Abstract
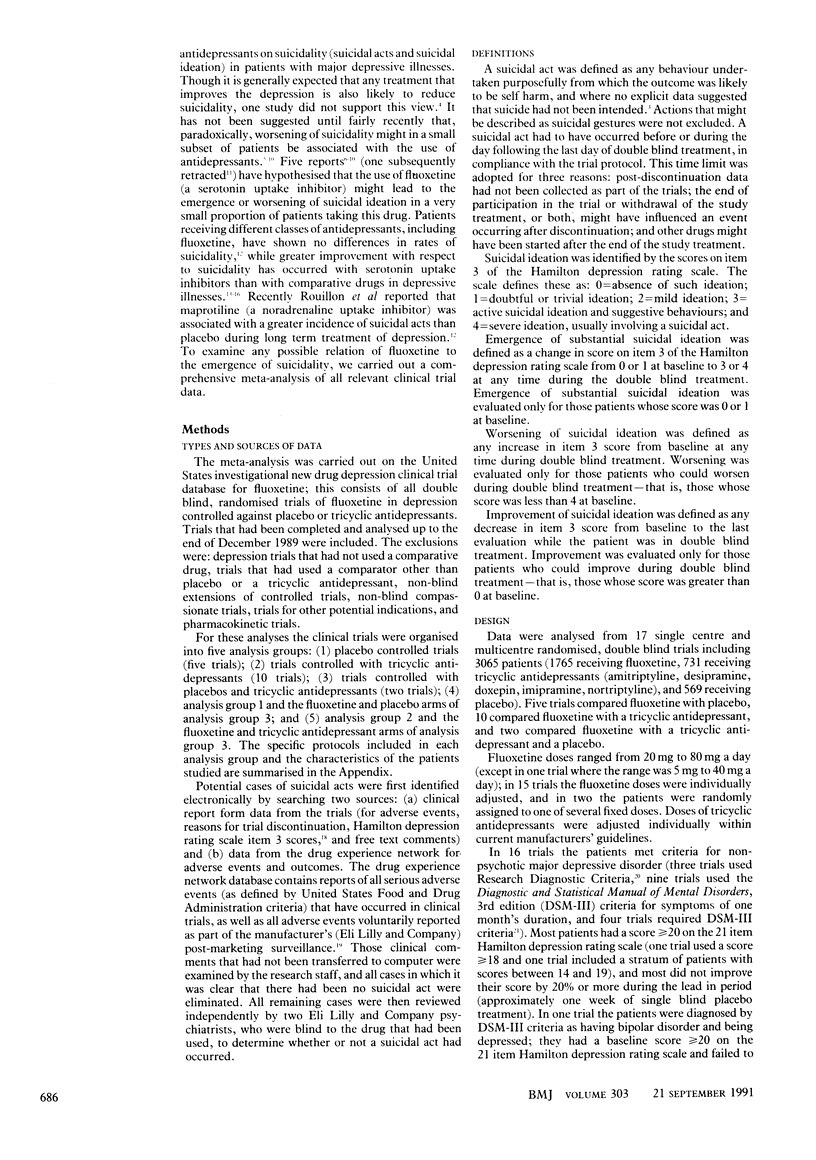
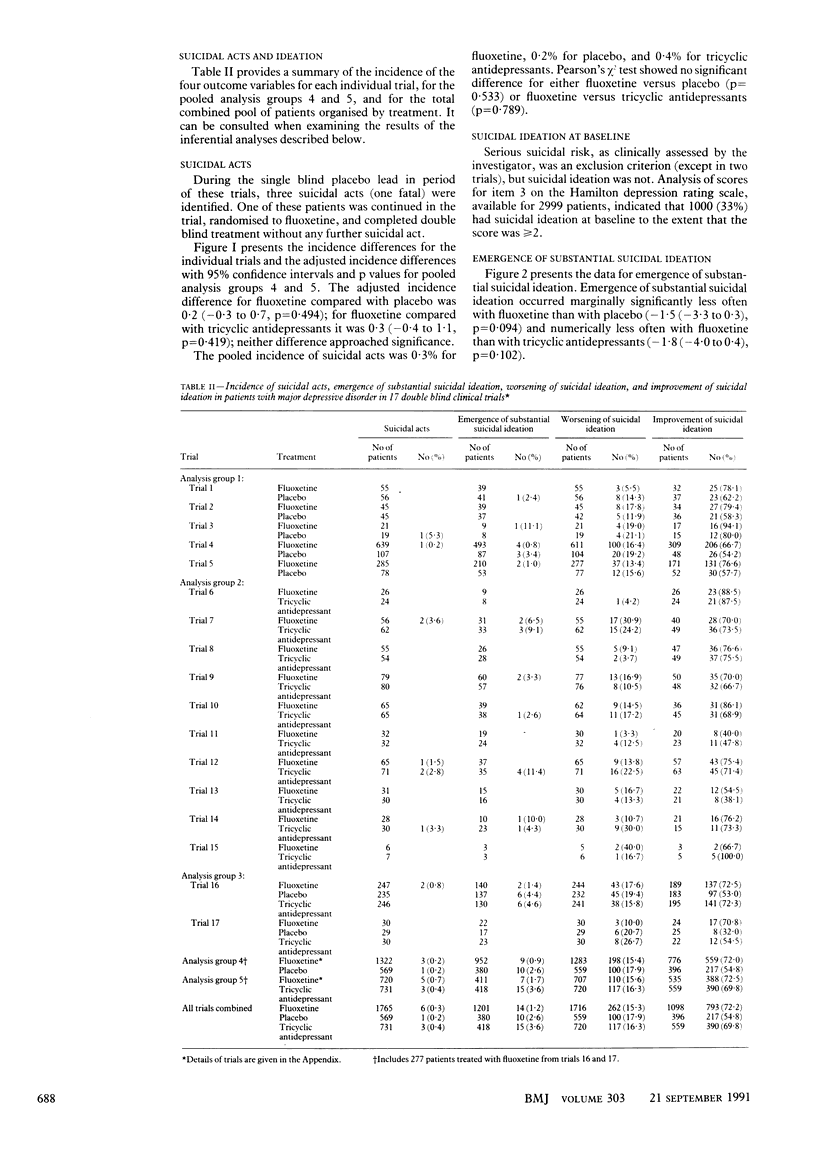
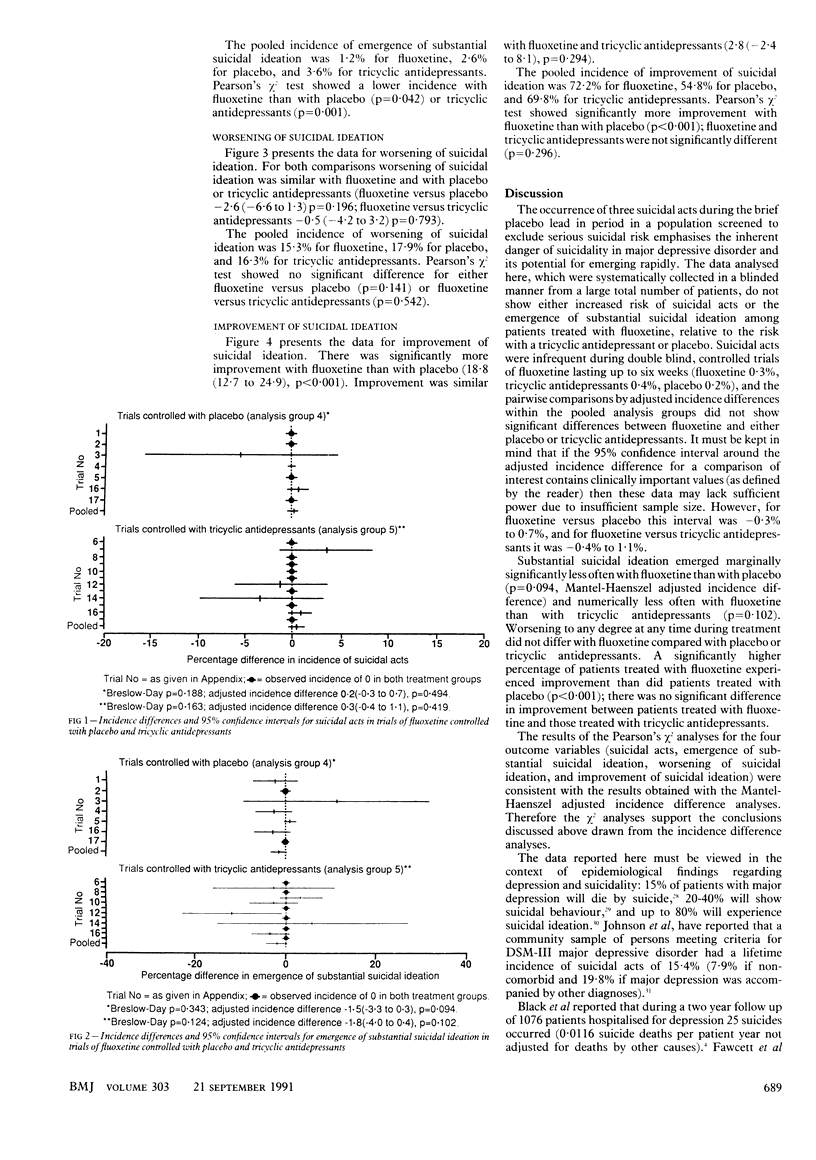
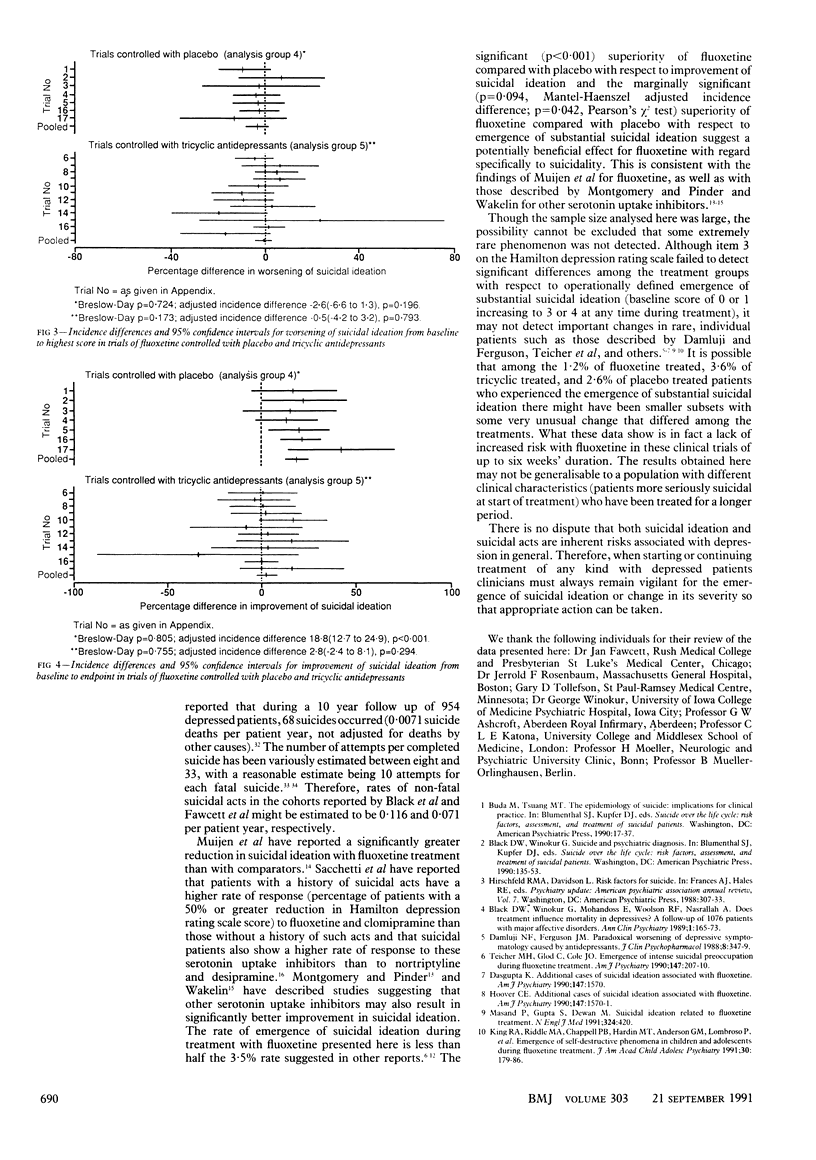
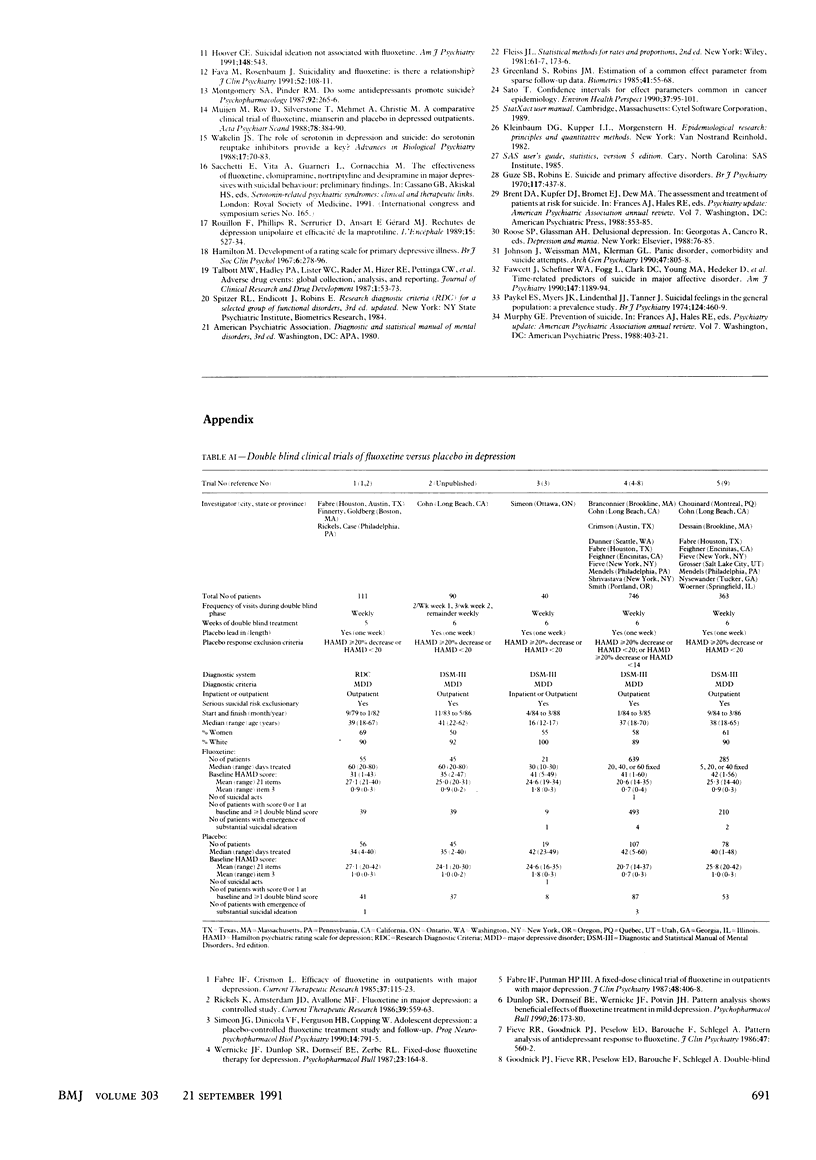
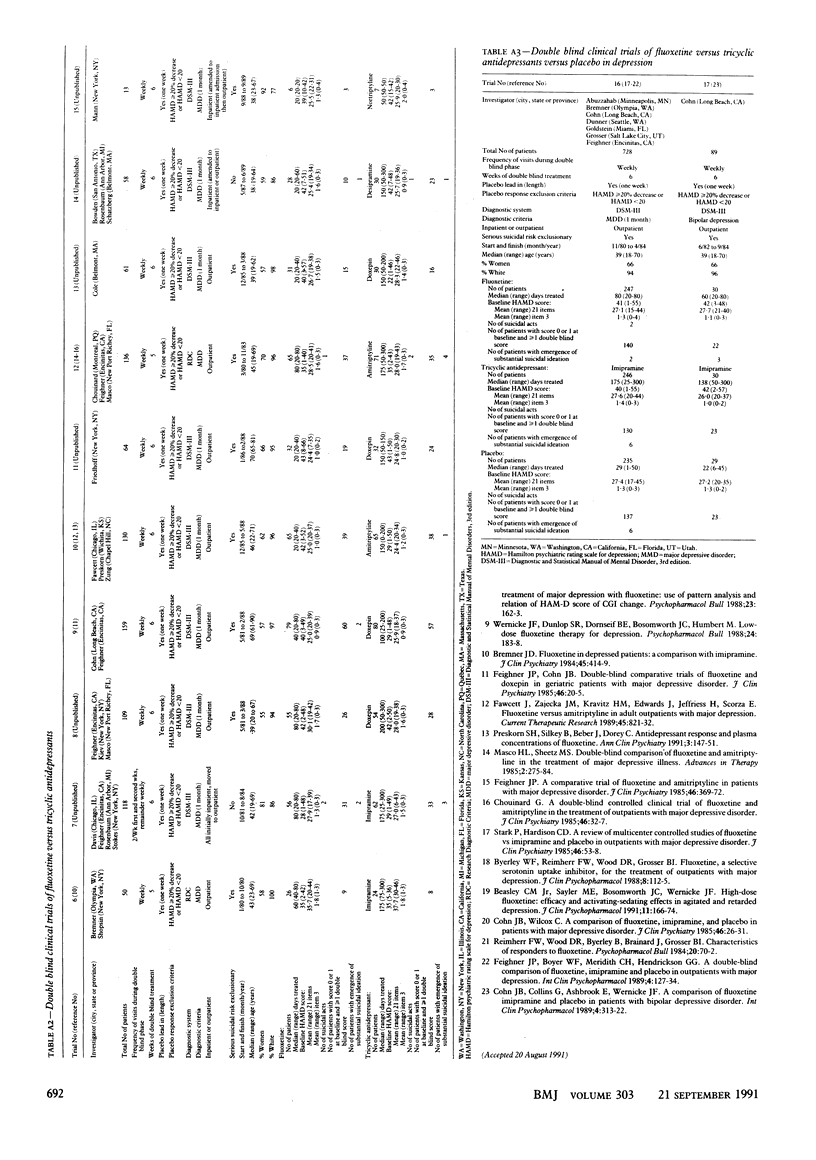
OBJECTIVE--A comprehensive meta-analysis of clinical trial data was performed to assess the possible association of fluoxetine and suicidality (suicidal acts and ideation). DESIGN--Retrospective analysis of pooled data from 17 double blind clinical trials in patients with major depressive disorder comparing fluoxetine (n = 1765) with a tricyclic antidepressant (n = 731) or placebo (n = 569), or both. MAIN OUTCOME MEASURES--Multiple data sources were searched to identify patients with suicidal acts. Suicidal ideation was assessed with item 3 of the Hamilton depression rating scale, which systematically rates suicidality. Emergence of substantial suicidal ideation was defined as a change in the rating of this item from 0 or 1 at baseline to 3 or 4 during double blind treatment; worsening was defined as any increase from baseline; improvement was defined as a decrease from baseline at the last visit during the treatment. RESULTS--Suicidal acts did not differ significantly in comparisons of fluoxetine with placebo (0.2% v 0.2%, p = 0.494, Mantel-Haenszel adjusted incidence difference) and with tricyclic antidepressants (0.7% v 0.4%, p = 0.419). The pooled incidence of suicidal acts was 0.3% for fluoxetine, 0.2% for placebo, and 0.4% for tricyclic antidepressants, and fluoxetine did not differ significantly from either placebo (p = 0.533, Pearson's chi 2) or tricyclic antidepressants (p = 0.789). Suicidal ideation emerged marginally significantly less often with fluoxetine than with placebo (0.9% v 2.6%, p = 0.094) and numerically less often than with tricyclic antidepressants (1.7% v 3.6%, p = 0.102). The pooled incidence of emergence of substantial suicidal ideation was 1.2% for fluoxetine, 2.6% for placebo, and 3.6% for tricyclic antidepressants. The incidence was significantly lower with fluoxetine than with placebo (p = 0.042) and tricyclic antidepressants (p = 0.001). Any degree of worsening of suicidal ideation was similar with fluoxetine and placebo (15.4% v 17.9%, p = 0.196) and with fluoxetine and tricyclic antidepressants (15.6% v 16.3%, p = 0.793). The pooled incidence of worsening of suicidal ideation was 15.3% for fluoxetine, 17.9% for placebo, and 16.3% for tricyclic antidepressants. The incidence did not differ significantly with fluoxetine and placebo (p = 0.141) or tricyclic antidepressants (p = 0.542). Suicidal ideation improved significantly more with fluoxetine than with placebo (72.0% v 54.8%, p less than 0.001) and was similar to the improvement with tricyclic antidepressants (72.5% v 69.8%, p = 0.294). The pooled incidence of improvement of suicidal ideation was 72.2% for fluoxetine, 54.8% for placebo, and 69.8% for tricyclic antidepressants. The incidence with fluoxetine was significantly greater than with placebo (p less than 0.001) and did not differ from that with tricyclic antidepressants (p = 0.296). CONCLUSIONS--Data from these trials do not show that fluoxetine is associated with an increased risk of suicidal acts or emergence of substantial suicidal thoughts among depressed patients.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beasley C. M., Jr, Sayler M. E., Bosomworth J. C., Wernicke J. F. High-dose fluoxetine: efficacy and activating-sedating effects in agitated and retarded depression. J Clin Psychopharmacol. 1991 Jun;11(3):166–174. [PubMed] [Google Scholar]
- Bremner J. D. Fluoxetine in depressed patients: a comparison with imipramine. J Clin Psychiatry. 1984 Oct;45(10):414–419. [PubMed] [Google Scholar]
- Byerley W. F., Reimherr F. W., Wood D. R., Grosser B. I. Fluoxetine, a selective serotonin uptake inhibitor, for the treatment of outpatients with major depression. J Clin Psychopharmacol. 1988 Apr;8(2):112–115. [PubMed] [Google Scholar]
- Chouinard G. A double-blind controlled clinical trial of fluoxetine and amitriptyline in the treatment of outpatients with major depressive disorder. J Clin Psychiatry. 1985 Mar;46(3 Pt 2):32–37. [PubMed] [Google Scholar]
- Cohn J. B., Collins G., Ashbrook E., Wernicke J. F. A comparison of fluoxetine imipramine and placebo in patients with bipolar depressive disorder. Int Clin Psychopharmacol. 1989 Oct;4(4):313–322. doi: 10.1097/00004850-198910000-00006. [DOI] [PubMed] [Google Scholar]
- Cohn J. B., Wilcox C. A comparison of fluoxetine, imipramine, and placebo in patients with major depressive disorder. J Clin Psychiatry. 1985 Mar;46(3 Pt 2):26–31. [PubMed] [Google Scholar]
- Damluji N. F., Ferguson J. M. Paradoxical worsening of depressive symptomatology caused by antidepressants. J Clin Psychopharmacol. 1988 Oct;8(5):347–349. [PubMed] [Google Scholar]
- Dunlop S. R., Dornseif B. E., Wernicke J. F., Potvin J. H. Pattern analysis shows beneficial effect of fluoxetine treatment in mild depression. Psychopharmacol Bull. 1990;26(2):173–180. [PubMed] [Google Scholar]
- Fabre L. F., Putman H. P., 3rd A fixed-dose clinical trial of fluoxetine in outpatients with major depression. J Clin Psychiatry. 1987 Oct;48(10):406–408. [PubMed] [Google Scholar]
- Fava M., Rosenbaum J. F. Suicidality and fluoxetine: is there a relationship? J Clin Psychiatry. 1991 Mar;52(3):108–111. [PubMed] [Google Scholar]
- Fawcett J., Scheftner W. A., Fogg L., Clark D. C., Young M. A., Hedeker D., Gibbons R. Time-related predictors of suicide in major affective disorder. Am J Psychiatry. 1990 Sep;147(9):1189–1194. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- Feighner J. P. A comparative trial of fluoxetine and amitriptyline in patients with major depressive disorder. J Clin Psychiatry. 1985 Sep;46(9):369–372. [PubMed] [Google Scholar]
- Feighner J. P., Boyer W. F., Merideth C. H., Hendrickson G. G. A double-blind comparison of fluoxetine, imipramine and placebo in outpatients with major depression. Int Clin Psychopharmacol. 1989 Apr;4(2):127–134. doi: 10.1097/00004850-198904000-00004. [DOI] [PubMed] [Google Scholar]
- Feighner J. P., Cohn J. B. Double-blind comparative trials of fluoxetine and doxepin in geriatric patients with major depressive disorder. J Clin Psychiatry. 1985 Mar;46(3 Pt 2):20–25. [PubMed] [Google Scholar]
- Fieve R. R., Goodnick P. J., Peselow E. D., Barouche F., Schlegel A. Pattern analysis of antidepressant response to fluoxetine. J Clin Psychiatry. 1986 Nov;47(11):560–562. [PubMed] [Google Scholar]
- Guze S. B., Robins E. Suicide and primary affective disorders. Br J Psychiatry. 1970 Oct;117(539):437–438. doi: 10.1192/bjp.117.539.437. [DOI] [PubMed] [Google Scholar]
- Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967 Dec;6(4):278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- Hoover C. E. Suicidal ideation not associated with fluoxetine. Am J Psychiatry. 1991 Apr;148(4):543–543. doi: 10.1176/ajp.148.4.543a. [DOI] [PubMed] [Google Scholar]
- Johnson J., Weissman M. M., Klerman G. L. Panic disorder, comorbidity, and suicide attempts. Arch Gen Psychiatry. 1990 Sep;47(9):805–808. doi: 10.1001/archpsyc.1990.01810210013002. [DOI] [PubMed] [Google Scholar]
- King R. A., Riddle M. A., Chappell P. B., Hardin M. T., Anderson G. M., Lombroso P., Scahill L. Emergence of self-destructive phenomena in children and adolescents during fluoxetine treatment. J Am Acad Child Adolesc Psychiatry. 1991 Mar;30(2):179–186. doi: 10.1097/00004583-199103000-00003. [DOI] [PubMed] [Google Scholar]
- Montgomery S. A., Pinder R. M. Do some antidepressants promote suicide? Psychopharmacology (Berl) 1987;92(2):265–266. doi: 10.1007/BF00177927. [DOI] [PubMed] [Google Scholar]
- Muijen M., Roy D., Silverstone T., Mehmet A., Christie M. A comparative clinical trial of fluoxetine, mianserin and placebo in depressed outpatients. Acta Psychiatr Scand. 1988 Sep;78(3):384–390. doi: 10.1111/j.1600-0447.1988.tb06353.x. [DOI] [PubMed] [Google Scholar]
- Paykel E. S., Myers J. K., Lindenthal J. J., Tanner J. Suicidal feelings in the general population: a prevalence study. Br J Psychiatry. 1974 May;124(0):460–469. doi: 10.1192/bjp.124.5.460. [DOI] [PubMed] [Google Scholar]
- Reimherr F. W., Wood D. R., Byerley B., Brainard J., Grosser B. I. Characteristics of responders to fluoxetine. Psychopharmacol Bull. 1984 Winter;20(1):70–72. [PubMed] [Google Scholar]
- Rouillon F., Phillips R., Serrurier D., Ansart E., Gérard M. J. Rechutes de dépression unipolaire et efficacité de la maprotiline. Encephale. 1989 Nov-Dec;15(6):527–534. [PubMed] [Google Scholar]
- Simeon J. G., Dinicola V. F., Ferguson H. B., Copping W. Adolescent depression: a placebo-controlled fluoxetine treatment study and follow-up. Prog Neuropsychopharmacol Biol Psychiatry. 1990;14(5):791–795. doi: 10.1016/0278-5846(90)90050-q. [DOI] [PubMed] [Google Scholar]
- Teicher M. H., Glod C., Cole J. O. Emergence of intense suicidal preoccupation during fluoxetine treatment. Am J Psychiatry. 1990 Feb;147(2):207–210. doi: 10.1176/ajp.147.2.207. [DOI] [PubMed] [Google Scholar]
- Wernicke J. F., Dunlop S. R., Dornseif B. E., Bosomworth J. C., Humbert M. Low-dose fluoxetine therapy for depression. Psychopharmacol Bull. 1988;24(1):183–188. [PubMed] [Google Scholar]



