into the cytosol for antigen presentation to CD8 T cells. Previous studies have demonstrated successful CTL induction in inbred mice after administration of PA plus LFn carrying 8- to 9-aa peptide epitope. For example, immunization of BALB/c mice with PA plus LFn-LLO, a fusion protein of LFn with a CTL epitope from the listeriolysin protein of Listeria monocytogenes, stimulated a significant CTL response. This response protected animals challenged with L. monocytogenes. Immunized mice showed a significant reduction of colony-forming units in the spleen and liver compared with untreated mice (13). Similarly, immunization with PA plus LFn fused to a lymphocytic choriomeningitis virus (LCMV) nucleoprotein epitope protects against lethal LCMV infection. Another study demonstrated CTL induction in C57BL/6 mice by PA plus an LFn fusion protein carrying a CTL epitope from ovalbumin (LFn-OVA) (14).
Although “universal” epitopes recognized by CD4 T cells from most members of an MHC-diverse population are not uncommon, no such CD8 T cell epitopes have ever been identified. The immunodominant epitopes recognized by HIV-specific CTL are quite varied from individual to individual. Therefore, an ideal T cell-dependent vaccine should be able to present larger protein antigens encompassing many potential epitopes. The initial goal of this study was to determine whether the LFn/PA system could be used to deliver large protein antigens to the host cytosol for class I presentation. In a previous study, fusion of LFn with HIV-1 gp120 was able to present a variable region 3 (V3) epitope in vitro by means of the MHC class I antigen presentation pathway in a PA-dependent fashion (15). However, this construct has not been shown to elicit a CTL response in vivo. Here, we report the production of stable and soluble recombinant fusion proteins between LFn and a variety of HIV antigens up to 500 aa in length. We demonstrate that immunization with these HIV candidate vaccines is safe in mice and rabbits and can elicit CD8 T cell responses in mice. The proteins also stimulate human PBMC in an in vitro activation protocol. These results lay the foundation to advance this approach from laboratory experiments to clinical testing.
Materials and Methods
Molecular Construction and Expression of LFn Fusion Proteins.
The DNA fragment encoding the V3 region and gag p24 from HIV-HXB were amplified by PCR, cloned into the LFn expression plasmid pET15bLFn, and sequenced to verify the inframe fusion between the LFn and the HIV coding sequence. The nef coding sequence was amplified from HIV-ELI. The protein expression vector for LFn and its fusion derivatives is the pET15b plasmid (Novagen). The main features of this vector system include an inducible T7 promoter, an internal His-tag for protein purification, and multiple cloning sites. The recombinant LFn is expressed in Escherichia coli as an intracellular soluble protein with six tandem histidine residues at its N-terminal end. The molecular mass of LFn is about 31 kDa. Bacteria were grown in a 10-liter Bio-flow 2000 bench top bio-reactor (New Brunswick Scientific). Purification of the His-tagged proteins was conducted by using a commercial kit according to the manufacturer's protocol (Novagen). The production and biological activity testing of PA were as previously described (27).
51Cr-Release Assay Using P18 Pulsed Target Cells.
Spleen cells from immunized BALB/c mice were used as the source of CTL. The precursor CTL in the splenic cultures were stimulated in vitro by culture with gamma-irradiated and peptide-pulsed BALB/c splenocytes from unimmunized animals. After 6 days of culture at 37°C in a CO2 incubator, mature CTL (effector cells) were tested for their ability to lyse either 51Cr-labeled P18 peptide-pulsed P815 cells (positive targets) or 51Cr-labeled P815 cells not treated with peptide (negative targets). A standard 4-h cytotoxicity assay format was used with 10,000 targets per well and effector:target ratios of 40:1, 13:1, 4:1, and 1:1.
In Vitro Stimulation of Human CTL and T Helper Cells by LFn-p24/PA and LFn-NG/PA.
Adherent autologous mononuclear cells from 2 × 106 peripheral blood mononuclear cells (PBMC) were activated in 1 ml of RPMI 1640 supplemented with 10% pooled human AB serum (Sigma) in 24-well plates with 5 ng/ml granulocyte–macrophage colony-stimulating factor (GM-CSF; R & D Systems) for 1 week before adding 1 μg/ml phytohemagglutinin (PHA-P, Difco), 10 μg/ml control peptide, 10 μg/ml LFn fusion protein, and/or 10 μg/ml PA. After 2 h incubation at 37°C, the treated antigen-presenting cells were washed to remove unbound immunogen, and thawed PBMC (2 × 106 per well in 1 ml) were added. The next day, recombinant human IL-2 (a gift of Chiron Oncology) was added to a final concentration of 25–50 units/ml. Cells were fed biweekly with IL-2-containing media and tested for cytotoxicity or lymphoproliferation 10–14 days later. HIV-specific cytotoxicity was assayed by 4-h 51Cr-release assay using recombinant vaccinia virus (vv) encoding lacZ (vsc8), gag (vDK1), or nef (vnef) to infect autologous B lymphoblastoid cell line (B-LCL) target cells as described (23). Lymphoproliferation assay was performed in quadruplicate microtiter wells by measuring [3H]thymidine (0.5 μCi/well) incorporation 5 days after stimulation of 2 × 105 cells with recombinant vv-infected autologous B-LCL, 1 μg/ml PHA, or medium. Plates were harvested and read using a Packard Topcount harvester and microplate reader, and the stimulation index was calculated as the ratio: (mean cpm of stimulated wells)/(mean cpm of unstimulated control wells).
Membrane Translocation by LFn-p24/PA.
We used a direct assay described previously (24). Briefly, trypsin-nicked PA was incubated with CHO-K1 cells for 2 h at 4°C. The cells were then washed with cold PBS and incubated with 35S-labeled LFn-p24 for 2 h at 4°C. The cells were then washed extensively and exposed to Mes/gluconate buffer at 37°C and pH 4.8 for 2 min. This mimics the acidification of the endosome and permits surface delivery of LFn-tagged molecules, such as LFn-p24. Pronase E or buffer was then added to half the wells to digest surface-bound LFn-p24 that had not been internalized. The cells were then washed again, lysed, and counted. The amount of protein translocated was calculated from the ratio: (counts in the Pronase treated cells)/(counts in mock-treated cells).
Cytotoxicity Studies in Cultured Mouse Macrophages.
Mouse macrophage cells (RAW264.7) were seeded in microtiter plates at 30,000 cells per well and incubated for 48 h at 37°C with 10% CO2. After treatment with different concentrations of LF or LFn-HIV in the presence of PA for 3 h, MTS solution (Owen's reagent; Promega) was added. MTS can be reduced only by living cells into a colored soluble compound. Two hours later, absorbance at 490 nm was read. The ratio of the A490 of treated cells to the A490 of control cells is proportional to the proportion of viable cells.
Preclinical Safety Studies in Experimental Animals.
All procedures involving animals were approved by the appropriate institutional animal care and use committee. Injections for the rabbits were delivered in the thigh, alternating sides for multiple injections. Intramuscular injections in the rats were delivered as a divided dose in both thighs. Necropsies involved gross pathology determinations and histopathology evaluation, of the major organs, by a board-certified veterinary pathologist.
Results
Construction and Expression of LFn-V3, LFn-p24, LFn-Nef, and LFn-NG.
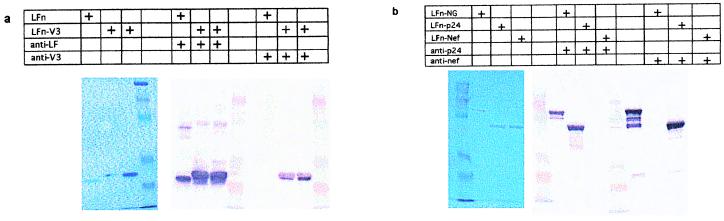
As a first step to test the fusion of LFn to larger peptides for antigenic processing and class I presentation, we used the 32-aa V3 loop of HIV-1 gp120 as the fused antigen. It contains known CTL and T helper epitopes presented in BALB/c mice (H-2d). Because the CTL P18 epitope (16) is located at the center of the 32 amino acids of the V3 loop, it would require in vivo processing for presentation on MHC class I molecules. Purified LFn-V3 is a 34-kDa soluble protein in cell extracts that reacts with rabbit polyclonal antibodies to LFn and to a mouse monoclonal antibody to the V3 peptide (Fig. 1a). The protein is stable and soluble after one-step purification by affinity chromatography. We also constructed LFn fusions with HIV-1 gag p24 (231 aa) and nef (204 aa), which are prominent HIV-1 antigens for CTL responses during natural HIV infection (17–21). Both LFn-p24 and LFn-nef can be produced with more than 95% purity in a stable and soluble form. A typical 10-liter bench-top fermentation usually produces at least 100 mg of the LFn-p24 or LFn-nef fusion protein. We further tested the ability of the toxin system to mediate the internalization of a large LFn-fusion protein by inserting the sequence for nef between LFn and gag p24 to produce an approximately 83-kDa fusion protein (LFn-NG) containing 51 kDa of combined HIV-1 antigen. The fusion protein LFn-NG is also soluble in the cell extract and stable at physiological conditions. The size of LFn-NG is approximately the same as the native LF (Fig. 1b).
Figure 1.
SDS-gel electrophoresis and Western analysis of purified LFn-V3, LFn-p24, LFn-nef, and LFn-NG. (Left, of both a and b) Purified LFn and its fusion proteins stained with Coomassie brilliant blue. Western blot analysis is shown in the Middle [anti-LFn rabbit serum (a) and anti-HIV p24 serum (b)] and Right [anti-HIV V3 mouse monoclonal antibody (a) and anti-HIV nef mouse serum (b)].
LFn-V3/PA Immunization Induces a CTL Response in BALB/c Mice.
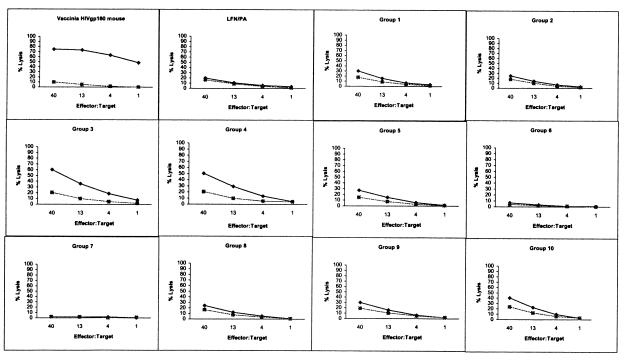
The P18 peptide derived from the HIV-1 V3 loop can be presented by MHC class I molecules of BALB/c mice, thus enabling us to test whether immunization with the epitope delivered as an LFn fusion protein can elicit CTL in vivo. Because the nine amino acids representing the epitope reside in the middle of the V3 insertion in the LFn fusion, we hoped to demonstrate that antigen processing occurred in vivo to present this epitope by the MHC class I molecule Dd. Comparing LFn-V3 with the previously reported LFn-LLO, LFn-LCMV, and LFn-OVA (13, 14), which carry the minimum epitope only, our goal was to extend the utility of LFn/PA delivery from peptide epitopes to a bigger protein antigen. Five groups of BALB/c mice, four in each group, were immunized i.m. with increasing doses of LFn-V3 plus PA. Five-fold dose escalations of LFn-V3 from 1.2 to 750 pmol (0.038–24 μg) were administered, keeping the LFn-V3 to PA molar ratio constant at 5:1. Five additional groups of mice received only LFn-V3 at the same doses without PA. Two additional groups were immunized as negative and positive controls. The negative control group received 30 pmol LFn (with no fused antigen) and 6 pmol PA. The positive control mice were immunized with recombinant vv expressing HIV-1 gp160. All mice were re-immunized 10 wk later with exactly the same formulation given to each group. CTL assays were conducted 7 days after the first immunization and 4 wk after the second immunization using in vitro-stimulated splenocytes as effector cells and P18 peptide-pulsed P815 cells as targets. Seven days after the first immunization, cultures from all groups showed no significant CTL activity (data not shown). After the second immunization, significant CTL induction in some of the groups was observed (Fig. 2). Animals that received LFn plus PA had no detectable activity. P18-specific CTL induction by LFn-V3 plus PA was dose-dependent. The highest CTL activity resulted from the immunization with 30 pmol (0.88 μg) of LFn-V3 plus 6 pmol of PA (Fig. 2, Group 3), whereas either lower or higher doses of the same immunogen complex resulted in lower CTL activities (Groups 1,2, 4, and 5). (We thus define this dose as the optimal mouse effective dose, OMED.) CTL induction by LFn-V3 also appeared to be PA-dependent when comparing groups 3 and 4 to groups 8 and 9. At a higher dose of LFn-V3, CTL induction appeared to be less PA-dependent (Group 5 vs. Group 10). The OMED of LFn-V3 is similar to the lethal dose of wild-type anthrax toxin (0.8 μg) in experimental animals (22). As expected, all of the animals showed no adverse effects from the injection, even at the highest dose of 24 μg/mouse (Groups 5 and 10).
Figure 2.
HIV-specific CTL induction in BALB/c mice immunized twice with LFn-V3, with (Groups 1–5) or without (Groups 6–10) PA. Group 1 received 1.25 pmol of LFn-V3 plus 0.24 pmol of PA, whereas Group 6 received 1.25 pmol of LFn-V3 without PA. Immunization doses were escalated by a factor of 5 using an LFn-V3:PA molar ratio of 5:1. Group 2 received 6 pmol of LFn-V3/1.2 pmol of PA; Group 7, 6 pmol of LFn-V3; Group 3, 30 pmol of LFn-V3/6 pmol of PA; Group 8, 30 pmol of LFn-V3; Group 4, 150 pmol of LFn-V3/30 pmol of PA; Group 9, 150 pmol of LFn-V3; Group 5, 750 pmol of LFn-V3/150 pmol of PA; and Group 10, 750 pmol of LFn-V3. The percent lysis was calculated by using the formula: [Experimental release) − (spontaneous release)]/[(Maximum release) − (spontaneous release)] × 100. ⧫, P815P18; ▪, P815 No Ag.
We note that the CTL response to LFn-V3 plus PA (Fig. 2, Group 3) is lower than that to the recombinant vv expressing HIV-1 gp160, suggesting that, in its current form, this approach is not as robust as the live virus-vectored immunization in raising CTL in the inbred mouse.
LFn-p24/PA and LFn-NG Elicit Human HIV-Specific CD8 T cells in Vitro.
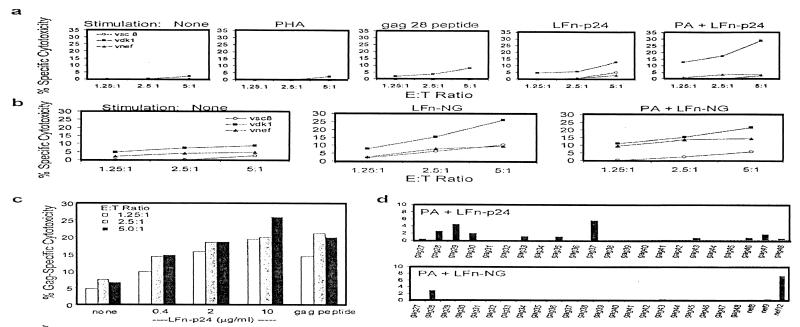
Because of MHC class I restriction, presentation of the identified human CTL epitopes in HIV-1 p24 and nef cannot be tested in BALB/c mice or rhesus monkeys. Therefore, immunogenicity of the candidate vaccine was further tested in an in vitro assay using PBMC from HIV-seropositive donors whose CTL are known to recognize immunodominant epitopes contained within HIV-1 p24 and nef (23). Adherent autologous PBMC, that had been activated with GM-CSF, were treated for 2 h at 37°C with 10 μg/ml each of LFn-HIV and PA, washed to remove unbound antigen, and then used as antigen-presenting cells in an in vitro assay to measure the induction of a secondary immune response in vitro. Fourteen days after stimulation with these treated antigen-presenting cells, PBMC were tested for cytotoxicity against autologous B cells infected with recombinant vv expressing either HIV proteins or a lacZ control. Representative data using PBMC from a donor whose CTL recognize epitopes contained within p24143–162 (peptide gag28: VHQAISOPRTLNAWVKVVEEK), nef71–90 (peptide nef8: PEVPLRPMTYKAAVDLSHFL), and nef111–130 (peptide nef12: LWIYHTQGYFPDWQNYTPGPGV) are shown (Fig. 3). In the absence of PA, the vaccine was weakly immunogenic (comparable to gag 28 peptide). In the presence of PA, the CTL response was significantly amplified and was detected even at an E:T ratio of 1.25:1. The PA dependence of the response suggests that internalization of the fusion protein is delivered by PA as postulated. The response was also specific because a nef response was not amplified. The in vitro CD8 T cell response to PA plus LFn-p24 was dose-dependent, showing increasing responses as the amount of LFn-p24 was increased from 0.4 to 10 μg/ml, while keeping the concentration of PA fixed. In experiments with PBMC from three donors, including the subject shown above, there was no in vitro amplification of the CTL response to antigen-presenting cells treated with LFn-nef plus PA. (data not shown) The LFn-NG construct containing nef and gag p24 was also tested in samples from the same patient. Responses to both nef and gag were induced, but some response to p24 was induced even in the absence of PA (Fig. 3). We are currently investigating the nature of this PA-independent function.
Figure 3.
LFn-p24 and LFn-NG induce human HIV-specific CTL in an in vitro vaccination assay. Adherent PBMC from asymptomatic HIV-infected donor 606 (a–d) were activated with GM-CSF and treated for 2 h with nothing, PHA, HIV immunodominant peptide, or LFn-p24 or LFn-NG in the presence or absence of PA, before adding autologous PBMC. Ten to fourteen days later, the induction of a secondary CD8 T cell response was measured by 51Cr-release assay against autologous B cell lines infected with recombinant vv expressing gag (vdk1), nef (vnef), or lacZ control (vsc8). (a) LFn-p24 induces gag-specific CTL from donor 606 as much as the immunodominant peptide, gag 28. However, the response is greatly enhanced by PA delivery of the antigen. (b) LFn-NG when added with PA stimulates both gag- and nef-specific CTL activity from the same donor. (c) The induction of gag-specific CTL by LFn-p24 is dose-dependent in the presence of a fixed amount of PA (10 μg/ml). (d) CTL from subject 606 recognize immunodominant epitopes in gag28, nef 8, and nef 12. Stimulation of PBMC from donor 606 with LFn-p24 plus PA induces a response to the subdominant epitope gag37. Data from a 4-h assay performed at an E:T ratio of 5:1 are shown. The activities are presented as the percentage of HIV-1 gag-specific cytotoxicity.
To determine whether these candidate vaccines stimulate the immunodominant or subdominant (“cryptic”) CTL responses, epitope mapping was performed on samples from the same patient stimulated with PA plus LFn-p24 or LFn-NG. The nef-containing vaccine stimulated a response to nef12, but not nef8, the other immunodominant epitope recognized by this subject. Exposure to LFn-p24, but not LFn-NG, appeared to stimulate response to a subdominant p24 epitope in the gag 37 peptide. These results suggest that different LFn constructs containing the same sequences may be processed within the cell in somewhat different ways and vary in the responses they generate.
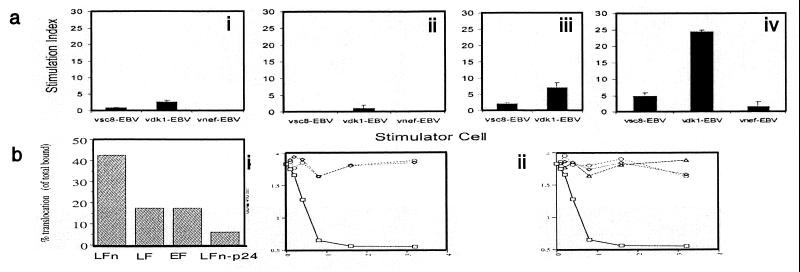
Our preliminary studies have mostly focused on the CD8 T cell response. However, in one Center for Disease Control stage A1 HIV-seropositive subject who had a weak CTL response to nef and gag, we noticed that ≈95% of the cells that grew out of the LFn-NG/PA-stimulated cultures were CD4+. This suggested that the vaccine might be stimulating a CD4 response, even though fresh PBMC from this donor did not proliferate to purified p24 Ag obtained from two sources (Protein Sciences and Virogenetics, data not shown). We therefore tested the stimulated cultures for proliferation to HIV antigens (Fig. 4a). To avoid possible crossreaction to antigens in PA or LFn, the LFn-p24/PA- or LFn-NG/PA-treated cultures were tested for proliferation to autologous B-LCL that had been infected with recombinant vv expressing gag, nef, or lacZ. There was a strong proliferative response to p24 (SI = 24.4) in the cultures stimulated with LFn-NG, a possible response in the LFn-p24-treated cultures (SI = 7.1) and no response above background to p24 in the control cultures treated with no stimulation (SI = 2.7) or PHA (SI = 1.1). These results suggest that the proposed vaccines can also stimulate a CD4 T cell response and that the efficiency with which different constructs do this may vary.
Figure 4.
(a) Lymphoproliferative (LP) response to gag p24 induced by in vitro stimulation of PBMC from HIV-seropositive donor 604 with LFn-NG. This donor did not have any detectable LP response to gag when fresh PBMC were tested against recombinant HIV-1 p24 protein (not shown). Stimulation was by adherent autologous PBMC treated with nothing (i), PHA (ii), LFn-p24 + PA (iii), or LFn-NG + PA (iv). Stimulated cultures contained approximately 95% CD4 T cells. LPA was performed by testing proliferation to autologous EBV-transformed B cells infected with recombinant vaccinia expressing lacZ (vsc8), gag (vDK1), or nef (vnef). (b) In vitro translocation of LFn-p24. LFn, full-length LF, full-length EF, and LFn-p24 were tested for translocation in the presence of PA. Bars represent the percent of bound protein internalized into CHO-K1 cells. (c) In vitro cytotoxicity of LF and LFn fusion proteins in the presence or the absence of PA in a macrophage cell line. (i) Cultures were exposed to PA only (◊) at concentrations of 0.1–3.2 μg/ml, LF only (○), or both (□) at a 2:1 ratio by weight. The LD50 for native LT is 0.4 μg/ml LF plus 0.2 μg/ml PA. (ii) Although □ represents the cytotoxic effect of LF in the presence of PA, LFn-p24 (○) and LFn-NG (◊) in the presence of PA showed no significant effect. The effect of PA alone is represented with ▵.
Membrane Translocation by LFn-p24.
We also tested the internalization of the LFn-p24 fusion proteins into cultured cells using proteolytically activated PA. After inducing delivery at the cell surface by lowering the pH, cells were treated with Pronase E to digest proteins that bound to the surface but had not been translocated into cells. Protected intracellular proteins were then analyzed by SDS/PAGE. As seen in Fig. 4b, 6.4% of bound LFn-p24 translocated into the cell in this assay. Several LFn fusion proteins have been described that do not translocate (24), and they translocated at 0% in this assay (data not shown).
LFn-p24 Fusion Constructs Are Not Toxic in Vitro and in Vivo.
Further evaluation of LFn-p24/PA as an HIV-1 vaccine candidate for clinical testing in humans requires rigorous safety studies. Although previous studies have demonstrated that removing the toxic domain of LF completely abolishes the toxicity of LT both in vitro and in vivo, we confirmed the safe usage of the proposed vaccine construct in cultured cells and in experimental animals. Treatment of mouse macrophage cells in vitro with LT results in rapid cell lysis. We therefore developed a test to analyze the cytotoxicity of recombinant LF fusions in the presence of PA. Fig. 4c shows that 0.4 μg/ml of native LF plus 0.2 μg/ml PA results in death of 50% of mouse macrophage cells. Neither LF nor PA alone is cytotoxic. However, at the highest concentration of LFn-p24 or LFn-NG plus PA tested (3.2 μg/ml), no significant cell killing was observed. We then tested the toxicity of LFn-p24 plus PA in experimental rabbits. In an acute toxicology study, four groups of NZW rabbits, four in each group, were injected with 0, 100, 500, or 2000 μg of LFn-p24 plus PA at a 2:1 ratio by weight. All rabbits survived the injection with no significant adverse response. Necropsies also revealed no detectable abnormality at the injection site or in any organ, including the liver, heart, and spleen (data not shown). Sixteen additional rabbits were injected three times with the same vaccine doses (LFn/PA in μg: 0/0, 100/50, 500/250, 2000/1000). All animals survived the injections and daily observation, and two subsequent post exposure necropsies raised no safety concerns (data not shown).
We also conducted a safety test of LFn-p24/PA using Fisher 344 rats, the most sensitive animal model for anthrax toxin. Injection of 0.8 μg native LT results in death within 1 h (18). Four groups of rats, three in each group, were i.m. injected with 0, 100, 500, and 2000 μg LFn-p24 plus PA at a 2:1 ratio by weight. All animals survived the injection and showed no detectable adverse signs. Necropsy of all of the animals at 14 days postinjection revealed no significant pathologic effect associated with the injection (data not shown). Further safety studies in macaques are in progress.
Discussion
The LFn-p24/PA and LFn-NG/PA constructs possess desirable features as candidate T cell-dependent HIV vaccines. Previous studies showed that LFn fusions carrying a single CTL epitope of 9–12 amino acids were able to elicit protective CTL in mice. Here, we demonstrate that LFn fused to a 33-aa polypeptide can elicit CTL in animals, suggesting that the polypeptide is processed in the cytosol for MHC class I presentation. We also showed that this approach is capable of presenting recombinant polypeptides in vitro that are as large as 500 aa, including the entire HIV-1 p24 plus the nef protein. Such a capacity is critically important for generating CD8-specific CTL because of the relatively larger number of class I alleles found in the human population. Most HIV-infected donors have detectable CTL against a variety of epitopes present in several HIV-1 antigens, which vary significantly depending on the HLA class I allele. Even in subjects with the same HLA class I haplotype, the detectable CTL response is not necessarily identical (17). It is, therefore, impossible to select one specific CTL epitope, or group of selected epitopes, for a vaccine intended to stimulate CD8 T cells for use in a genetically diverse population. This is an obstacle for vaccine designs that use synthetic peptides or small recombinant antigens. LFn-p24 and LFn-NG were stable and soluble at physiologic conditions. Because the typical bench-top production yields between 100–400 mg of purified fusion protein, these vaccine candidates have the potential for being a cost-effective product. Production of LFn-p24 and recombinant PA in compliance with current good manufacturing practices is under way, and this candidate vaccine is expected to be tested in a phase I human trial within the year.
Because of difficulties with MHC class I restriction, we are unable to evaluate fully in animal models the potential immunogenicity of LFn-p24/PA or LFn-NG/PA. We have been able to demonstrate, however, that LFn-V3 immunization of mice appears to be immunogenic, eliciting anti-HIV CTL with as little as 0.8 μg of the recombinant fusion protein. We hypothesize that such efficiency may result from the ability of the vaccine to usurp the natural activity of the binary lethal toxin to deliver antigen to the cytosol. This hypothetical mechanism of internalization is supported by the membrane translocation study of LFn-p24 protein and the PA dependence of the immune response at lower doses in vivo in mice and in vitro in humans.
The LFn/PA delivery system may also be capable of activating immunodominant as well as some “cryptic” CTL epitopes. Although there may be as many as 300 potential CTL epitopes in HIV antigens (18), some of these epitopes seem to dominate over others in stimulating human CTL (23, 25, 26). It is unclear whether CTL recognition of some nondominant or “cryptic” epitopes might be protective. One possibility is that these cryptic epitopes are not well recognized by the CTL of infected patients because they are not well presented on natural HIV-infected targets. It is also possible that the virus evolved so as not to present efficiently epitopes that might be restricted by common HLA haplotypes. Because LFn-p24/PA was able to stimulate reactivity to an additional CTL epitope not activated during natural infection, the LFn fusion protein may enter the MHC class I presentation pathway differently from HIV proteins in infected cells. Epitopes that are not presented efficiently enough to induce a dominant CTL response might still be present in sufficient copies on the infected cell to trigger CTL lysis. Estimates of the number of peptide-MHC molecules required for CTL recognition are as low as one per cell. It will therefore be important to test the ability of CTL induced by toxin fusion vaccination (or by other vaccine strategies) to trigger lysis of HIV-infected cell targets.
LFn-p24/PA shows an excellent safety profile in vitro and in vivo, consistent with current understanding of LF toxicology at the molecular level. Unlike other binary exotoxins, the toxic domain of LF can be completely dissociated from the PA-binding domain, making it possible to genetically eliminate toxicity without inactivating the mechanism for cellular internalization. In this study, Fisher rats, which are exquisitely sensitive to anthrax toxin, were treated with as much as 2500 times the OMED of LFn-p24/PA without adverse effects. The optimal LFn concentration to elicit CTL in mice is comparable to the reported lethal dose of unmodified LF (22). Taken together, we anticipate that these candidate vaccines will prove safe in humans at the doses planned (10–50 OMED).
Acknowledgments
We thank Drs. John Collier, Kevin Killeen, Urban Ramstedt, David Beattie, Bryan Roberts, Henry Marsh, and Max Essex. We also wish to thank Amy Strong, Angela Woods, Lisa Moore, Carol Ferioli, Jenny Weng, Adrian Lowe, and Zhan Xu for excellent technical support. This work is supported in part by AVANT Immunotherapeutics and by National Institutes of Health Grants AI47539 (to Y.L.) and AI42671 and AI41526 (to M.S.).
Abbreviations
- CTL
cytotoxic T lymphocyte
- LT
lethal toxin
- PA
protective antigen
- LF
lethal factor
- EF
edema factor
- LFn
the PA binding domain of LF
- LCMV
lymphocytic choriomeningitis virus
- V3
variable region 3
- PBMC
peripheral blood mononuclear cell
- GM-CSF
granulocyte–macrophage colony-stimulating factor
- PHA
phytohemagglutinin
- vv
vaccinia virus
- OMED
optimal mouse effective dose
References
- 1.Ogg G S, Jin X, Bonhoeffer S, Dunbar P R, Nowak M A, Mopnard S, Segal J P, Cao Y, Rowland-Jones S L, Cerundolo V, et al. Science. 1998;279:2103–2106. doi: 10.1126/science.279.5359.2103. [DOI] [PubMed] [Google Scholar]
- 2.Schmitz J E, Kuroda M J, Santra S, Sasseville V G, Simon M A, Lifton M A, Racz P, Tenner-Racz K, Dalesandro M, Scallon B J, et al. Science. 1999;283:857–860. doi: 10.1126/science.283.5403.857. [DOI] [PubMed] [Google Scholar]
- 3.Brodie S J, Lewinsohn D A, Patterson B K, Jiyamapa D, Krieger J, Corey L, Greenberg P, Riddell S R. Nat Med. 1999;5:34–41. doi: 10.1038/4716. [DOI] [PubMed] [Google Scholar]
- 4.Letvin N L. Science. 1998;280:1875–1879. doi: 10.1126/science.280.5371.1875. [DOI] [PubMed] [Google Scholar]
- 5.Pamer E, Cresswell P. Annu Rev Immunol. 1998;16:323–358. doi: 10.1146/annurev.immunol.16.1.323. [DOI] [PubMed] [Google Scholar]
- 6.Milne J C, Furlong D, Hanna P C, Wall J S, Collier R J. J Biol Chem. 1994;269:20607–20612. [PubMed] [Google Scholar]
- 7.Petosa C, Collier R J, Klimpel K R, Leppla S H, Liddington R C. Nature (London) 1997;385:833–838. doi: 10.1038/385833a0. [DOI] [PubMed] [Google Scholar]
- 8.Leppla S H. Proc Natl Acad Sci USA. 1982;79:3162–3166. doi: 10.1073/pnas.79.10.3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klimpel K R, Arora N, Leppla S H. Mol Microbiol. 1994;13:1093–1100. doi: 10.1111/j.1365-2958.1994.tb00500.x. [DOI] [PubMed] [Google Scholar]
- 10.Duesbery N S, Webb C P, Leppla S H, Gordon V M, Klimpel K R, Copeland T D, Ahn A G, Oskarsson M K, Fukasawa K, Paull K D, Vander, Woude G F. Science. 1998;280:734–737. doi: 10.1126/science.280.5364.734. [DOI] [PubMed] [Google Scholar]
- 11.Hanna P C, Kruskal B A, Ezekowitz R A, Bloom B R, Collier R J. Mol Med. 1994;1:7–18. [PMC free article] [PubMed] [Google Scholar]
- 12.Milne J C, Blanke S R, Hanna P C, Collier R J. Mol Microbiol. 1995;15:661–666. doi: 10.1111/j.1365-2958.1995.tb02375.x. [DOI] [PubMed] [Google Scholar]
- 13.Ballard J D, Collier R J, Starnbach M N. Proc Natl Acad Sci USA. 1996;93:12531–12534. doi: 10.1073/pnas.93.22.12531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ballard J D, Doling A M, Beauregard K, Collier R J, Starnbach M N. Infect Immun. 1998;66:615–619. doi: 10.1128/iai.66.2.615-619.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goletz T J, Klimpel K R, Arora N, Leppla S H, Keith J M, Berzofsky J A. Proc Natl Acad Sci USA. 1997;94:12059–12064. doi: 10.1073/pnas.94.22.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takeshita T, Takaharshi H, Kozlowski S, Ahlers J D, Pendleton C D, Moore R L, Nakagawa Y, Yokomuro K, Fox B S, Margulies D H, Berzofsky J A. J Immunol. 1995;154:1973–1986. [PubMed] [Google Scholar]
- 17.Lieberman J, Fabry J A, Fong D M, Parkerson G R., III AIDS Res Hum Retroviruses. 1997;13:383–392. doi: 10.1089/aid.1997.13.383. [DOI] [PubMed] [Google Scholar]
- 18.Brander C, Walker B D. In: Humans Retroviruses and AIDS. Korber B T, Brander C, Haynes B F, Moore J P, Koup R, Walker BD, Bradac J A, editors. Los Alamos, NM: Los Alamos Natl. Lab.; 1997. p. 4. [Google Scholar]
- 19.Culmann B, Gomard E, Kieny M, Guy B, Dreyfus F, Saimot A, Sereni D, Sicard D, Levy J. J Immunol. 1991;146:1560–1565. [PubMed] [Google Scholar]
- 20.Haas G, Plikat U, Debre P, Lucchiari M, Katlama C, Dudoit Y, Bonduelle O, Bauer M, Ihlenfeldt H, Jung G, et al. J Immunol. 1996;157:4212–4221. [PubMed] [Google Scholar]
- 21.Goulder P, Conlon C, McIntyre K, McMichael A. AIDS. 1996;10:1441–1443. doi: 10.1097/00002030-199610000-00025. [DOI] [PubMed] [Google Scholar]
- 22.Leppla S H. Sourcebook of Bacterial Protein Toxins. New York: Academic; 1991. pp. 277–302. [Google Scholar]
- 23.Lieberman J. In: Symposium in Immunology. Eibl V M M, Huber C, Peter H H, Wahn U, editors. Berlin: Springer; 1996. pp. 55–64. [Google Scholar]
- 24.Wesche J, Elliott J L, Falnes P, Olsnes S, Collier R J. Biochemistry. 1998;37:15737–15746. doi: 10.1021/bi981436i. [DOI] [PubMed] [Google Scholar]
- 25.Lieberman J, Fabry J A, Kuo M C, Earl P, Moss B, Skolnik P R. J Immunol. 1992;148:2738–2747. [PubMed] [Google Scholar]
- 26.Shankar P, Fabry J, Fong D M, Lieberman J. Immunol Lett. 1996;52:23–30. doi: 10.1016/0165-2478(96)02574-6. [DOI] [PubMed] [Google Scholar]
- 27.Ivins B E, Welkos S L. Infect Immun. 1986;54:537–542. doi: 10.1128/iai.54.2.537-542.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]