Abstract
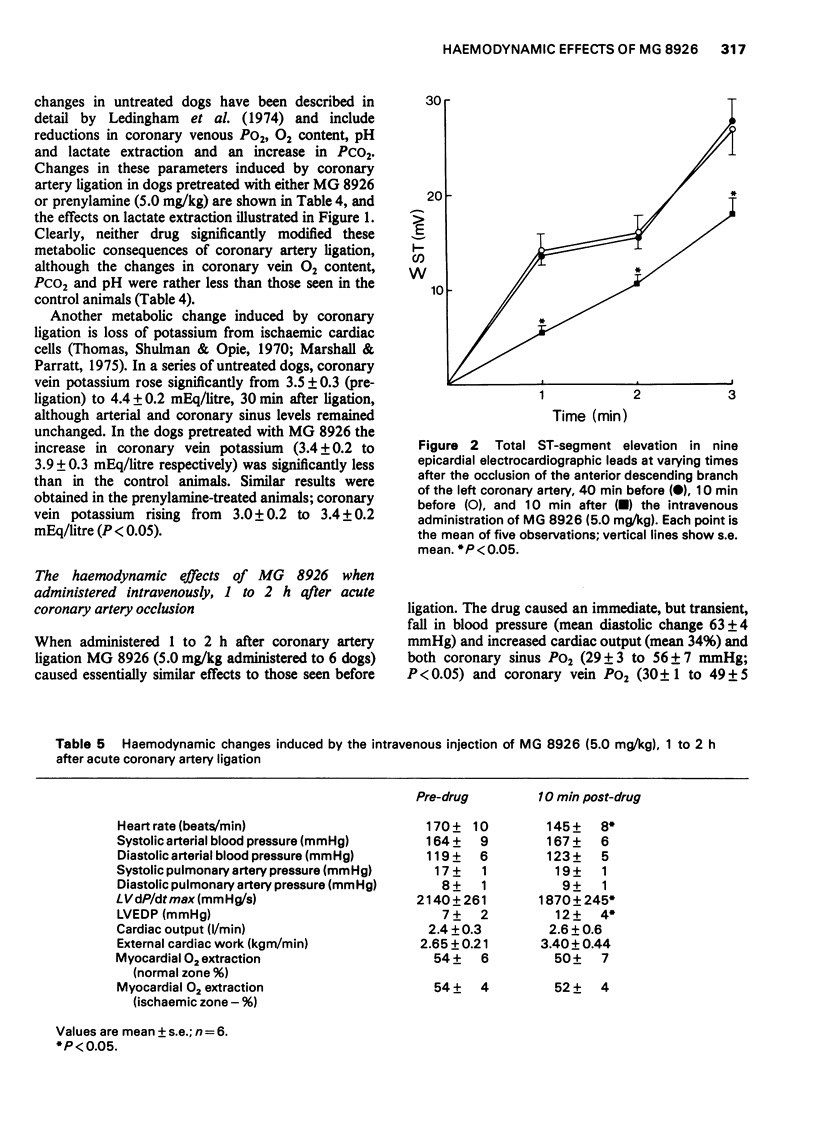
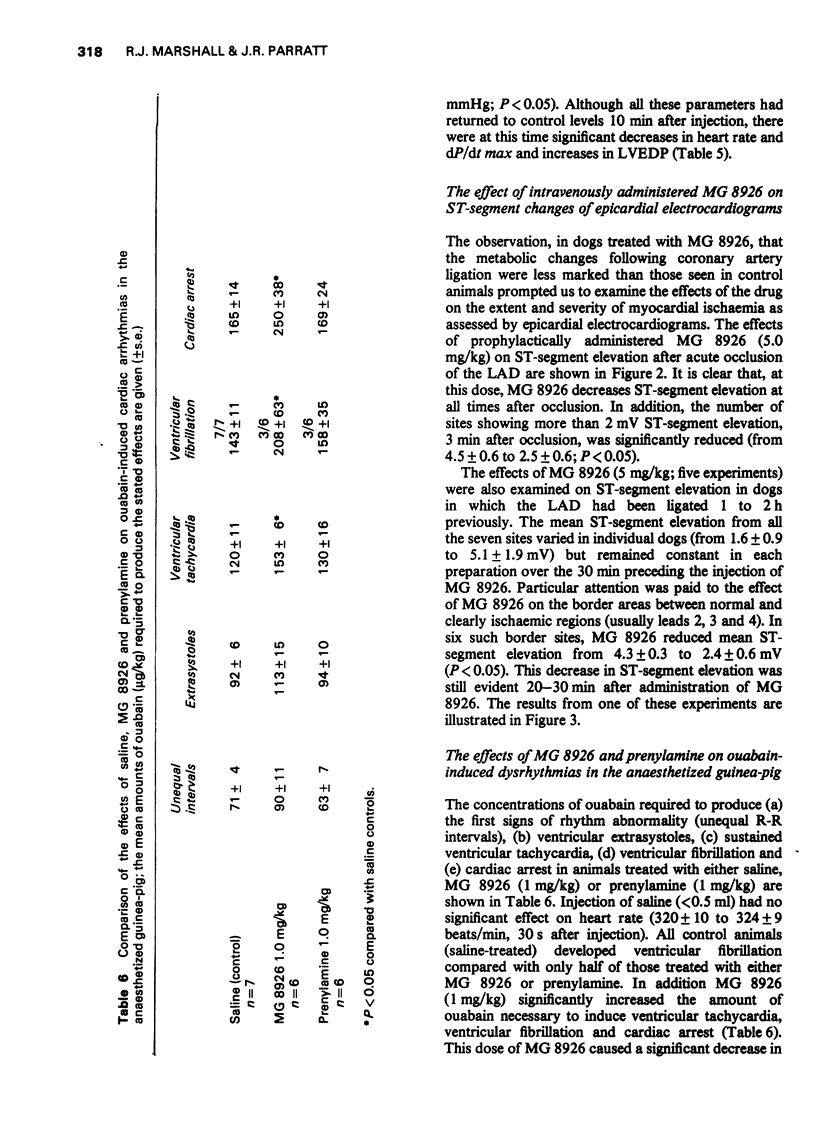
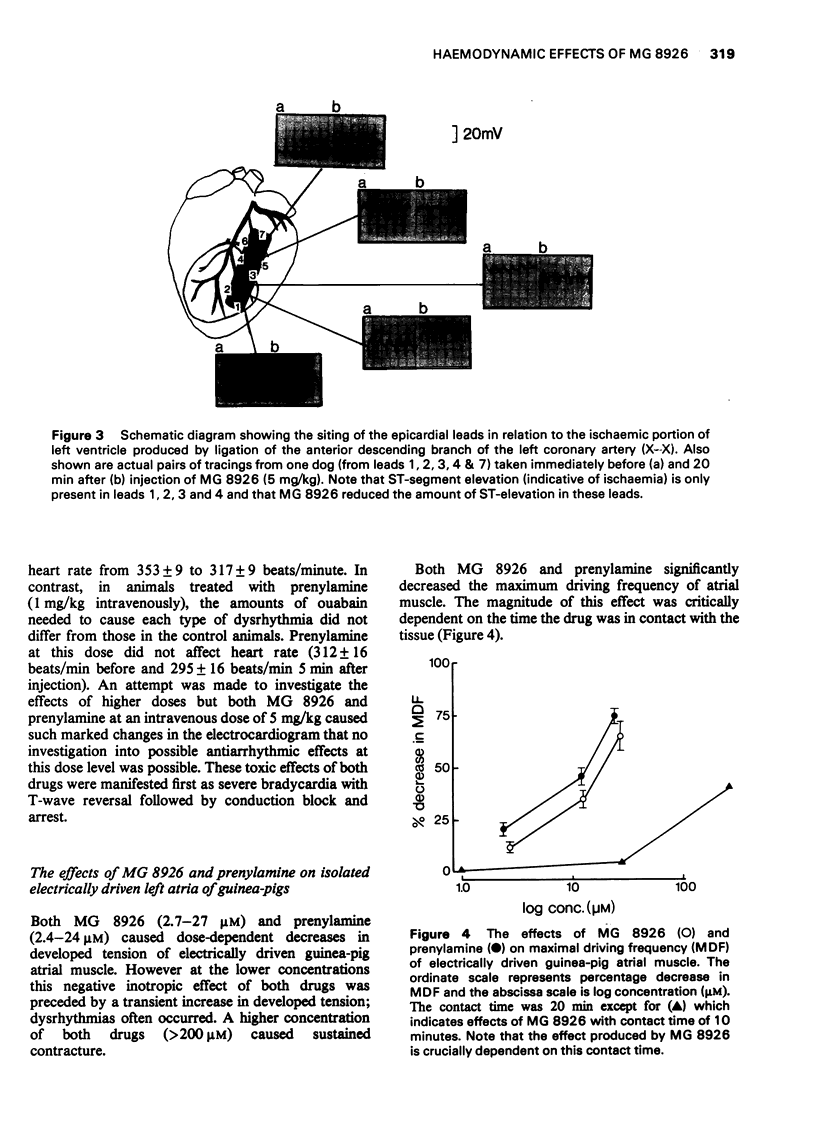
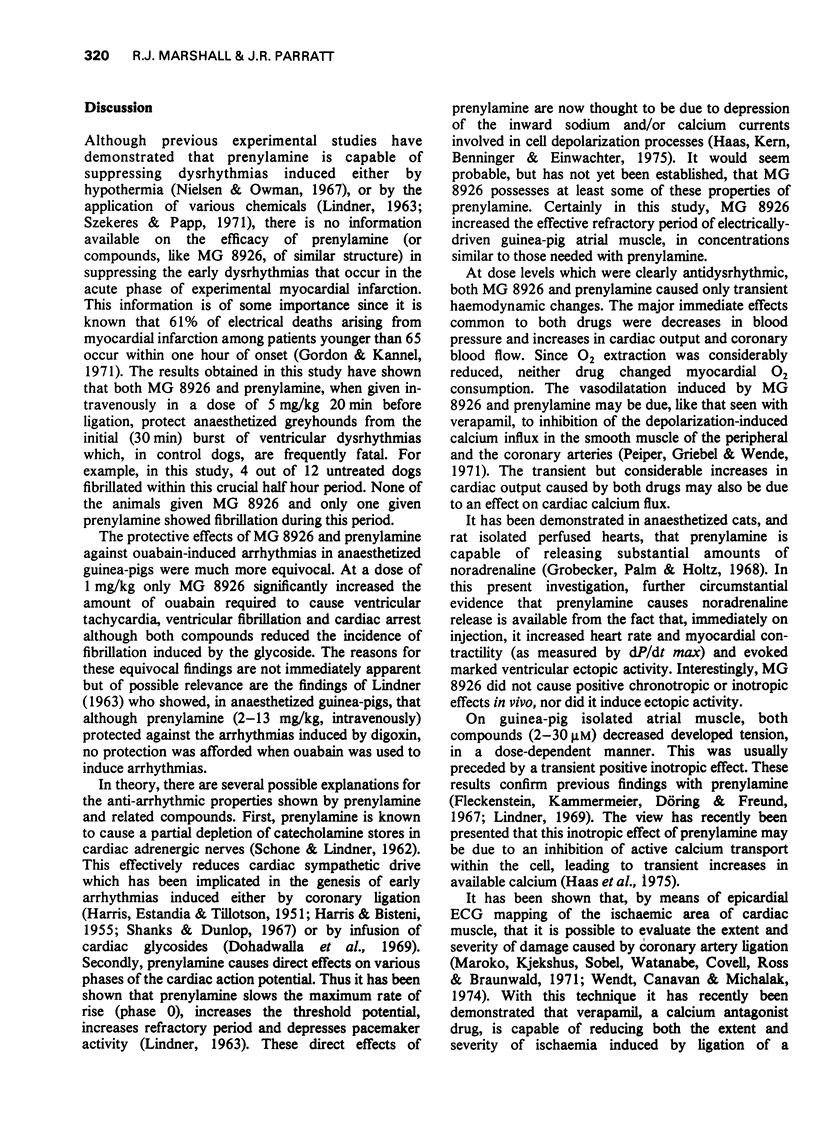
1 The antidysrhythmic, haemodynamic and metabolic effects of a new prospective antianginal and antidysrhythmic agent, N-(3-3-dipenylpropyl)-alpha-methyl-beta-cyclohexylethylamine hydrochloride (MG 8926), have been compared with the chemically related substance, prenylamine, in anaesthetized greyhounds and guinea-pigs. 2 When given intravenously 20 min beforehand, both MG 8926 and prenylamine (5 mg/kg) significantly suppressed the early dysrhythmias induced by coronary artery ligation in anaesthetized greyhounds. At a dose of 1 mg/kg, MG 8926 also protected anaesthetized guinea-pigs from dysrhythmias induced by ouabain infusions. 3 In dogs pretreated with MG 8926, metabolic changes indicative of myocardial ischaemia (increased PCO2 and potassium efflux, decreased oxygen content and pH) were less marked than those occurring in control animals. 4 Evidence was obtained that MG 8926, when given either before or after coronary occlusion, was capable of decreasing the severity of myocardial ischaemia as assessed by ST-segment changes in epicardial electrocardiograms.
Full text
PDF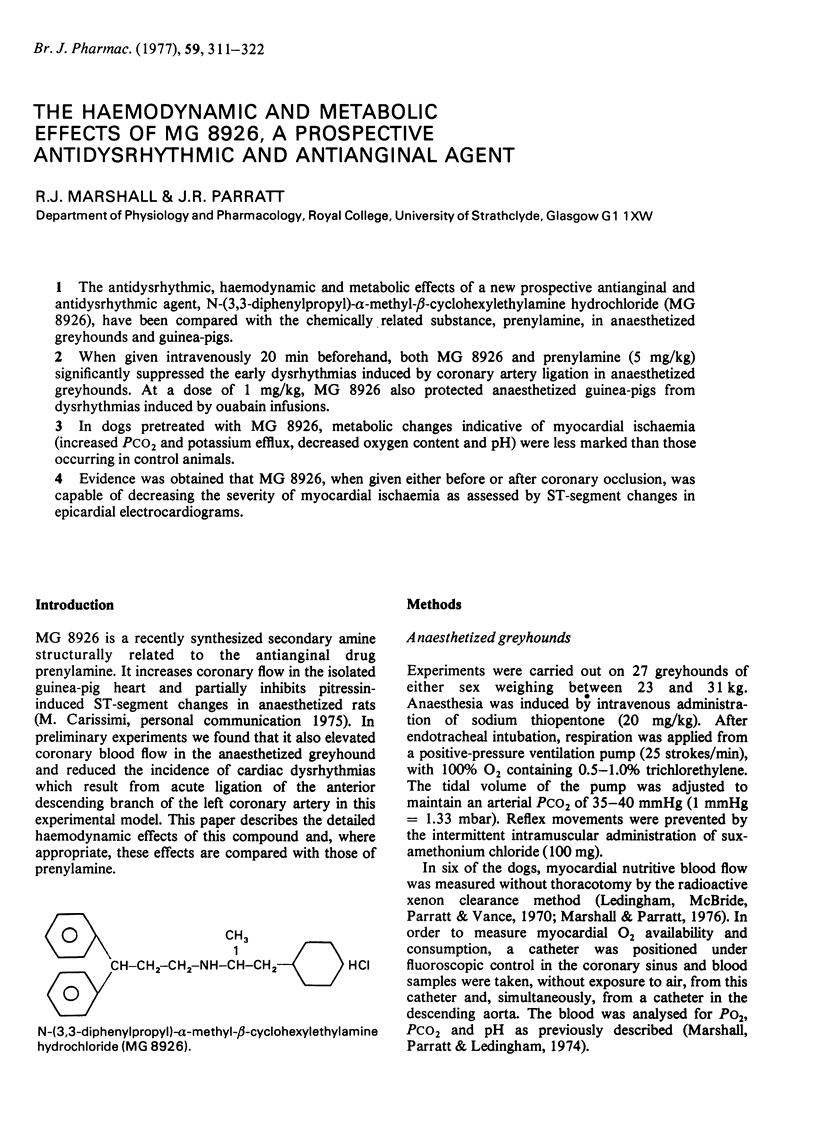
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dohadwalla A. N., Freedberg A. S., Vaughan Williams E. M. The relevance of beta-receptor blockade to ouabain-induced cardiac arrhythmias. Br J Pharmacol. 1969 Jun;36(2):257–267. doi: 10.1111/j.1476-5381.1969.tb09503.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas I. R., MacDonald J. A., Milligan G. F., Mellon A., Ledingham I. M. A comparison of methods for the measurement of cardiac output and blood oxygen content. Br J Anaesth. 1975 Apr;47(4):443–450. doi: 10.1093/bja/47.4.443. [DOI] [PubMed] [Google Scholar]
- ELLIS C. H. Screening of drugs for anti-arrhythmic activity. Ann N Y Acad Sci. 1956 Nov 16;64(4):552–563. doi: 10.1111/j.1749-6632.1956.tb36829.x. [DOI] [PubMed] [Google Scholar]
- Fleckenstein A., Kammermeier H., Döring H. J., Freund H. J. Zum Wirkungsmechanismus neuartiger Koronardilatatoren mit gleichzeitig Sauerstoff-einsparenden Myokard-Effekten, Prenylamin und Iproveratril. 1. Z Kreislaufforsch. 1967 Jul;56(7):716–744. [PubMed] [Google Scholar]
- Gordon T., Kannel W. B. Premature mortality from coronary heart disease. The Framingham study. JAMA. 1971 Mar 8;215(10):1617–1625. [PubMed] [Google Scholar]
- Grobecker H., Palm D., Holtz P. Zur Pharmakologie des Prenylamins. Naunyn Schmiedebergs Arch Exp Pathol Pharmakol. 1968;260(5):379–399. [PubMed] [Google Scholar]
- Gross G. J., Winbury M. M. Beta adrenergic blockade on intramyocardial distribution of coronary blood flow. J Pharmacol Exp Ther. 1973 Dec;187(3):451–464. [PubMed] [Google Scholar]
- HARRIS A. S., BISTENI A. Effects of sympathetic blockade drugs on ventricular tachycardia resulting from myocardial infarction. Am J Physiol. 1955 Jun;181(3):559–566. doi: 10.1152/ajplegacy.1955.181.3.559. [DOI] [PubMed] [Google Scholar]
- Haas H. G., Kern R., Benninger C., Einwächter H. M. Effects of prenylamine on cardiac membrane currents and contractility. J Pharmacol Exp Ther. 1975 Mar;192(3):688–701. [PubMed] [Google Scholar]
- LINDNER E. UNTERSUCHUNGEN UEBER DIE FLIMMERWIDRIGE WIRKUNG DES N-(3'-PHENYL-PROPYL-(2'))-1,1-DIPHENYLPROPYL-(3)-AMINS (SEGONTIN) Arch Int Pharmacodyn Ther. 1963 Dec 1;146:485–500. [PubMed] [Google Scholar]
- Ledingham I. M., McBride T. I., Parratt J. R., Vance J. P. The effect of hypercapnia on myocardial blood flow and metabolism. J Physiol. 1970 Sep;210(1):87–105. doi: 10.1113/jphysiol.1970.sp009197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledingham I. M., Parratt J. R., Smith G., Vance J. P. Haemodynamic and myocardial effects of hyperbaric oxygen in dogs subjected to haemorrhage. Cardiovasc Res. 1971 Jul;5(3):277–285. doi: 10.1093/cvr/5.3.277. [DOI] [PubMed] [Google Scholar]
- Marhsall R. J., Parratt J. R. The effect of noradrenaline on blood flow and oxygen consumption in normal and ischemic areas of myocardium. Am Heart J. 1973 Nov;86(5):653–662. doi: 10.1016/0002-8703(73)90343-8. [DOI] [PubMed] [Google Scholar]
- Maroko P. R., Kjekshus J. K., Sobel B. E., Watanabe T., Covell J. W., Ross J., Jr, Braunwald E. Factors influencing infarct size following experimental coronary artery occlusions. Circulation. 1971 Jan;43(1):67–82. doi: 10.1161/01.cir.43.1.67. [DOI] [PubMed] [Google Scholar]
- Marshall R. J., Parratt J. R. Antiarrhythmic, haemodynamic and metabolic effects of 3alpha-amino-5alpha-androstan-2beta-ol-17-one hydrochloride in greyhounds following acute coronary artery ligation. Br J Pharmacol. 1975 Nov;55(3):359–368. doi: 10.1111/j.1476-5381.1975.tb06939.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall R. J., Parratt J. R. Comparative effects of propranolol and practolol in the early stages of experimental canine myocardial infarction. Br J Pharmacol. 1976 Jun;57(2):295–303. doi: 10.1111/j.1476-5381.1976.tb07479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall R. J., Parratt J. R., Ledingham I. M. Changes in blood flow and oxygen consumption in normal and ischaemic regions of the myocardium following acute coronary artery ligation. Cardiovasc Res. 1974 Mar;8(2):204–215. doi: 10.1093/cvr/8.2.204. [DOI] [PubMed] [Google Scholar]
- Marshall R. J., Parratt J. R. Reduction in ventricular arrhythmias following acute coronary artery ligation in the dog after the administration of creatine phosphate. Naunyn Schmiedebergs Arch Pharmacol. 1974;281(4):437–441. doi: 10.1007/BF00499438. [DOI] [PubMed] [Google Scholar]
- Nielsen K. C., Owman C. Control of ventricular fibrillation during induced hypothermia in cats after differential depletion of cardiac catecholamine stores with prenylamine (Segontin). Circ Res. 1967 Jul;21(1):45–58. doi: 10.1161/01.res.21.1.45. [DOI] [PubMed] [Google Scholar]
- Peiper U., Griebel L., Wende W. Activation of vascular smooth muscle of rat aorta by noradrenaline and depolarization: two different mechanisms. Pflugers Arch. 1971;330(1):74–89. doi: 10.1007/BF00588736. [DOI] [PubMed] [Google Scholar]
- Shanks R. G., Dunlop D. Effect of propranolol on arrhythmias following coronary artery occlusion in dogs. Cardiovasc Res. 1967 Jan;1(1):34–41. doi: 10.1093/cvr/1.1.34. [DOI] [PubMed] [Google Scholar]
- Smith H. J., Singh B. N., Nisbet H. D., Norris R. M. Effects of verapamil on infarct size following experimental coronary occlusion. Cardiovasc Res. 1975 Jul;9(4):569–578. doi: 10.1093/cvr/9.4.569. [DOI] [PubMed] [Google Scholar]
- Staszewska-Barczak J., Ceremuzynski L. The continuous estimation of catecholamine release in the early stages of myocardial infarction in the dog. Clin Sci. 1968 Jun;34(3):531–539. [PubMed] [Google Scholar]
- Thomas M., Shulman G., Opie L. Arteriovenous potassium changes and ventricular arrhythmias after coronary artery occlusion. Cardiovasc Res. 1970 Jul;4(3):327–333. doi: 10.1093/cvr/4.3.327. [DOI] [PubMed] [Google Scholar]
- Wende W., Bleifeld W., Meyer J., Stühlen H. W. Reduction of the size of acute, experimental myocardial infarction by Verapamil. Basic Res Cardiol. 1975 Mar-Apr;70(2):198–208. doi: 10.1007/BF01905620. [DOI] [PubMed] [Google Scholar]
- Wendt R. L., Canavan R. C., Michalak R. J. Effects of various agents on regional ischemic myocardial injury: electrocardiographic analysis. Am Heart J. 1974 Apr;87(4):468–482. doi: 10.1016/0002-8703(74)90172-0. [DOI] [PubMed] [Google Scholar]