Abstract
Objective
To determine how much patients know about lithium therapy and to examine factors that might influence this knowledge.
Setting
Lithium outpatient clinic.
Patients
Patients (n = 123) affiliated with a lithium outpatient clinic (mean treatment duration of 12 years). Diagnoses, according to the Diagnostic and Statistical Manual of Mental Disorders, 3rd edition, revised, included bipolar disorder, recurrent unipolar depression and schizoaffective disorder.
Outcome measures
Quantitative assessment of lithium-related knowledge, obtained by responses to a questionnaire adapted from the Lithium Knowledge Test, and factors affecting this knowledge.
Results
Age was negatively correlated with lithium therapy knowledge scores, whereas duration of treatment, sex, education and diagnosis appeared to be unrelated to knowledge.
Conclusion
Patient education about lithium treatment should be intensified, especially for older patients taking lithium because adverse drug reactions pose a greater risk to the elderly.
Medical subject headings: drug therapy, lithium, mood disorders, patient education
Abstract
Objectif
Déterminer les connaissances des patients à l'égard de la thérapie au lithium et examiner les facteurs susceptibles d'influer sur ces connaissances.
Contexte
Patients traités au lithium en clinique externe.
Patients
Patients (n = 123) affiliés à une clinique externe de traitement au lithium (durée moyenne du traitement : 12 ans). Selon la troisième édition révisée du Manuel diagnostique et statistique des troubles mentaux, les diagnostics comprenaient un trouble bipolaire, une dépression unipolaire récidivante et un trouble schizo-affectif.
Mesures de résultats
Évaluation quantitative des connaissances du traitement par le lithium — obtenue au terme d'un questionnaire adapté du test de connaissance du lithium — et des facteurs influant sur ces connaissances.
Résultats
On a établi une corrélation négative entre l'âge et le résultat obtenu au questionnaire sur la thérapie au lithium, mais aucune corrélation entre la durée du traitement, le sexe, le niveau d'instruction, le diagnostic et le niveau de connaissances.
Conclusion
Il y aurait lieu d'intensifier l'information fournie aux patients sur le traitement au lithium, surtout chez les patients âgés traités au lithium, étant donné les risques plus élevés que posent les réactions défavorables au médicament pour les personnes âgées.
Introduction
At present, lithium prophylaxis is the most effective treatment for recurrent affective disorders,1,2,3,4,5 and there is sufficient evidence that other psychiatric disorders respond to lithium treatment as well.6 Factors affecting the long-term outcome of lithium prophylaxis are not completely understood, but compliance with treatment is probably an important predictor of outcome,7,8,9,10,11 as well as the occurrence and intensity of adverse drug reactions,7 although some conflicting data exist regarding the last issue.12
Knowledge about a drug and its effects may play an important role in establishing compliance13,14,15,16 because health beliefs are based, at least in part, on information.16 Many specialized lithium outpatient clinics, including the Berlin Lithium Clinic, therefore provide information brochures to patients.17 However, evidence for an association between patients' knowledge about lithium treatment and subsequent behaviour is sparse because there have been very few studies done.18,19,20
A more practical reason for optimal patient education is that there are substantial risks of adverse drug reactions,21,22,23 even with accepted pharmacological treatment regimens.24,25 Because long-term treatment, often characterized by monthly or longer intervals between visits in the outpatient setting, requires that patients are competent to manage their prophylaxis, it is necessary that they be well informed. This is of particular significance for elderly patients because they may have difficulties understanding and remembering essential information. However, they may also be at increased risk of lithium intoxication associated with multimorbidity and polypharmacy. Treatment-related decisions in certain situations (e.g., pregnancy) should be based on solid knowledge by both physician and patient.
To assess the degree of patients' knowledge about lithium, we gave a simple questionnaire covering a wide range of lithium-related issues to patients in a specialized lithium outpatient clinic. Domains of knowledge were mode of action of lithium, behavioural adaptations required during long-term lithium treatment, identification of side effects or intoxication, and general treatment-related issues.
Methods
A German translation of the Lithium Knowledge Test18 was prepared and screened for comprehensiveness. Because the aim of this study was to cover a wide range of important treatment issues, we also added some questions, primarily related to adverse effects of lithium and corresponding potential behavioural consequences. Academic members of the lithium clinic then met to revise the questionnaire and define the most appropriate rating format. Expansions and modifications were relatively small and likely did not influence the validity of the questionnaire.
Questions were presented as simply as possible (e.g., “Common side effects of lithium are?”), and patients were asked to mark the correct responses in a list presented after each question. A simple yes or no answer was required for each of 63 items.
We defined 4 domains of lithium-related knowledge: “mode of lithium action” (e.g., target symptoms), “treatment issues” (e.g., why blood level of lithium should be followed), “adverse drug reactions – intoxication” and “factors of importance for lithium treatment” (e.g., nutritional precautions). The number of items per domain differed according to the importance of the domain, which was determined by clinical experience. For example, the mode of action domain consisted of only 4 items, whereas adverse reactions – intoxication consisted of 27 items.
Knowledge about lithium was determined by adding the number of correct responses for each domain (domain score) and for the entire questionnaire (total score). We did not subtract 1 point for each incorrect answer (as Peet and Harvey18 did) because this would have provided no additional information and would have changed the distribution of scores. No attempt was made to standardize domain scores, so they cannot be directly compared with one another.
A research nurse invited patients to participate in the study while they were in the outpatient clinic waiting room. Patients were informed about the rationale of the study and the procedure (i.e., filling out a questionnaire) and were reassured that participation was voluntary and answers would be kept confidential. Participants were given the questionnaire to fill out before scheduled appointments with the treating psychiatrists.
Patients were former inpatients of the Department of Psychiatry, Freie Universität Berlin, or had been referred by psychiatrists in private practice. At the time of the study, they were being treated as outpatients and were affiliated with the Berlin Lithium Clinic at the Department of Psychiatry, an outpatient clinic for optimal care of and research on patients with unipolar, bipolar and schizoaffective disorders receiving lithium or other prophylactic treatment.26
At intake, patients of the clinic receive comprehensive information about lithium treatment, and knowledge is “refreshed” twice a year, usually before patients leave on holidays (performed by the nurse) and, apart from this, by the treating psychiatrist. At each visit, patients are seen by a research nurse for blood level analysis and a short physical examination and by a psychiatrist for psychopathological assessment and recording of adverse events, as well as psychopharmacological intervention. Compliance with treatment is regularly assessed and recorded for all patients.
All patients entering the Berlin Lithium Clinic must give informed written consent that their data can be used for research. Only 1 patient refused to participate in this study. Because no negative consequences from participation could be expected, formal approval for this study from the ethical board was not necessary.
Correct responses on the questionnaire were coded as 1 and missing or false responses as 0. The sum of correct responses was then subjected to statistical analysis. The Mann–Whitney U test and Kruskal–Wallis test27 were used for nonparametric comparisons, and multivariate linear regression methods were used to model patients' responses, controlling for covariates where appropriate.28
Results
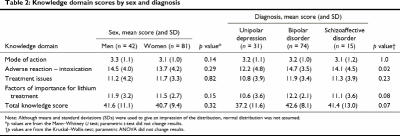
A total of 123 patients agreed to participate in this study (81 women, 42 men; mean age 52.8 years). Most had been diagnosed, according to criteria of the Diagnostic and Statistical Manual of Mental Disorders, third edition, revised (DSM-III-R), with bipolar disorder (60.2%), unipolar depression (25.2%) or schizoaffective disorder (12.2%).
All patients were taking lithium at the time they filled out the questionnaire, albeit total treatment duration differed markedly; the mean duration of treatment was 12.1 years (standard deviation [SD] 13.9 years, Table 1). Only 6 patients had been treated for less than 2 years, 22 had for less than 5 years, and the remaining patients had been treated for 5 or more years. When they filled out the questionnaire, all patients were in an euthymic state, as assessed by the AMDP rating scale for psychiatric symptoms29 and the Bech-Rafaelsen Mania Scale and Bech-Rafaelsen Melancholia Scale.30
Table 1
Education was classified as “elementary” (n = 42) when patients had graduated from an elementary school (usually 8 years of schooling) with or without (n = 10) formal occupational training; “medium” (n = 36) when an intermediate school certificate was obtained with or without (n = 1) occupational training; and “higher” (n = 45) when a high school certificate and various degrees of occupational training were obtained. Five (4%) patients were unemployed, 24 (19.5%) were retired, 16 (13%) were blue-collar workers, 40 (32.5%) had nonacademic white-collar jobs, 19 (15.5%) were housewives, 2 (1.6%) were studying at a university, but had former occupational training, and 17 (13.8%) held academic professions.
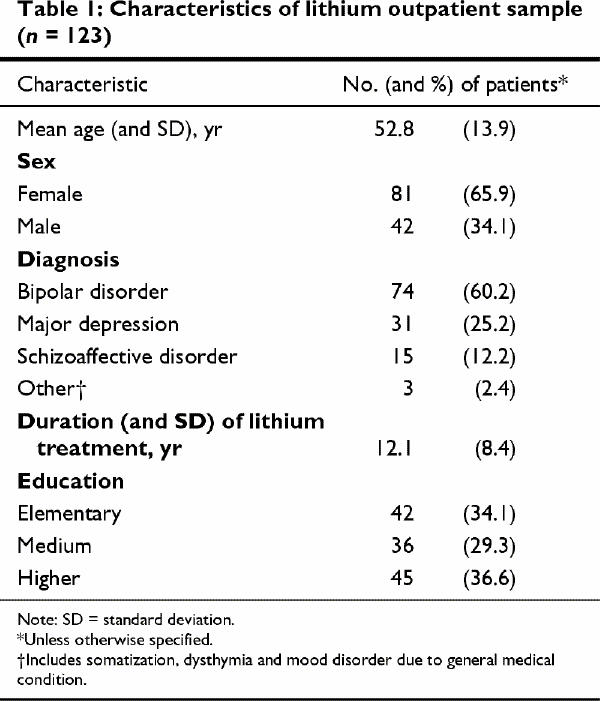
Approximately two-thirds of the responses to the 63 questions were correct (mean 41.0, median 43, SD 10, range 5–60). Table 2 shows results for each knowledge domain and total score broken down by sex and diagnosis. Patients with bipolar disorder scored highest in all knowledge domains, whereas scores for the group with unipolar depression were lowest, especially for adverse drug reactions and treatment-related issues. Sex differences were not observed.
Table 2
Because the group with unipolar depression was significantly older than the others (mean 61.2 yr v. 49.9 yr and 48.7 yr for the bipolar and schizoaffective group respectively, p < 0.001) and tended to be less educated (p = 0.084, Fisher's exact test), we used a multivariate linear regression model to estimate the influence of diagnosis, age, education and duration of treatment on the total knowledge score. For domains of knowledge, negative Spearman correlation coefficients were found with age and knowledge of behavioural adaptation (r = –0.46, p < 0.001), knowledge of adverse drug reactions–intoxication signs (r = –0.46, p < 0.001), and knowledge of factors of importance for lithium treatment (r = –0.40, p < 0.001); knowledge of mode of action was less strongly associated with age (r = –0.22, p = 0.016). The correlations between treatment duration and total score were generally lower. Thus, it seems that age, per se, not duration of treatment, predicted poor knowledge about lithium.
Because age and duration of treatment were positively associated (Spearman rank correlation coefficient, r = 0.30, p < 0.001), but both were associated with the total score to different degrees (rage/total score = –0.51, p < 0.001, rduration/total score = –0.15, p = 0.1), we adopted a modelling strategy, where different coefficients for age are estimated, conditional on duration of lithium treatment. Duration of treatment was treated as a continuous variable, in addition to introducing 3 regression coefficients for age given by terziles of treatment duration (estimated separately). Thus, it could be determined if the association between age and knowledge was solely due to the fact that older patients started lithium prophylaxis earlier (giving them more of a chance to forget information or to have been informed less thoroughly) or whether there was no substantial modifying effect associated with duration of treatment, indicating that, independent of treatment duration, elderly patients knew less about their prophylaxis. Results of this analysis (Table 3, Fig. 1) suggest that age is inversely associated with knowledge, and the other covariates do not seem to contribute in predicting knowledge. A marginal trend of a decreasing association with increasing duration might be discussed. However, the direction remains constant. Although for both sexes, knowledge was significantly related to age, when age was nested within sex, a stronger association appeared for men than for women.
Table 3
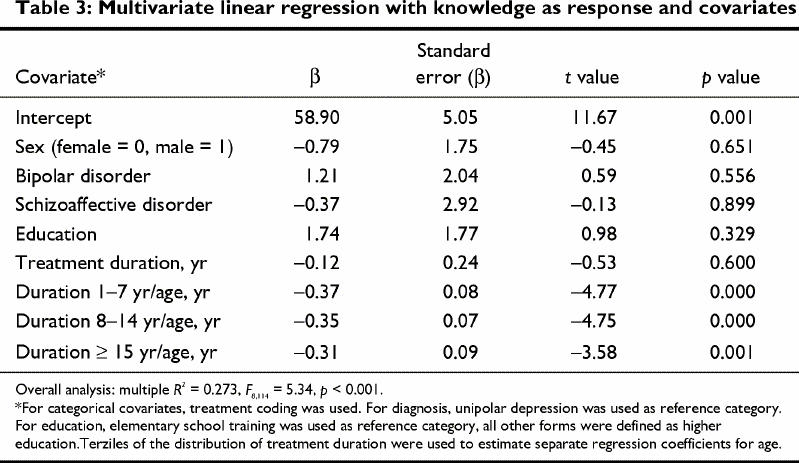
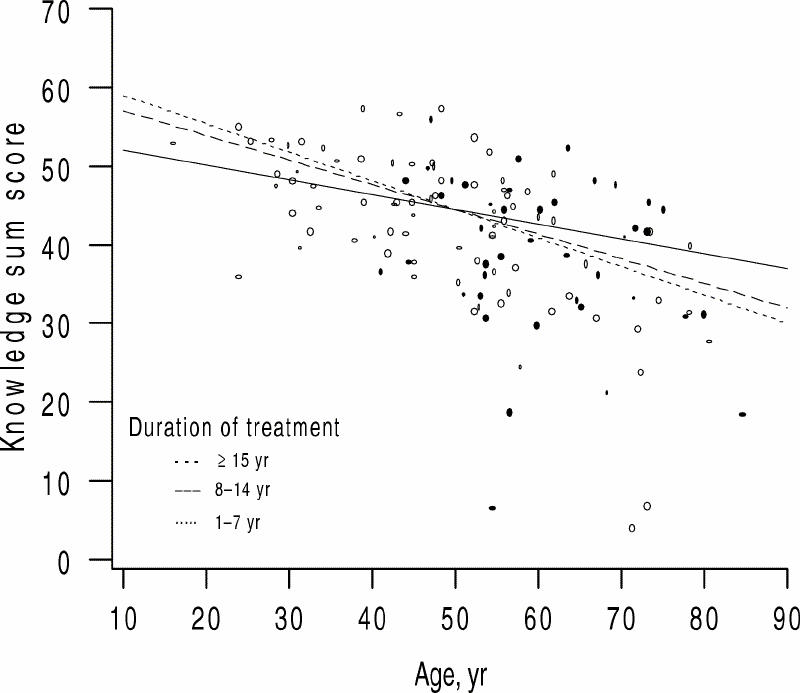
Fig. 1: Scatterplot of lithium-related knowledge versus age of patients, separated by duration of lithium treatment based on terziles of treatment duration of the whole group.
Discussion
No patient in our highly selected and compliant lithium outpatient clinic sample was able to answer all of the questions related to lithium treatment correctly. On average, one-third of questions were not answered correctly. We did not find that knowledge scores were related to sex, education or diagnosis. A consistent negative association between age and lithium-related knowledge was obtained. This association was independent of duration of treatment with lithium (i.e., it did not matter if a patient had been taking lithium for 1–7 years or over 15 years — knowledge scores were lower with increasing age). Although evident for both sexes, the relation with age was more pronounced for men than for women.
Our results were surprising because we had assumed that patients in a specialized lithium clinic would have full knowledge of their treatment. In fact, many of these patients who had been taking lithium for years did not have sufficient knowledge. Although the study is uncontrolled and the sample is relatively small, these findings deserve attention.
It seems that older patients need particularly careful information and instruction, both when lithium treatment is initiated and during continuation. It might be argued that elderly patients may have had difficulty coping with the questions. We did not examine the cognitive capacity of these patients, but the questions were presented in a simple format and none of the items in the questionnaire exceeded the information usually given to patients. In addition, the patients' understanding of the instructions was carefully checked by the research nurse.
Compliance did not seem to pose serious problems in this sample. In fact, informal ratings of staff personnel regarding patient compliance (based on serum concentration monitoring and clinical impression) resulted in only 6 subjects with questionable compliance. It can therefore be assumed that we measured lithium-related knowledge, but not, for example, negative attitudes toward lithium treatment, which might otherwise confound knowledge and compliance.
If it is true that neurotoxic effects and other adverse effects of lithium pose a greater risk to more elderly people,31,32,33,34 poorly informed patients should be more prone to encounter such risks. We cannot test this hypothesis, however, because we did not examine the frequency of adverse reactions in this study. Because adverse reactions with long-term lithium treatment are rare, large samples would be required to assess whether these events are due to a lack of information.
It is tempting to speculate that the management of adverse reactions could be improved by patients themselves if adequate knowledge was present and that this improvement would be greatest for older patients because their knowledge was the most limited in this study. Similar associations of treatment-related knowledge and age have not often been examined formally in psychiatric settings, nor in other settings of somatic diseases,35,36,37 but it seems reasonable that such an association exists. Therefore, future research should address whether more knowledge, in fact, prevents adverse events and risky situations and whether patient education can further improve knowledge, particularly in elderly patients where other limitations (e.g., cognitive factors,16 low interest in treatment issues38) might hamper educational efforts.
Acknowledgments
We thank Mrs. Ilse Becker and Mrs. Marta Mau (research nurses) and Mrs. Marianne Wald (technician) for their Cupertino and advice and Dr. Thomas Wolf (psychologist) for his helpful contributions in preparing the questionnaire.
Footnotes
Correspondence to: Dr. Rainer T. Schaub, Department of Psychiatry and Psychotherapy, Ernst-Moritz-Arndt-Universität Greifswald, Rostocker Chaussee 70, 18437 Stralsund, Germany; fax 49 3831 452104; schaub@mail.uni-greifswald.de
Submitted Apr. 5, 2000 Revised Aug. 28, 2000 Accepted Oct. 23, 2000
References
- 1.Bowden CL. Key treatment studies of lithium in manic-depressive illness: efficacy and side effects. J Clin Psychiatry 1998; 59(6 Suppl):13-9. [PubMed]
- 2.Denicoff KD, Smith-Jackson EE, Disney ER, Ali SO, Leverich GS, Post RM. Comparative prophylactic efficacy of lithium, carbamazepine, and the combination in bipolar disorder. J Clin Psychiatry 1997;58(11):470-8. [DOI] [PubMed]
- 3.Grof P. Has the effectiveness of lithium changed? Impact of the variety of lithium's effects. Neuropsychopharmacology 1998; 19(3):183-8. [DOI] [PubMed]
- 4.Greil W, Ludwig-Mayerhofer W, Erazo N, Engel RR, Czernik A, Giedke H, et al. Comparative efficacy of lithium and amitriptyline in the maintenance treatment of recurrent unipolar depression: a randomised study. J Affect Disord 1996;40(3):179-90. [DOI] [PubMed]
- 5.Greil W, Ludwig-Mayerhofer W, Erazo N, Schochlin C, Schmidt S, Engel RR, et al. Lithium versus carbamazepine in the maintenance treatment of bipolar disorders — a randomised study. J Affect Disord 1997;43(2):151-61. [DOI] [PubMed]
- 6.Meltzer HY. Treatment-resistant schizophrenia — the role of clozapine. Curr Med Res Opin 1997;14(1):1-20. [DOI] [PubMed]
- 7.Gitlin MJ, Cochran SD, Jamison KR. Maintenance lithium treatment: side effects and compliance [see comments]. J Clin Psychiatry 1989;50(4):127-31. [PubMed]
- 8.Lenzi A, Lazzerini F, Placidi GF, Cassano GB, Akiskal HS. Predictors of compliance with lithium and carbamazepine regimens in the long-term treatment of recurrent mood and related psychotic disorders. Pharmacopsychiatry 1989;22(1):34-7. [DOI] [PubMed]
- 9.Jamison KR, Gerner RH, Goodwin FK. Patient and physician attitudes toward lithium: relationship to compliance. Arch Gen Psychiatry 1979;36(8 Spec No):866-9. [DOI] [PubMed]
- 10.Aagaard J, Vestergaard P, Maarbjerg K. Adherence to lithium prophylaxis: II. Multivariate analysis of clinical, social, and psychosocial predictors of nonadherence. Pharmacopsychiatry 1988;21(4):166-70. [DOI] [PubMed]
- 11.Aagaard J, Vestergaard P. Predictors of outcome in prophylactic lithium treatment: a 2-year prospective study. J Affect Disord 1990;18(4):259-66. [DOI] [PubMed]
- 12.Schumann C, Berghöfer A, Müller-Oerlinghausen B. Non-adherence with long-term prophylaxis: a 6-year naturalistic follow-up study of affectively ill patients. Psychiatry Res 1999; 89(3):247-57. [DOI] [PubMed]
- 13.Schou M. The combat of non-compliance during prophylactic lithium treatment. Acta Psychiatr Scand 1997;95(5):361-3. [DOI] [PubMed]
- 14.Tettersell MJ. Asthma patients' knowledge in relation to compliance with drug therapy. J Adv Nurs 1993;18(1):103-13. [DOI] [PubMed]
- 15.Tempier R. Long-term psychiatric patients' knowledge about their medication. Psychiatr Serv 1996;47(12):1385-7. [DOI] [PubMed]
- 16.Lorenc L, Branthwaite A. Are older adults less compliant with prescribed medication than younger adults? Br J Clin Psychol 1993;32(Pt 4):485-92. [DOI] [PubMed]
- 17.Walker J. Use of a patient education booklet to improve compliance with lithium therapy [letter]. Psychosomatics 1981;22:51. [DOI] [PubMed]
- 18.Peet M, Harvey NS. Lithium maintenance: 1. A standard education programme for patients [see comments]. Br J Psychiatry 1991;158:197-200. [DOI] [PubMed]
- 19.Connelly CE. Compliance with outpatient lithium therapy. Perspect Psychiatr Care 1984;22(2):44-50. [DOI] [PubMed]
- 20.Harvey NS, Kay R. Compliance during lithium treatment, intra-erythrocyte lithium variability, and relapse. J Clin Psychopharmacol 1991;11(6):362-7. [PubMed]
- 21.Kampf D. Lithium und Nierenfunktion. In: Müller-Oerlinghausen B, Greil W, Berghöfer A, editors. Die Lithiumtherapie. Berlin: Springer-Verlag; 1997. p. 368-81.
- 22.Mavrogiorou P, Hegerl U. Neurologische, neuromuskuläre und neurotoxische Effekte der Lithiumtherapie. In: Müller-Oerlinghausen B, Greil W, Berghöfer A, editors. Die Lithiumtherapie. Berlin: Springer-Verlag; 1997. p. 330-41.
- 23.Bschor T, Bauer M, Albrecht J. Beeinflussung der Schilddrüsenfunktion durch Lithium. In: Müller-Oerlinghausen B, Greil W, Berghöfer A, editors. Die Lithiumtherapie. Berlin: Springer-Verlag; 1997. p. 357-67.
- 24.American Psychiatric Association. Practice guideline for the treatment of patients with bipolar disorder. Am J Psychiatry 1994;151(Suppl):1-36. [DOI] [PubMed]
- 25.Rush AJ. Mood disorders: systematic medication management. Modern problems of pharmacopsychiatry. Vol. 25. Basel: Karger; 1997.
- 26.Pietzcker A, Muller-Oerlinghausen B. The outpatient clinic for patients under chronic lithium or neuroleptic treatment as a phase-IV research tool. Pharmacopsychiatry 1984;17(5):162-7. [DOI] [PubMed]
- 27.Armitage P, Berry G. Statistical methods in medical research. 3rd ed. Oxford: Blackwell Scientific; 1994.
- 28.Ripley B, Venables B. Modern applied statistics with S-Plus. Berlin: Springer-Verlag; 1995.
- 29.Das AMDP-System [The AMDP-System]. 4th ed. Berlin: Springer-Verlag; 1981.
- 30.Bech P. Rating scales for affective disorders. Their validity and consistency. Acta Psychiatr Scand 1981;295:1-101. [PubMed]
- 31.Flint AJ, Rifat SL. A prospective study of lithium augmentation in antidepressant-resistant geriatric depression. J Clin Psychopharmacol 1994;14(5):353-6. [PubMed]
- 32.Lafferman J, Solomon K, Ruskin P. Lithium augmentation for treatment-resistant depression in the elderly. J Geriatr Psychiatry Neurol 1988;1(1):49-52. [DOI] [PubMed]
- 33.Zimmer B, Rosen J, Thornton JE, Perel JM, Reynolds CF 3rd. Adjunctive lithium carbonate in nortriptyline-resistant elderly depressed patients. J Clin Psychopharmacol 1991;11(4):254-6. [PubMed]
- 34.Hardy BG, Shulman KI, Zucchero C. Gradual discontinuation of lithium augmentation in elderly patients with unipolar depression. J Clin Psychopharmacol 1997;17(1):22-6. [DOI] [PubMed]
- 35.Anderson JM, Wiggins S, Rajwani R, Holbrook A, Blue C, Ng M. Living with a chronic illness: Chinese-Canadian and Euro-Canadian women with diabetes — exploring factors that influence management. Soc Sci Med 1995;41(2):181-95. [DOI] [PubMed]
- 36.Ankri J, Beaufils B, Ledisert D, Henrard JC. Behavior regarding therapeutic drugs and self concept of elderly persons with chronic diseases [in French]. Soc Sci Med 1997;44(3):337-45. [DOI] [PubMed]
- 37.Becker G, Beyene Y, Newsom EM, Rodgers DV. Knowledge and care of chronic illness in three ethnic minority groups. Fam Med 1998;30(3):173-8. [PubMed]
- 38.Bailey BJ, Carney SL, Gillies AH, McColm LM, Smith AJ, Taylor M. Hypertension treatment compliance: what do patients want to know about their medications? Prog Cardiovasc Nurs 1997;12(4):23-8. [PubMed]