Abstract
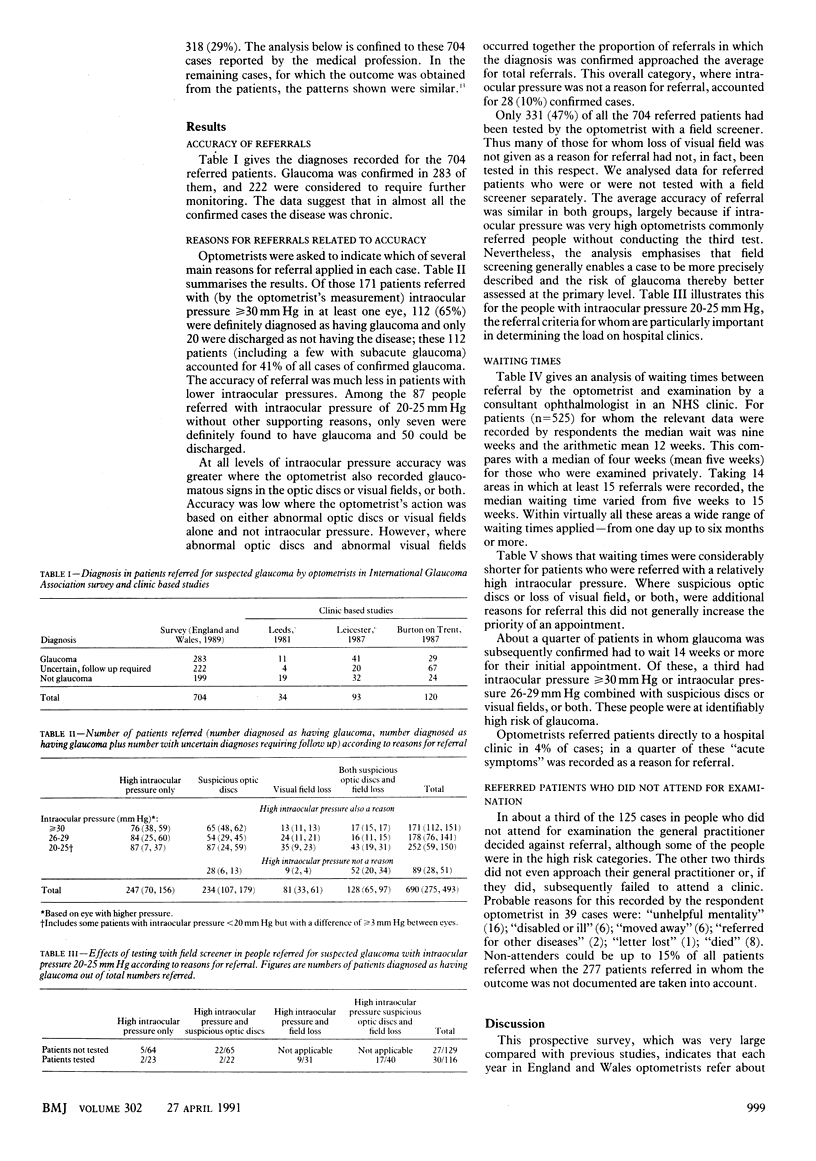
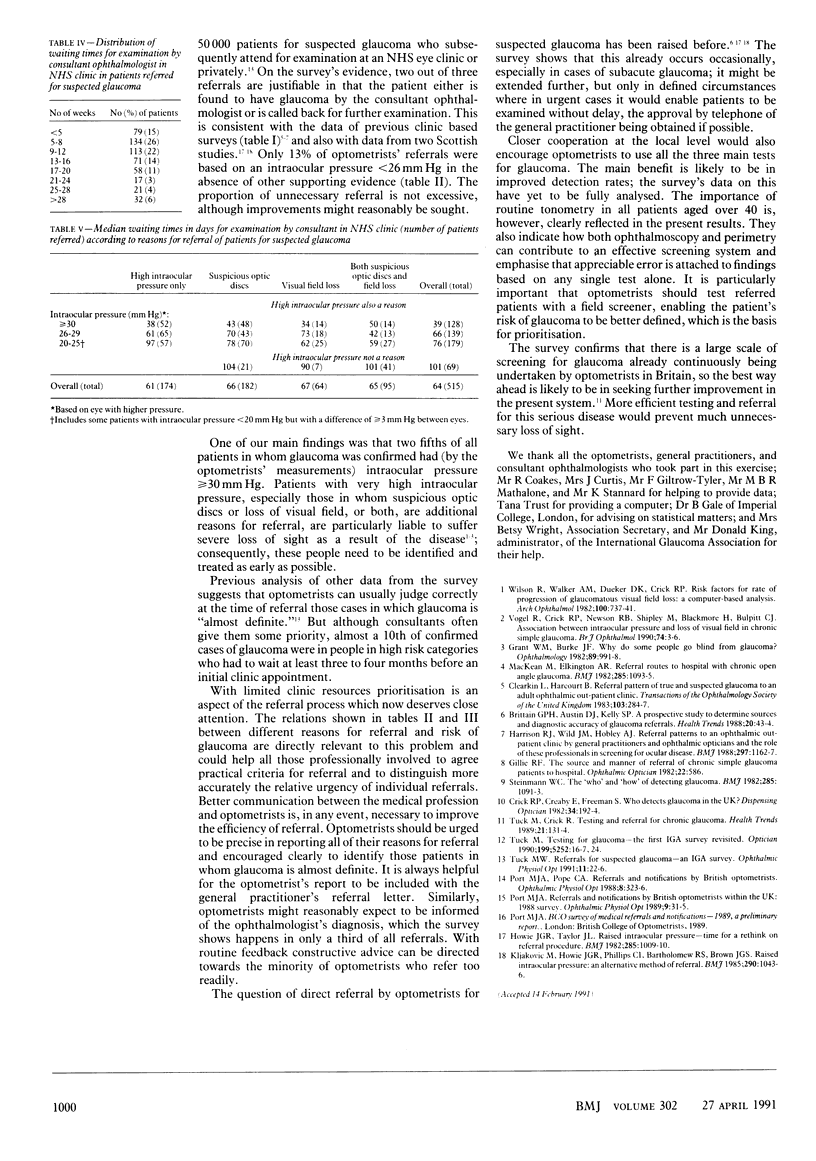
OBJECTIVE--To examine the efficiency of referral for suspected glaucoma to general practitioners and consultants by optometrists. DESIGN--A prospective survey covering 5% of all sight tests performed by optometrists in England and Wales over six months, with analysis of referred patients. SETTING--241 optometrists' practices in areas representative of England and Wales in socioeconomic terms. SUBJECTS--Of 275,600 people attending for a sight test, 1505 were referred with suspected glaucoma (0.9% of those aged over 4%). Outcomes were recorded for 1228 patients, 1103 (90%) of whom attended for examination by a consultant ophthalmologist (8% on a private basis). The analysis was confined to the 704 cases in which the information on diagnosis was received directly from a consultant or general practitioner. MAIN OUTCOME MEASURES--Diagnoses reported by consultant ophthalmologists. Waiting times before an appointment for examination by a consultant ophthalmologist. RESULTS--Glaucoma was confirmed in 283 of the 704 referred patients, and another 222 patients were considered to require further monitoring. In all, 112 (41%) of 275 confirmed cases of glaucoma were in patients with intraocular pressures greater than or equal to 30 mm Hg. At all levels of intraocular pressure the accuracy of referral was greater when the optometrist also recorded the presence of suspicious optic discs or loss of visual field, or both; but only 331 (47%) out of the 704 referred patients had been tested with a field screener. The median waiting time for an NHS clinic appointment was nine weeks. Almost a 10th of confirmed cases of glaucoma were in people in a high risk category for glaucoma who had to wait at least 14 weeks for an appointment. CONCLUSIONS--Closer cooperation, especially at the local level, among consultants, general practitioners, and optometrists is needed to improve testing and referral for suspected glaucoma. Optometrists should be encouraged to perform all the three main tests--ophthalmoscopy, tonometry, and perimetry--in patients before referral and to report precisely on reasons for referral to help prioritisation. The optometrist's referral letter to the general practitioner should always be passed on to the consultant. Similarly, the diagnosis should always be reported back to the optometrist.
Full text
PDF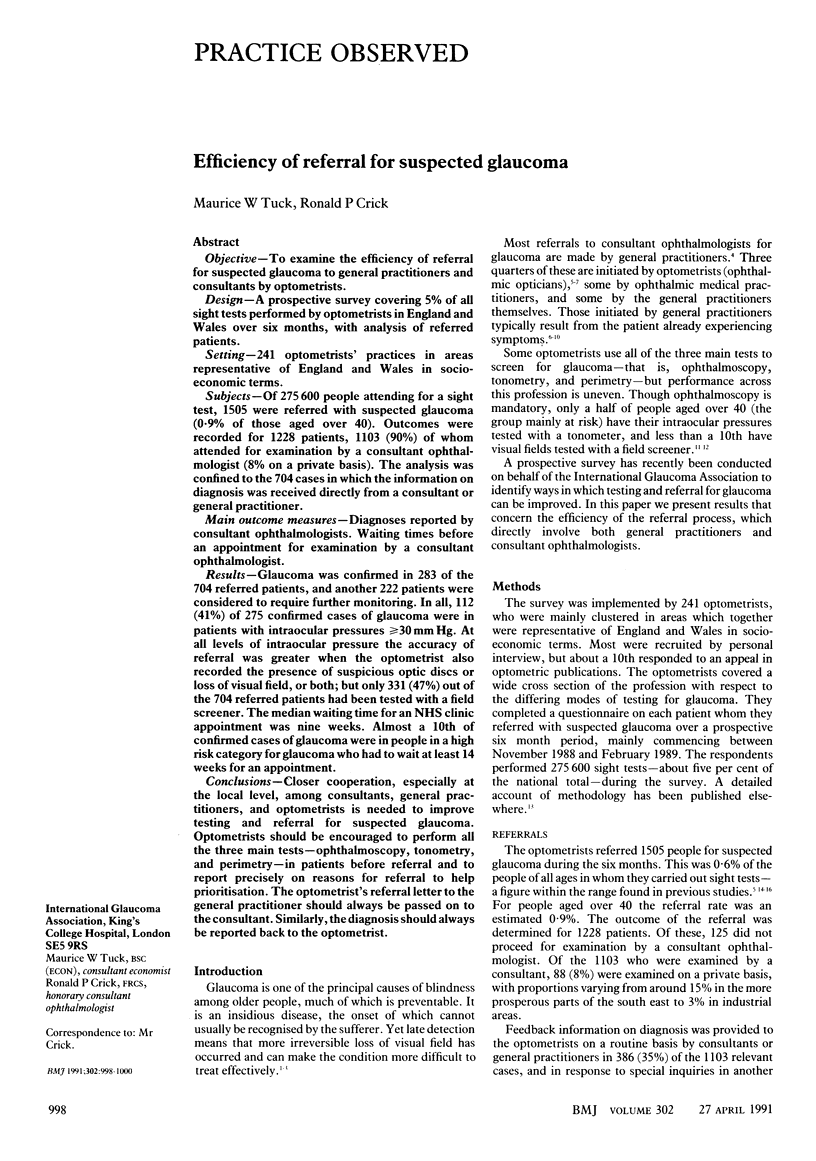
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brittain G. P., Austin D. J., Kelly S. P. A prospective survey to determine sources and diagnostic accuracy of glaucoma referrals. Health Trends. 1988 May;20(2):43–44. [PubMed] [Google Scholar]
- Clearkin L., Harcourt B. Referral pattern of true and suspected glaucoma to an adult ophthalmic outpatient clinic. Trans Ophthalmol Soc U K. 1983;103(Pt 3):284–287. [PubMed] [Google Scholar]
- Dyson R. H., Cannon S. R. Is arthroscopy always necessary?: a waiting list review. Health Trends. 1989 Feb;21(1):13–15. [PubMed] [Google Scholar]
- Grant W. M., Burke J. F., Jr Why do some people go blind from glaucoma? Ophthalmology. 1982 Sep;89(9):991–998. doi: 10.1016/s0161-6420(82)34675-8. [DOI] [PubMed] [Google Scholar]
- Harrison R. J., Wild J. M., Hobley A. J. Referral patterns to an ophthalmic outpatient clinic by general practitioners and ophthalmic opticians and the role of these professionals in screening for ocular disease. BMJ. 1988 Nov 5;297(6657):1162–1167. doi: 10.1136/bmj.297.6657.1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howie J. G., Taylor J. L. Raised intraocular pressure-time for a think on referral procedure? Br Med J (Clin Res Ed) 1982 Oct 9;285(6347):1009–1010. doi: 10.1136/bmj.285.6347.1009-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kljakovic M., Howie J. G., Phillips C. I., Bartholomew R. S., Brown J. G. Raised intraocular pressure: an alternative method of referral. Br Med J (Clin Res Ed) 1985 Apr 6;290(6474):1043–1044. doi: 10.1136/bmj.290.6474.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKean J. M., Elkington A. R. Referral routes to hospital of patients with chronic open-angle glaucoma. Br Med J (Clin Res Ed) 1982 Oct 16;285(6348):1093–1095. doi: 10.1136/bmj.285.6348.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Port M. J., Pope C. A. Referrals and notifications by British optometrists. Ophthalmic Physiol Opt. 1988;8(3):323–326. [PubMed] [Google Scholar]
- Port M. J. Referrals and notifications by optometrists within the UK: 1988 survey. Ophthalmic Physiol Opt. 1989 Jan;9(1):31–35. doi: 10.1111/j.1475-1313.1989.tb00801.x. [DOI] [PubMed] [Google Scholar]
- Steinmann W. C. The "who" and "how" of detecting glaucoma. Br Med J (Clin Res Ed) 1982 Oct 16;285(6348):1091–1093. doi: 10.1136/bmj.285.6348.1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel R., Crick R. P., Newson R. B., Shipley M., Blackmore H., Bulpitt C. J. Association between intraocular pressure and loss of visual field in chronic simple glaucoma. Br J Ophthalmol. 1990 Jan;74(1):3–6. doi: 10.1136/bjo.74.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson R., Walker A. M., Dueker D. K., Crick R. P. Risk factors for rate of progression of glaucomatous visual field loss: a computer-based analysis. Arch Ophthalmol. 1982 May;100(5):737–741. doi: 10.1001/archopht.1982.01030030741002. [DOI] [PubMed] [Google Scholar]


