Abstract
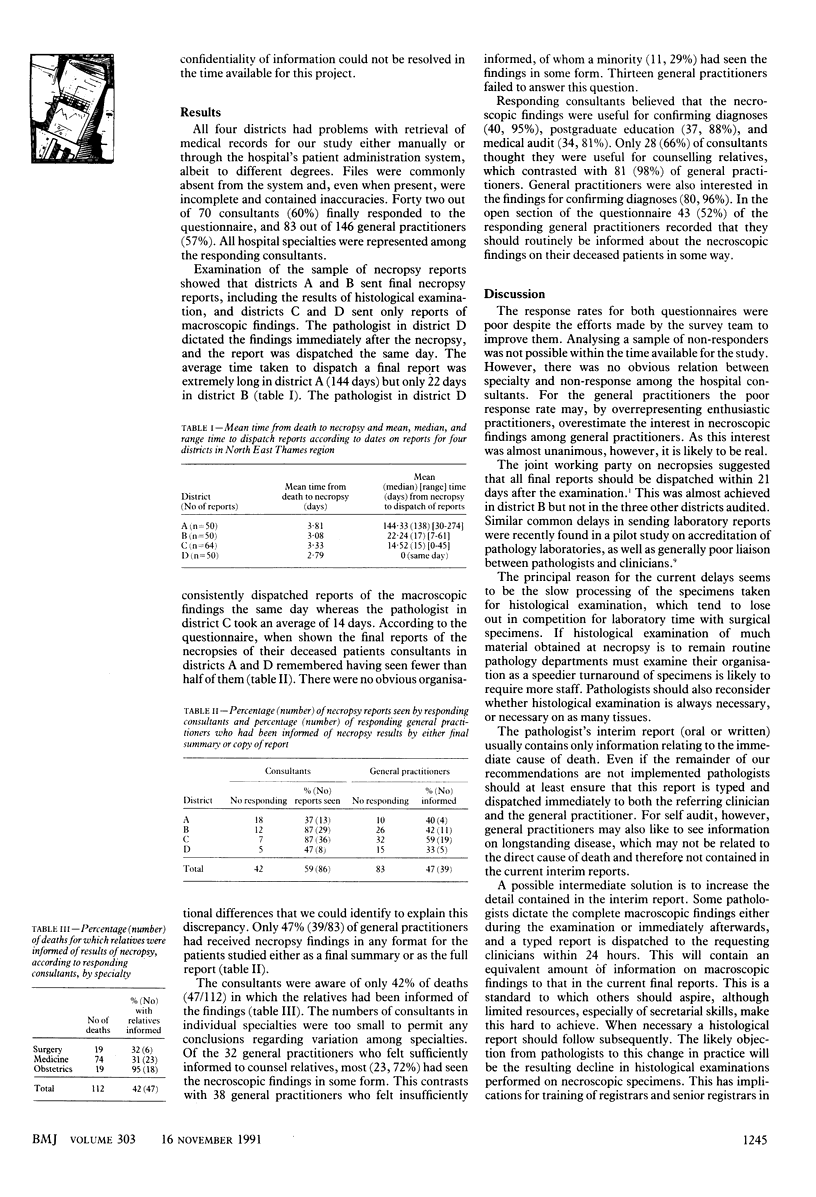
OBJECTIVE--To evaluate the adequacy of reporting of results of necropsy to referring clinicians and to general practitioners. DESIGN--Questionnaire survey of referring clinicians and general practitioners of deceased patients in four districts in North East Thames region. Patients were selected by retrospective systematic sampling of 50 or more necropsy reports in each district. SETTING--One teaching hospital, one inner London district general hospital, and two outer London district general hospitals. PARTICIPANTS--70 consultants and 146 general practitioners who were asked about 214 necropsy reports; coroners' reports were excluded. MAIN OUTCOME MEASURES--Time taken for dispatch of final reports after necropsy, consultants' recognition of the reports, general practitioners' recognition of the reports or of their findings, and consultants' recall of having discussed the findings with relatives. RESULTS--Only two hospitals dispatched final reports including histological findings (mean time to dispatch 144 days and 22 days respectively). 42 (60%) consultants and 83 (57%) general practitioners responded to the survey. The percentage of reports seen by consultants varied from 37% (n = 13) to 87% (n = 36); in all, only 47% (39/83) of general practitioners had been informed of the findings by any method. Consultants could recall having discussed findings with only 42% (47/112) of relatives. CONCLUSIONS--Communication of results of necropsies to hospital clinicians, general practitioners, and relatives is currently inadequate in these hospitals. IMPLICATIONS AND ACTION--A report of the macroscopic findings should be dispatched immediately after necropsy to clinicians and general practitioners; relatives should routinely be invited to discuss the necroscopic findings. One department has already altered its practice.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brown H. G. Lay perceptions of autopsy. Arch Pathol Lab Med. 1984 Jun;108(6):446–448. [PubMed] [Google Scholar]
- Chana J., Rhys-Maitland R., Hon P., Scott P., Thomas C., Hopkins A. Who asks permission for an autopsy? J R Coll Physicians Lond. 1990 Jul;24(3):185–188. [PMC free article] [PubMed] [Google Scholar]
- Friederici H. H. Reflections on the postmortem audit. JAMA. 1988 Dec 16;260(23):3461–3465. [PubMed] [Google Scholar]
- Goldman L., Sayson R., Robbins S., Cohn L. H., Bettmann M., Weisberg M. The value of the autopsy in three medical eras. N Engl J Med. 1983 Apr 28;308(17):1000–1005. doi: 10.1056/NEJM198304283081704. [DOI] [PubMed] [Google Scholar]
- Neville R. G. Notifying general practitioners about deaths in hospital: an audit. J R Coll Gen Pract. 1987 Nov;37(304):496–497. [PMC free article] [PubMed] [Google Scholar]
- Schned A. R., Mogielnicki R. P., Stauffer M. E. A comprehensive quality assessment program on the autopsy service. Am J Clin Pathol. 1986 Aug;86(2):133–138. doi: 10.1093/ajcp/86.2.133. [DOI] [PubMed] [Google Scholar]
- Underwood J. C., Cotton D. W., Stephenson T. J. Audit and necropsy. Lancet. 1989 Feb 25;1(8635):442–442. doi: 10.1016/s0140-6736(89)90039-1. [DOI] [PubMed] [Google Scholar]


