Abstract
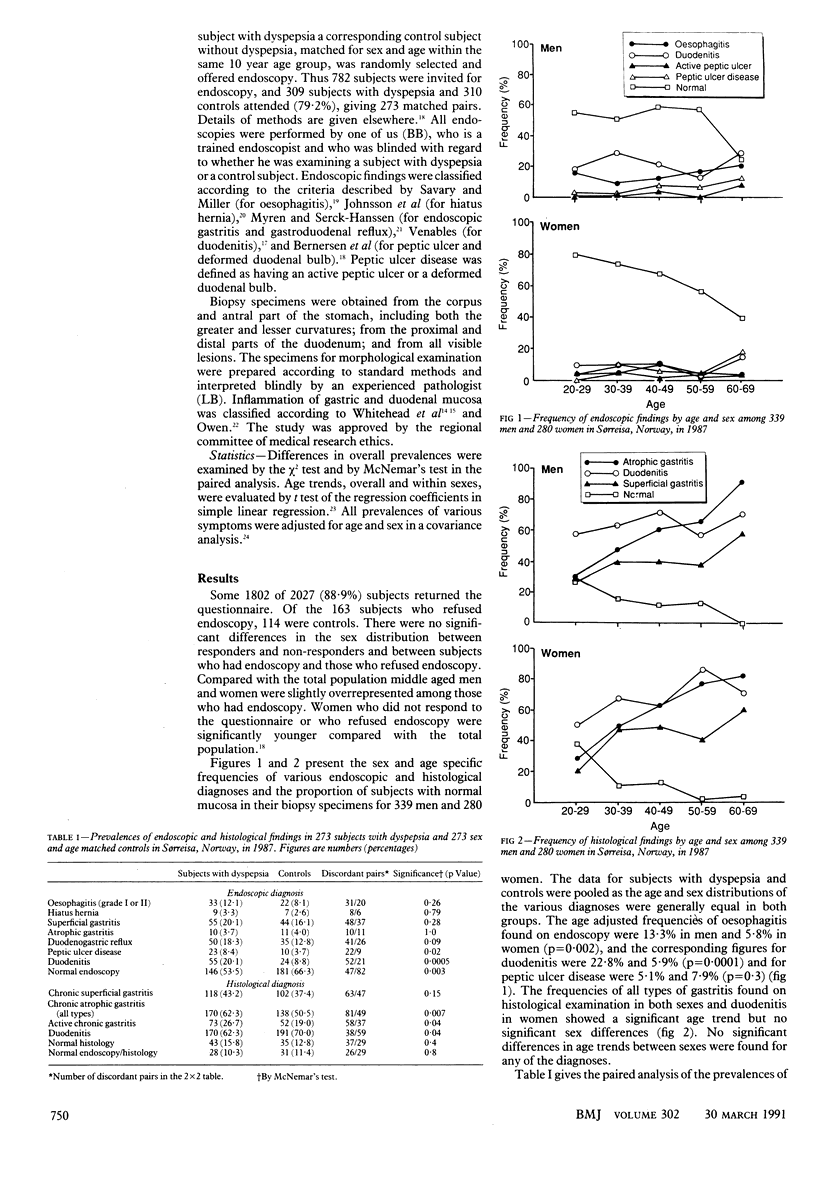
OBJECTIVE--To examine the association between dyspeptic symptoms and endoscopic and histological diagnoses. DESIGN--Cross sectional study of people with dyspepsia and controls matched for age and sex identified by questionnaire survey of all inhabitants aged 20 to 69. Endoscopy and histological examination was performed with the examiner blind to whether or not the patient had dyspepsia. SETTING--Population based survey in Sørreisa, Norway. SUBJECTS--All people with dyspepsia and age and sex matched people without dyspepsia were offered endoscopy. A total of 309 people with dyspepsia and 310 without dyspepsia underwent endoscopy, giving 273 matched pairs. MAIN OUTCOME MEASURES--Prevalences of endoscopic and histological diagnoses made according to internationally accepted standards. RESULTS--In all, 1802 of 2027 (88.9%) people returned the questionnaire. Of the 163 subjects who refused endoscopy, 114 were controls. Of five endoscopic and four histological diagnoses only peptic ulcer disease, endoscopic duodenitis, and active chronic gastritis were diagnosed significantly more often in people with dyspepsia. In all, 30% to 50% of the diagnoses of mucosal inflammation and peptic ulcer disease were made among subjects without dyspepsia, and only 10% of both those with and those without dyspepsia had normal endoscopic findings. CONCLUSIONS--The diagnostic findings, with possible exceptions of peptic ulcer disease and endoscopic duodenitis, showed no association of clinical value with dyspeptic symptoms. The small number of "normal" endoscopic findings in both those with and those without dyspepsia challenge well accepted endoscopic and histological diagnostic criteria with relation to the upper gastrointestinal tract.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Akdamar K., Ertan A., Agrawal N. M., McMahon F. G., Ryan J. Upper gastrointestinal endoscopy in normal asymptomatic volunteers. Gastrointest Endosc. 1986 Apr;32(2):78–80. doi: 10.1016/s0016-5107(86)71760-4. [DOI] [PubMed] [Google Scholar]
- Barbara L., Camilleri M., Corinaldesi R., Crean G. P., Heading R. C., Johnson A. G., Malagelada J. R., Stanghellini V., Wienbeck M. Definition and investigation of dyspepsia. Consensus of an international ad hoc working party. Dig Dis Sci. 1989 Aug;34(8):1272–1276. doi: 10.1007/BF01537277. [DOI] [PubMed] [Google Scholar]
- Bernersen B., Johnsen R., Straume B., Burhol P. G., Jenssen T. G., Stakkevold P. A. Towards a true prevalence of peptic ulcer: the Sørreisa gastrointestinal disorder study. Gut. 1990 Sep;31(9):989–992. doi: 10.1136/gut.31.9.989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheli R., Giacosa A. Duodenal ulcer and chronic gastritis. Endoscopy. 1986 Jul;18(4):125–126. doi: 10.1055/s-2007-1018350. [DOI] [PubMed] [Google Scholar]
- Cheli R. Symptoms in chronic non-specific duodenitis. Scand J Gastroenterol Suppl. 1982;79:84–87. [PubMed] [Google Scholar]
- Danielsson A., Ek B., Nyhlin H., Steen L. The relationship between active peptic ulcer, endoscopic duodenitis and symptomatic state after treatment with cimetidine. Ann Clin Res. 1980 Feb;12(1):4–12. [PubMed] [Google Scholar]
- DeLuca V. A., Jr, Winnan G. G., Sheahan D. G., Sanders F. J., Jr, Greenlaw R., Marignani P., Gorelick F. S., Bhalotra R., Goldblatt R. S. Is gastroduodenitis part of the spectrum of peptic ulcer disease? J Clin Gastroenterol. 1981;3(Suppl 2):17–22. [PubMed] [Google Scholar]
- Earlam R. J., Amerigo J., Kakavoulis T., Pollock D. J. Histological appearances of oesophagus, antrum and duodenum and their correlation with symptoms in patients with a duodenal ulcer. Gut. 1985 Jan;26(1):95–100. doi: 10.1136/gut.26.1.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenlaw R., Sheahan D. G., DeLuca V., Miller D., Myerson D., Myerson P. Gastroduodenitis. A broader concept of peptic ulcer disease. Dig Dis Sci. 1980 Sep;25(9):660–672. doi: 10.1007/BF01308325. [DOI] [PubMed] [Google Scholar]
- Guslandi M. Focus on duodenitis. Dig Dis. 1986;4(4):231–239. doi: 10.1159/000171153. [DOI] [PubMed] [Google Scholar]
- Joffe S. N. Relevance of duodenitis to non-ulcer dyspepsia and peptic ulceration. Scand J Gastroenterol Suppl. 1982;79:88–97. [PubMed] [Google Scholar]
- Johnsson F., Joelsson B., Gudmundsson K., Greiff L. Symptoms and endoscopic findings in the diagnosis of gastroesophageal reflux disease. Scand J Gastroenterol. 1987 Aug;22(6):714–718. doi: 10.3109/00365528709011148. [DOI] [PubMed] [Google Scholar]
- Kreuning J., Bosman F. T., Kuiper G., Wal A. M., Lindeman J. Gastric and duodenal mucosa in 'healthy' individuals. An endoscopic and histopathological study of 50 volunteers. J Clin Pathol. 1978 Jan;31(1):69–77. doi: 10.1136/jcp.31.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon M., Willing R. L., Whitehead R. Cimetidine in the management of symptomatic patients with duodenitis: a double-blind controlled trial. Dig Dis Sci. 1982 Mar;27(3):217–219. doi: 10.1007/BF01296918. [DOI] [PubMed] [Google Scholar]
- Management of dyspepsia: report of a working party. Lancet. 1988 Mar 12;1(8585):576–579. [PubMed] [Google Scholar]
- Myren J., Serck-Hanssen A. The gastroscopic diagnosis of gastritis with particular reference to mucosal reddening and mucus covering. Scand J Gastroenterol. 1974;9(5):457–462. [PubMed] [Google Scholar]
- Sircus W. Duodenitis: a clinical, endoscopic and histopathologic study. Q J Med. 1985 Sep;56(221):593–600. [PubMed] [Google Scholar]
- Siurala M., Varis K., Kekki M. New aspects on epidemiology, genetics, and dynamics of chronic gastritis. Front Gastrointest Res. 1980;6:148–166. doi: 10.1159/000403329. [DOI] [PubMed] [Google Scholar]
- Spiro H. M. Visceral viewpoints. Moynihan's disease? The diagnosis of duodenal ulcer. N Engl J Med. 1974 Sep 12;291(11):567–569. doi: 10.1056/NEJM197409122911107. [DOI] [PubMed] [Google Scholar]
- Talley N. J., Phillips S. F. Non-ulcer dyspepsia: potential causes and pathophysiology. Ann Intern Med. 1988 Jun;108(6):865–879. doi: 10.7326/0003-4819-108-6-865. [DOI] [PubMed] [Google Scholar]
- Thomson W. O., Joffe S. N., Robertson A. G., Lee F. D., Imrie C. W., Blumgart L. H. Is duodenitis a dyspeptic myth? Lancet. 1977 Jun 4;1(8023):1197–1198. doi: 10.1016/s0140-6736(77)92729-5. [DOI] [PubMed] [Google Scholar]
- Villako K., Ihamäki T., Tamm A., Tammur R. Upper abdominal complaints and gastritis. Ann Clin Res. 1984;16(4):192–194. [PubMed] [Google Scholar]
- Villako K., Tamm A., Savisaar E., Ruttas M. Prevalence of antral and fundic gastritis in a randomly selected group of an Estonian rural population. Scand J Gastroenterol. 1976;11(8):817–822. [PubMed] [Google Scholar]
- Whitehead R., Roca M., Meikle D. D., Skinner J., Truelove S. C. The histological classification of duodenitis in fibreoptic biopsy specimens. Digestion. 1975;13(3):129–136. doi: 10.1159/000197701. [DOI] [PubMed] [Google Scholar]
- Whitehead R., Truelove S. C., Gear M. W. The histological diagnosis of chronic gastritis in fibreoptic gastroscope biopsy specimens. J Clin Pathol. 1972 Jan;25(1):1–11. doi: 10.1136/jcp.25.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


