Abstract
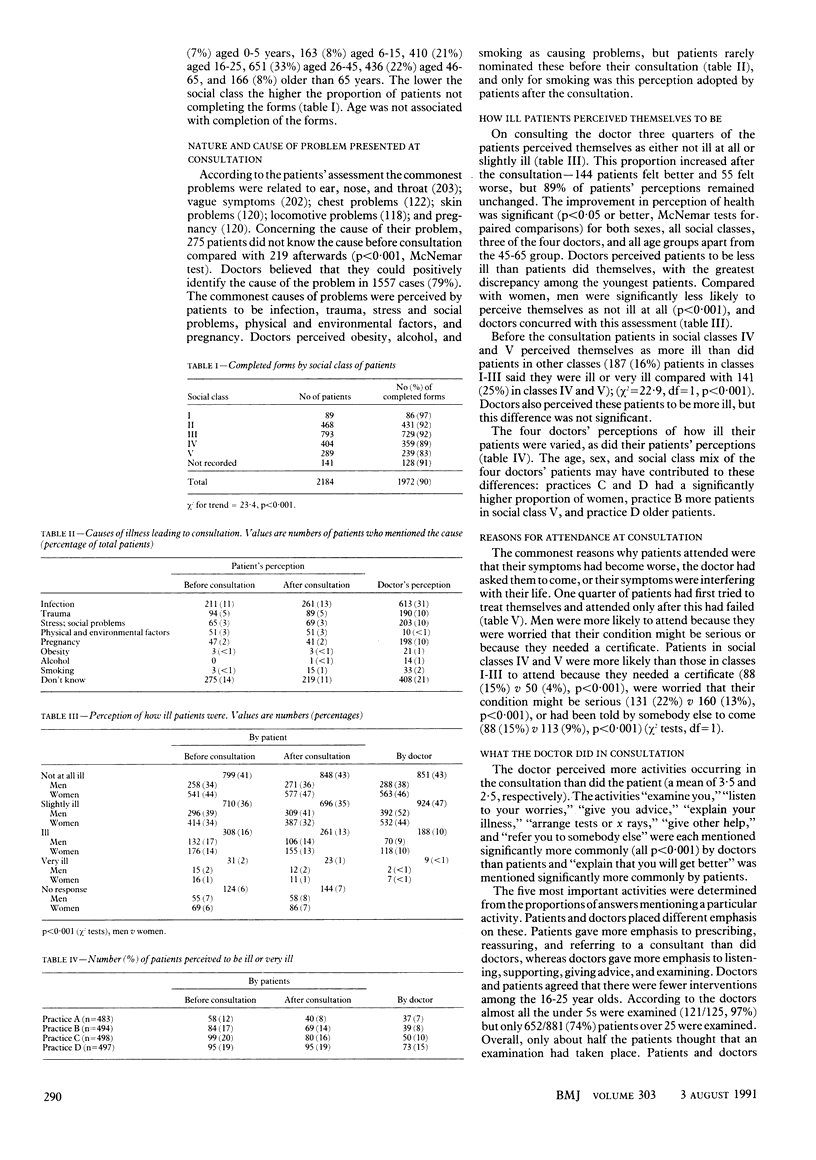
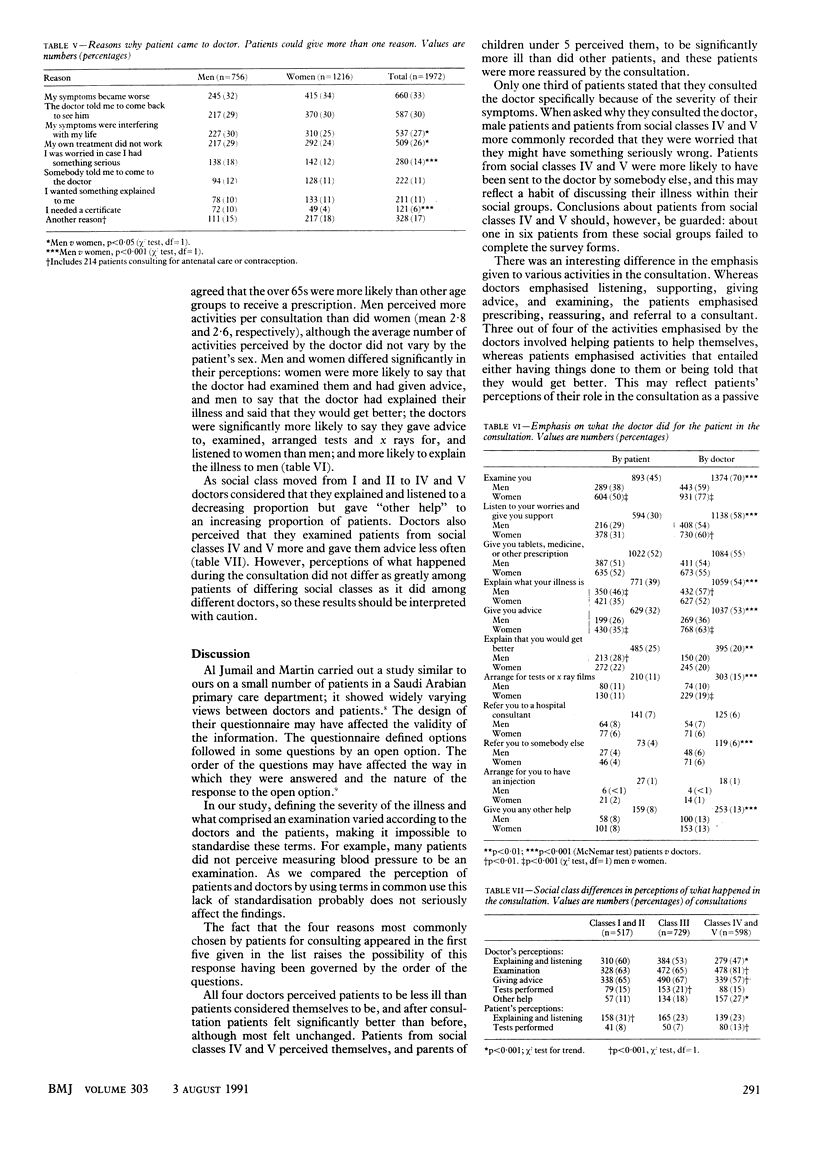
OBJECTIVE--To study patients' perceptions of why they consulted the doctor, how ill they thought they were, and what happened in the consultation. To compare patients' perceptions before and after the consultation and to compare these perceptions with those of the doctor. DESIGN--Patients filled in a questionnaire before and after the consultation. The doctor filled a questionnaire in after the consultation. SETTING--Three general practices in Bedfordshire and one in Hertfordshire. PATIENTS--500 consecutive patients consulting in each practice. MAIN OUTCOME MEASURES--Changes in patients' perceptions and differences between the perceptions of patients and doctors. RESULTS--Doctors perceived patients to be less ill than the patients themselves did. Patients from social classes IV and V and children perceived themselves to be more ill than the average. Patients perceived themselves to be less ill after the consultation. A third of patients attended because doctors had told them to, and a quarter of patients had already tried to treat their problem themselves when they attended the consultation. Doctors' perceptions of the consultation emphasised listening, supporting, and giving advice. Patients' perceptions emphasised prescribing, reassuring, and referring to a consultant. Doctors perceived that they listened, examined, and gave advice less to social classes IV and V than to social classes I, II, and III and gave explanations more often to men than to women. Patients perceived external factors rather than lifestyle factors as being more important in causing their problems. CONCLUSION--Doctors' perceptions of patients' problems differed from those of patients expressed both before and after their consultation. Doctors' and patients' perceptions also differed about the consultation itself. The consultation reassured some patients.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brett A. S., Mathieu A. E. Perceptions and behaviors of patients with upper respiratory tract infection. J Fam Pract. 1982 Aug;15(2):277–279. [PubMed] [Google Scholar]
- Coulter A. Lifestyles and social class: implications for primary care. J R Coll Gen Pract. 1987 Dec;37(305):533–536. [PMC free article] [PubMed] [Google Scholar]
- Johnson S. M., Snow L. F., Mayhew H. E. Limited patient knowledge as a reproductive risk factor. J Fam Pract. 1978 Apr;6(4):855–862. [PubMed] [Google Scholar]
- Johnson S. S. Health beliefs of hypertensive patients in a family medicine residency program. J Fam Pract. 1979 Nov;9(5):877–883. [PubMed] [Google Scholar]
- McWhinney I. R. Changing models: the impact of Kuhn's theory on medicine. Fam Pract. 1984 Mar;1(1):3–8. doi: 10.1093/fampra/1.1.3. [DOI] [PubMed] [Google Scholar]
- Stewart M. A., McWhinney I. R., Buck C. W. How illness presents: a study of patient behavior. J Fam Pract. 1975 Dec;2(6):411–414. [PubMed] [Google Scholar]
- Walker R. D. Knowledge of symptoms suggesting malignant disease amongst general practice patients. J R Coll Gen Pract. 1982 Mar;32(236):163–166. [PMC free article] [PubMed] [Google Scholar]
- Zola I. K. Pathways to the doctor-from person to patient. Soc Sci Med. 1973 Sep;7(9):677–689. doi: 10.1016/0037-7856(73)90002-4. [DOI] [PubMed] [Google Scholar]


