Abstract
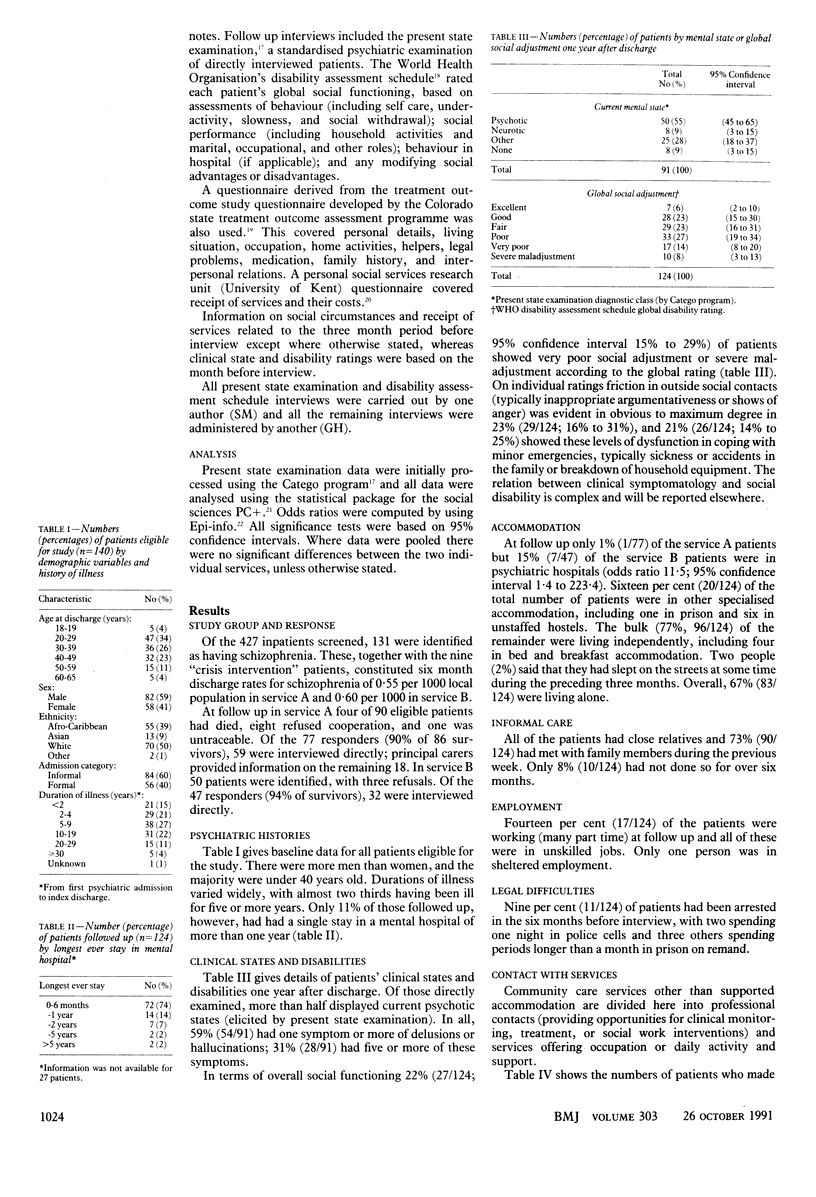
OBJECTIVES--To document the circumstances and care of patients with schizophrenia who had recently been discharged from local psychiatric inpatient services, and to establish the extent to which misgivings about community care might be justified. DESIGN--Cross sectional surveys with review of case notes. Follow up interviews with questionnaires administered one year after discharge. SETTING--Two inner London districts (West Lambeth and Lewisham) with high levels of social deprivation and at different stages of developing community services. PATIENTS--90 and 50 patients in the two services respectively, aged 18 to 65, who satisfied the Research Diagnostic Criteria for schizophrenia and who were discharged from inpatient services. MAIN OUTCOME MEASURES--Diagnosis elicited by present state examination, global social disability rating, use of services during the three months before interview. RESULTS--89 of the 140 patients (64%) had been ill for five or more years, yet few were former long stay inpatients. 55% (50/91; 95% confidence interval 45% to 65%) of those interviewed had current psychotic mental states and 22% (27/124; 16% to 31%) were functioning socially at very poor or severely maladjusted levels. 86% (107/124) were unemployed. The majority of patients had seen a mental health or social service professional, yet only 16% (20/124) were in specialised accomodation (excluding hospitals) and only 23% (17/73) of those eligible had used day care. Small numbers of people had experienced homelessness (two) or imprisonment (four over six months). CONCLUSIONS--Many schizophrenic patients leaving local psychiatric inpatient care have active symptomatology and profound social disabilities. Community care was characterised by high rates of contact with service professionals but little supported accommodation or day activity. This group of clients may require dedicated provision, which would actively encourage them to use services protected from the demands of those with less severe illness.
Full text
PDF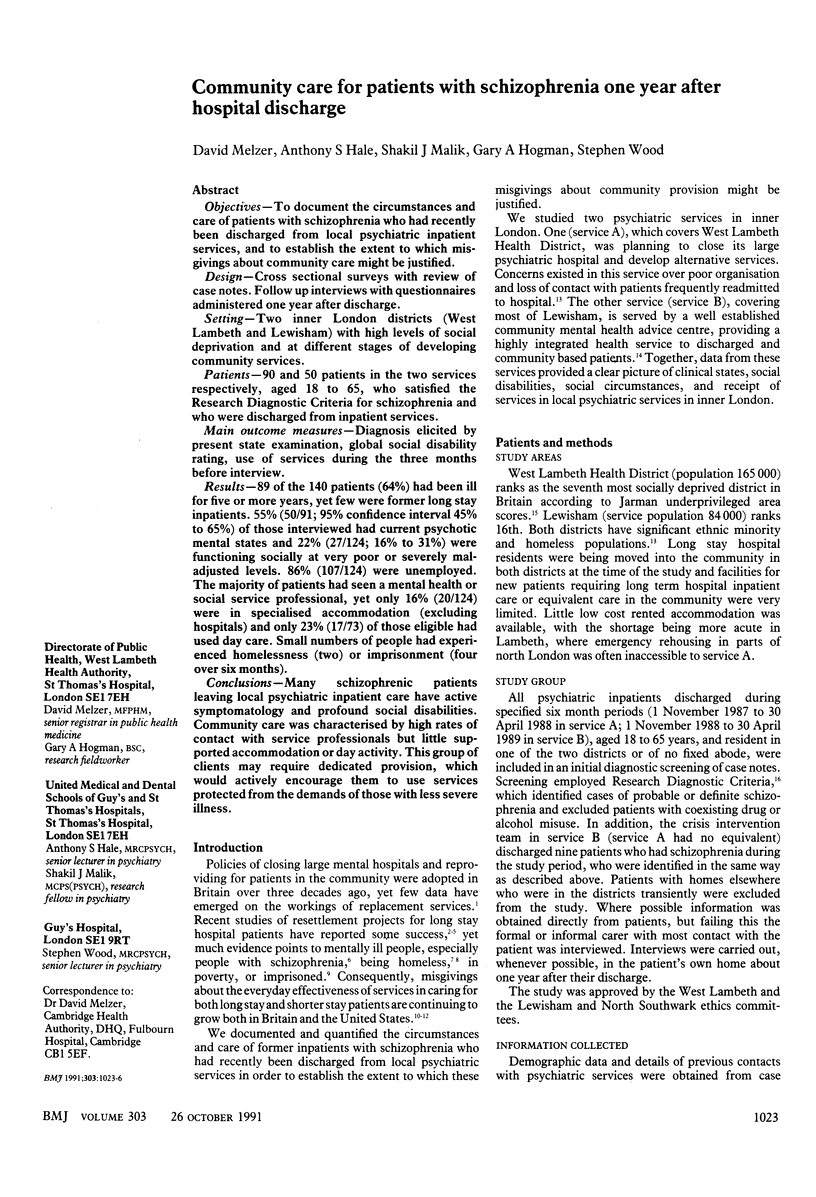


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Coid J. W. Mentally abnormal prisoners on remand: I--Rejected or accepted by the NHS? Br Med J (Clin Res Ed) 1988 Jun 25;296(6639):1779–1782. doi: 10.1136/bmj.296.6639.1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer P., Weegmann M., O'Neil M. Schizophrenia and the perception of emotions. How accurately do schizophrenics judge the emotional states of others? Br J Psychiatry. 1989 Aug;155:225–228. doi: 10.1192/bjp.155.2.225. [DOI] [PubMed] [Google Scholar]
- Ellis R. H., Wilson N. Z., Foster F. M. Statewide treatment outcome assessment in Colorado: the Colorado Client Assessment Record (CCAR). Community Ment Health J. 1984 Spring;20(1):72–89. doi: 10.1007/BF00754105. [DOI] [PubMed] [Google Scholar]
- Hogg L. I., Brooks N. New chronic schizophrenic patients: a comparison of daypatients and inpatients. Acta Psychiatr Scand. 1990 Mar;81(3):271–276. doi: 10.1111/j.1600-0447.1990.tb06495.x. [DOI] [PubMed] [Google Scholar]
- Johnstone E. C., Owens D. G., Gold A., Crow T. J., Macmillan J. F. Schizophrenic patients discharged from hospital--a follow-up study. Br J Psychiatry. 1984 Dec;145:586–590. doi: 10.1192/bjp.145.6.586. [DOI] [PubMed] [Google Scholar]
- Jones K., Robinson M., Golightley M. Long-term psychiatric patients in the community. Br J Psychiatry. 1986 Nov;149:537–540. doi: 10.1192/bjp.149.5.537. [DOI] [PubMed] [Google Scholar]
- Khoosal D., Jones P. Worcester Development Project: where do patients go when hospitals close? Health Trends. 1990;22(4):137–141. [PubMed] [Google Scholar]
- Kuipers L., Bebbington P. Expressed emotion research in schizophrenia: theoretical and clinical implications. Psychol Med. 1988 Nov;18(4):893–909. doi: 10.1017/s0033291700009831. [DOI] [PubMed] [Google Scholar]
- McCreadie R. G. The Nithsdale schizophrenia survey: I. Psychiatric and social handicaps. Br J Psychiatry. 1982 Jun;140:582–586. doi: 10.1192/bjp.140.6.582. [DOI] [PubMed] [Google Scholar]
- Olfson M. Assertive community treatment: an evaluation of the experimental evidence. Hosp Community Psychiatry. 1990 Jun;41(6):634–651. doi: 10.1176/ps.41.6.634. [DOI] [PubMed] [Google Scholar]
- Sayce L., Craig T. K., Boardman A. P. The development of community mental health centres in the U.K. Soc Psychiatry Psychiatr Epidemiol. 1991 Jan;26(1):14–20. doi: 10.1007/BF00783575. [DOI] [PubMed] [Google Scholar]
- Thornicroft G., Bebbington P. Deinstitutionalisation--from hospital closure to service development. Br J Psychiatry. 1989 Dec;155:739–753. doi: 10.1192/bjp.155.6.739. [DOI] [PubMed] [Google Scholar]
- Timms P. W., Fry A. H. Homelessness and mental illness. Health Trends. 1989 Aug;21(3):70–71. [PubMed] [Google Scholar]
- Watt D. C., Katz K., Shepherd M. The natural history of schizophrenia: a 5-year prospective follow-up of a representative sample of schizophrenics by means of a standardized clinical and social assessment. Psychol Med. 1983 Aug;13(3):663–670. doi: 10.1017/s0033291700048091. [DOI] [PubMed] [Google Scholar]
- Weller M., Tobiansky R. I., Hollander D., Ibrahimi S. Psychosis and destitution at Christmas 1985-88. Lancet. 1989 Dec 23;2(8678-8679):1509–1511. doi: 10.1016/s0140-6736(89)92946-2. [DOI] [PubMed] [Google Scholar]


