Abstract
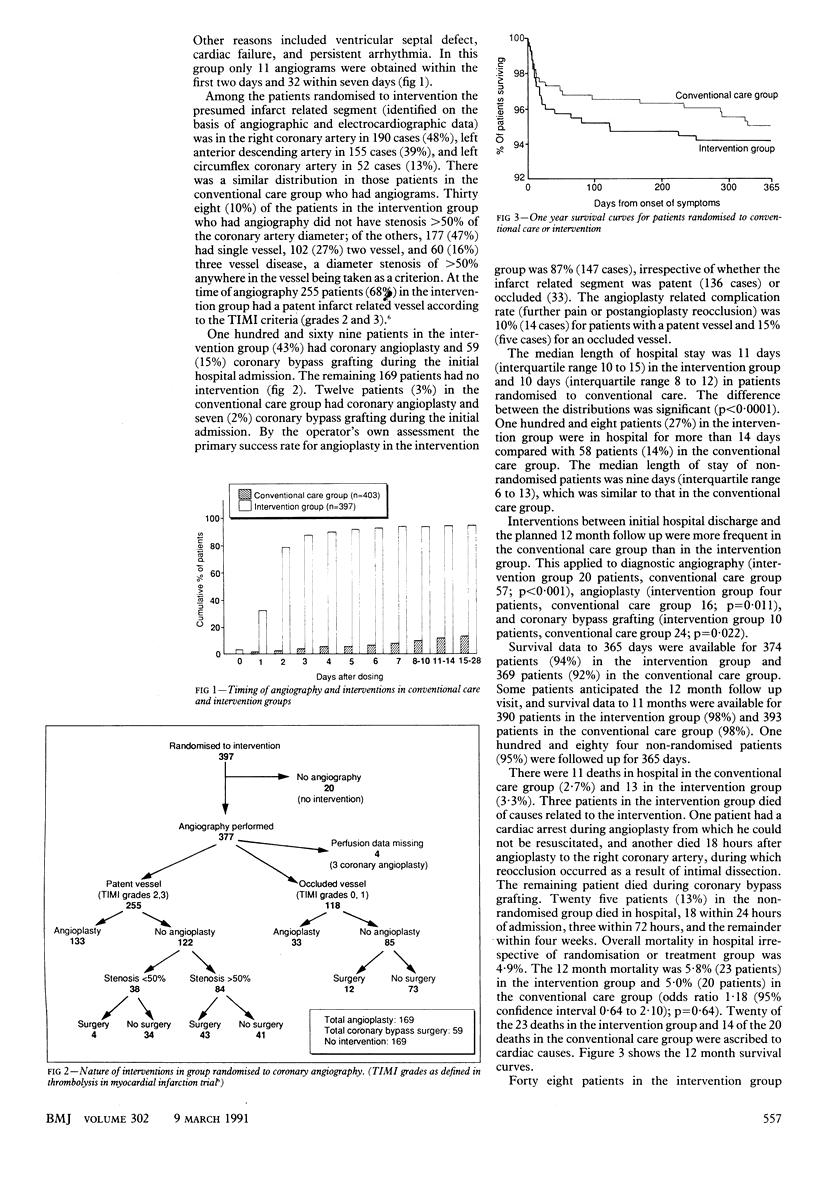
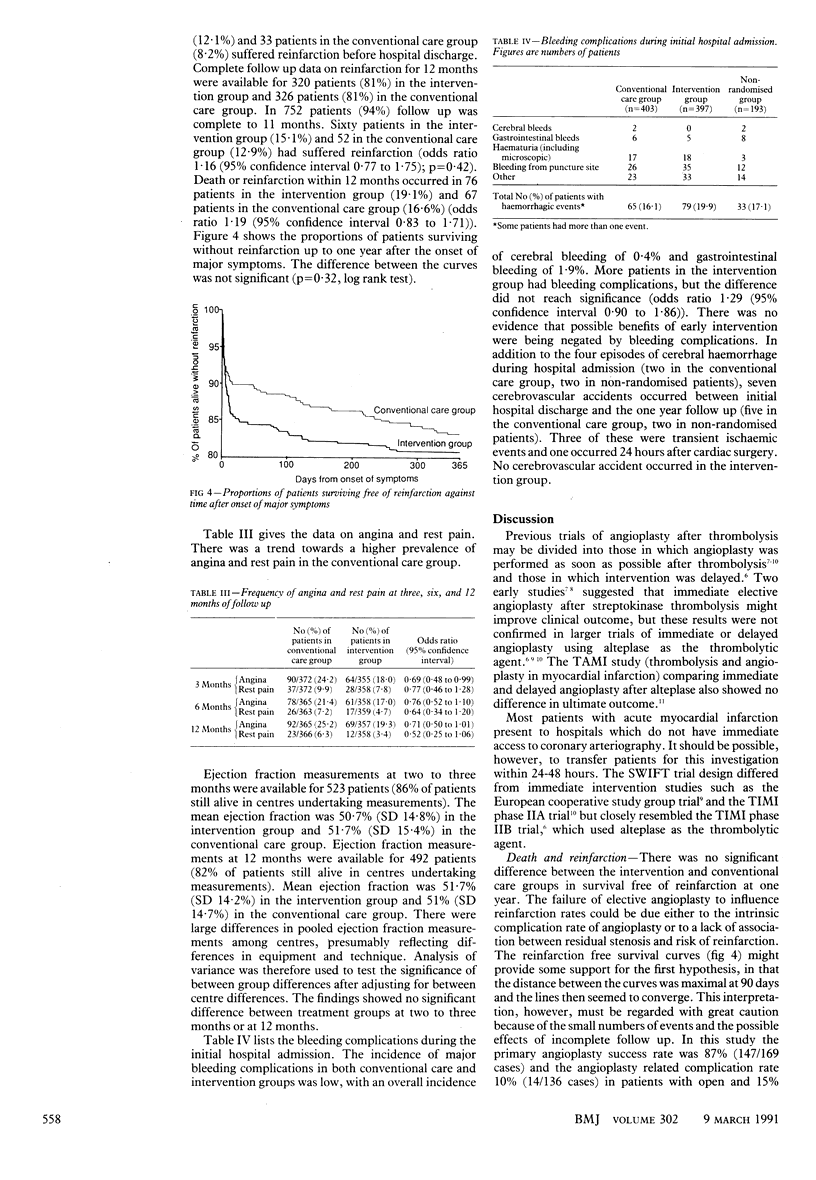
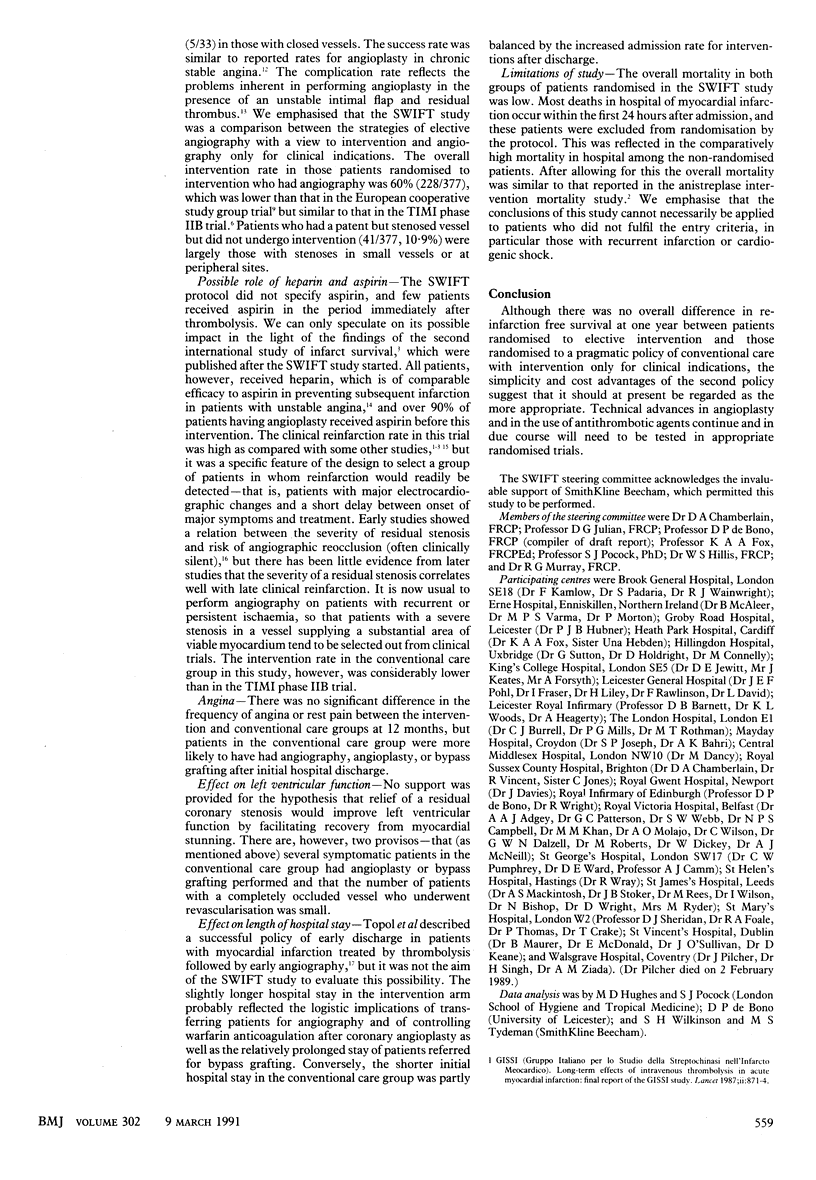
OBJECTIVE--To see whether early elective angiography with a view to coronary angioplasty or bypass grafting of a stenosed infarct related vessel would improve outcome in acute myocardial infarction treated by thrombolysis with anistreplase. DESIGN--Randomised study of two treatment strategies with analysis of results over 12 months. SETTING--21 district hospitals and regional cardiac centres in Britain and Ireland. SUBJECTS--800 of 993 patients presenting with clinical and electrocardiographic features of acute myocardial infarction up to three hours after the onset of major symptoms. TREATMENT STRATEGIES--Intravenous anistreplase 30 units followed by a standard regimen of heparin, warfarin, and timolol and (in patients so randomised) early angiography plus appropriate intervention. MAIN OUTCOME MEASURE--Death or reinfarction within 12 months. RESULTS--397 patients were randomised to receive early angiography plus appropriate intervention (coronary angioplasty in 169 cases, coronary grafting in 59) and 403 patients to receive conservative care (of these, 12 had angioplasty and seven bypass grafting during the initial admission). By 12 months mortality (5.8% (23 patients) in the intervention group v 5.0% (20) in the conservative care group; p = 0.6) and rates of reinfarction (15.1% (60 patients) v 12.9% (52); p = 0.4) were similar in the two groups. No significant differences in rates of angina or rest pain were found at 12 months. Left ventricular ejection fraction at three and 12 months was the same in both groups. Median hospital stay was longer in the intervention group (11 days v 10 days; p less than 0.0001). CONCLUSION--For most patients given thrombolytic treatment for acute myocardial infarction a strategy of angiography and intervention is appropriate only when required for clinical indications.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Düber C., Jungbluth A., Rumpelt H. J., Erbel R., Meyer J., Thoenes W. Morphology of the coronary arteries after combined thrombolysis and percutaneous transluminal coronary angioplasty for acute myocardial infarction. Am J Cardiol. 1986 Oct 1;58(9):698–703. doi: 10.1016/0002-9149(86)90340-1. [DOI] [PubMed] [Google Scholar]
- Erbel R., Pop T., Henrichs K. J., von Olshausen K., Schuster C. J., Rupprecht H. J., Steuernagel C., Meyer J. Percutaneous transluminal coronary angioplasty after thrombolytic therapy: a prospective controlled randomized trial. J Am Coll Cardiol. 1986 Sep;8(3):485–495. doi: 10.1016/s0735-1097(86)80172-3. [DOI] [PubMed] [Google Scholar]
- Harrison D. G., Ferguson D. W., Collins S. M., Skorton D. J., Ericksen E. E., Kioschos J. M., Marcus M. L., White C. W. Rethrombosis after reperfusion with streptokinase: importance of geometry of residual lesions. Circulation. 1984 May;69(5):991–999. doi: 10.1161/01.cir.69.5.991. [DOI] [PubMed] [Google Scholar]
- Papapietro S. E., MacLean W. A., Stanley A. W., Jr, Hess R. G., Corley N., Arciniegas J. G., Cooper T. B. Percutaneous transluminal coronary angioplasty after intracoronary streptokinase in evolving acute myocardial infarction. Am J Cardiol. 1985 Jan 1;55(1):48–53. doi: 10.1016/0002-9149(85)90297-8. [DOI] [PubMed] [Google Scholar]
- Perry R. A., Seth A., Hunt A., Shiu M. F. Coronary angioplasty in unstable angina and stable angina: a comparison of success and complications. Br Heart J. 1988 Nov;60(5):367–372. doi: 10.1136/hrt.60.5.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoons M. L., Arnold A. E., Betriu A., de Bono D. P., Col J., Dougherty F. C., von Essen R., Lambertz H., Lubsen J., Meier B. Thrombolysis with tissue plasminogen activator in acute myocardial infarction: no additional benefit from immediate percutaneous coronary angioplasty. Lancet. 1988 Jan 30;1(8579):197–203. doi: 10.1016/s0140-6736(88)91062-8. [DOI] [PubMed] [Google Scholar]
- Simoons M. L., Serruys P. W., vd Brand M., Bär F., de Zwaan C., Res J., Verheugt F. W., Krauss X. H., Remme W. J., Vermeer F. Improved survival after early thrombolysis in acute myocardial infarction. A randomised trial by the Interuniversity Cardiology Institute in The Netherlands. Lancet. 1985 Sep 14;2(8455):578–582. doi: 10.1016/s0140-6736(85)90584-7. [DOI] [PubMed] [Google Scholar]
- Topol E. J., Burek K., O'Neill W. W., Kewman D. G., Kander N. H., Shea M. J., Schork M. A., Kirscht J., Juni J. E., Pitt B. A randomized controlled trial of hospital discharge three days after myocardial infarction in the era of reperfusion. N Engl J Med. 1988 Apr 28;318(17):1083–1088. doi: 10.1056/NEJM198804283181702. [DOI] [PubMed] [Google Scholar]
- Topol E. J., Califf R. M., George B. S., Kereiakes D. J., Abbottsmith C. W., Candela R. J., Lee K. L., Pitt B., Stack R. S., O'Neill W. W. A randomized trial of immediate versus delayed elective angioplasty after intravenous tissue plasminogen activator in acute myocardial infarction. N Engl J Med. 1987 Sep 3;317(10):581–588. doi: 10.1056/NEJM198709033171001. [DOI] [PubMed] [Google Scholar]
- Van de Werf F., Arnold A. E. Intravenous tissue plasminogen activator and size of infarct, left ventricular function, and survival in acute myocardial infarction. BMJ. 1988 Nov 26;297(6660):1374–1379. doi: 10.1136/bmj.297.6660.1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox R. G., von der Lippe G., Olsson C. G., Jensen G., Skene A. M., Hampton J. R. Trial of tissue plasminogen activator for mortality reduction in acute myocardial infarction. Anglo-Scandinavian Study of Early Thrombolysis (ASSET). Lancet. 1988 Sep 3;2(8610):525–530. doi: 10.1016/s0140-6736(88)92656-6. [DOI] [PubMed] [Google Scholar]


