Abstract
Objective
To assess if the lithium dosage prescribed according to the Pepin method leads to therapeutic serum concentrations of lithium.
Methods
For 13 healthy volunteers, the initial daily doses of lithium were calculated according to the Pepin formula with a view to obtaining a serum lithium level of 0.8 mmol/L. Lithium was administered twice daily for 21 days, and blood samples were drawn daily, 12 hours after the last dose was taken. Dosage was adjusted if serum concentrations were below 0.6 mmol/L or above 1.0 mmol/L or if major side effecTots were reported.
Results
Daily lithium doses ranged from 1050 mg to 1950 mg (mean 1569 mg, standard deviation [SD] 291 mg), The mean serum lithium concentrations for weeks 1, 2 and 3 were 0.74 mmol/L (SD 0.19 mmol/L), 0.67 mmol/L (SD 0.22 mmol/L) and 0.69 mmol/L (SD 0.13 mmol/L), respectively. Within-subject variance was negligible. Sixty-eight percent of the serum lithium concentration measurements fell between 0.57 mmol/L and 0.83 mmol/L, and 84% fell within the recommended therapeutic range of 0.60 mmol/L and 1.20 mmol/L.
Conclusions
The Pepin method is a safe but conservative method for predicting the appropriate daily dose of lithium.
Medical subject headings: bipolar disorder; dose-response relationship, drug; forecasting; lithium; models, biological
Abstract
Objectif
Déterminer si la dose de lithium prescrite selon la méthode Pepin produit des concentrations thérapeutiques de lithium dans le sérum.
Méthodes
Chez 13 volontaires en bonne santé, on a calculé les doses quotidiennes initiales de lithium en fonction de la formule Pepin afin d'obtenir des taux de 0,8 mmol/L de lithium dans le sérum. Le lithium a été administré deux fois par jour pendant 21 jours et l'on a prélevé des échantillons de sang tous les jours, 12 heures après la dernière dose. On a rajusté la posologie si les taux sériques tombaient à moins de 0,6 mmol/L ou dépassaient 1,0 mmol/L, ou si l'on signalait des effets secondaires importants.
Résultats
Les doses quotidiennes de lithium ont varié de 1050 mg à 1950 mg (moyenne de 1569 mg, écart type [ET] de 291 mg). Les concentrations moyennes de lithium dans le sérum au cours des semaines 1, 2 et 3 se sont établies à 0,74 mmol/L (ET, 0,19 mmol/L), 0,67 mmol/L (ET, 0,22 mmol/L) et 0,69 mmol/L (ET, 0,13 mmol/L) respectivement. L'écart chez un même sujet a été négligeable. Soixante-huit pour cent des mesures de concentration du lithium dans le sérum ont varié de 0,57 mmol/L à 0,83 mmol/L et 84 % se sont établies à l'intérieur de la plage thérapeutique recommandée de 0,60 mmol/L à 1,20 mmol/L.
Conclusions
La méthode Pepin est une façon sécuritaire mais conservatrice de calculer la bonne dose quotidienne de lithium.
Introduction
At the beginning of bipolar patients' treatment with lithium, it is often necessary to adjust the dosage as fast as possible. The recommended serum level to obtain a beneficial effect in bipolar disorder is between 0.60 mmol/L and 1.20 mmol/L.1,2 Inappropriate dosage can entail a poor control of symptoms and potentially dangerous side effects.3 Thus, predicting the optimal dosage to obtain optimal therapeutic concentration is important. An individualized approach to drug dosage is therefore necessary for the safe and effective use of lithium medication. It has been shown that pharmacokinetic techniques such as Cooper's method may lead to potentially toxic lithium dosage. Initial lithium dosage is most often calculated via empirical methods and then titrated on the basis of serum lithium determinations to achieve appropriate concentrations.4,5,6,7 However, this method may yield errors in the initial dosage, with associated increased risk of undertreatment or toxicity and a delay in reaching the desired serum concentrations.3 To lessen these problems, methods for predicting individual dosage requirements have been developed.8
There are several methods to predict serum lithium levels.9,10,11,12,13,14,15,16 Pepin et al14 developed a method that predicts dosage on the basis of an estimate of the lithium body clearance. This approach does not rely on measuring serum lithium concentrations to make a prediction. According to Patrias and Moore,10 the Zetin formula overestimates the appropriate dosage of lithium 3 times more frequently than the Pepin formula. Furthermore, the Zetin equation was recently found to be a poor predictor of lithium dose.17,18,19
A more recent study20 compared the Zetin, Jermain21 and Pepin a priori methods and an empirical method to predict lithium dosage requirements. The records of 47 patients were used in the study, and dosage and serum concentration data were analyzed to assess the precision and bias of each a priori method. The Jermain and empirical methods significantly overpredicted concentration and underpredicted dosage; the Zetin method overpredicted dosage; and the Pepin method underpredicted dosage but not concentration. The average difference in dosage error among the methods was 73.3 mg/day. The authors concluded that the 3 methods were similar to an empirical method in their ability to predict lithium dosages.
One of the shortcomings of many previous studies investigating dosage and serum levels of lithium is the retrospective approach taken. To date, only 2 such studies have been conducted prospectively with patients with bipolar disorder.22,23 Moreover, Rosenberg et al24 found that a mathematical model used for dose prediction was moderately accurate but tended to predict a lower dose than was actually required, and Markoff and King25 reported that dose-prediction errors with the Zetin alogrithm led to underdosing. Browne et al26 compared pharmacokinetic and empirical dosing methods and failed to demonstrate any statistically significant differences among the procedures. In light of the above-mentioned difficulties,27,28,29,30,31,32,33,34,35 a prospective study is needed to examine the prediction errors of the Pepin method.
Methods
Participants were recruited through advertisements in local papers. Individuals were eligible to take part in the study if they met the following criteria: 18–50 years of age; no heart, thyroid or kidney conditions; no mental illness; and no general anesthesia in the past 6 months. In addition, women of childbearing age had to be using a reliable method of birth control and have had a negative pregnancy test before inclusion in the trial. All subjects gave full informed consent and were seen in an outpatient setting; compliance rates were monitored as closely as possible.36,37,38,39
The final sample comprised 15 of 30 healthy volunteers selected for a double-blind, placebo-controlled study of the effects of lithium on cognition.40
Lithium
The active agent used in this experiment was a slow-release lithium carbonate (Lithizine) in 150-mg and 300-mg capsules. The initial daily dose was calculated according to the Pepin formula to obtain a desired blood serum lithium level of 0.8 mmol/L, the mean clinical concentration used in lithium therapy. Blood samples were drawn weekly, in the morning, 12 hours after the last intake of lithium or placebo.
The Pepin formula is written as follows (Equation 1) where D = dosage of lithium in mmol (300 mg lithium carbonate = 8.12 mmol), Css_min = desired steady-state trough concentration in mmol/L, V_app = apparent volume of distribution (calculated as Cl_Li/K), t = dosage interval (day), F = fraction absorbed (1.0) and k = 0.693/t1/2_Li
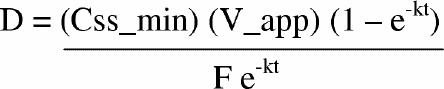 |
Complimentary formulas to solve the Pepin equation include:
· To determine ideal weight (kg):
for men, weight = 50 + 90.551 (height – 1.524)
for women, weight = 45.5 + 90.551 (height – 1.524)
· To determine clearance of creatinine (mL/min):
for men, Cl_Cr = [(140 – age)(weight)]/(72 Cr_S)
for women, Cl_Cr = [0.85(140 – age)(weight)]/(72 Cr_S)
· To determine clearance of lithium (mL/min):
Cl_Li = 0.235(Cl_Cr)
· To determine t1/2 (h):
t1/2_Li = t1/2_n/{1 – Fe [1 – (Cl_Cr/100)]},
where t1/2_n = 24 h and Fe = 0.95 (dose excretion).
Daily maintenance dose was adjusted in increments of 300 mg during the treatment phase if the serum lithium concentration was more than 0.2 mmol/L from the target level (i.e., 0.8 mmol/L) or reduced if major side effects were reported.
Data analysis
The variation between subjects and between weeks was calculated with an analysis of variance; the critical level of significance was set at 0.05.
Results
Lithium serum concentrations of 15 of 30 healthy volunteers selected for a double-blind, placebo-controlled study of the effects of lithium on cognition40 were monitored over the study period. One volunteer dropped out during the course of the study and another was removed for medical reasons. The final sample therefore comprised 13 healthy volunteers — 6 women and 7 men (mean age 32 years [range 18–44 years]) with a mean education level of 16 years (range 12–25 years).
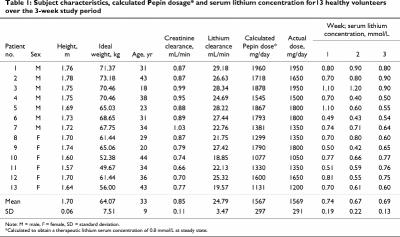
Initial daily doses calculated with the Pepin formula ranged from 1050 mg to 1950 mg (mean 1569 mg, standard deviation [SD] 291 mg). Mean lithium serum levels were 0.74 mmol/L (SD 0.19 mmol/L) for week 1, 0.67 mmol/L (SD 0.22 mmol/L) for week 2 and 0.69 mmol/L (SD 0.13 mmol/L) for week 3 (Table 1).
Table 1
During the first few days of lithium intake, side effects (i.e., headaches, nausea and, less frequently, vomiting and diarrhea) were reported by 4 subjects. In contrast to studies where lithium dosage is increased slowly, 41 7 of the subjects guessed they were receiving lithium. This is likely related to our dosage regimen, where maximum doses were administered at the start to obtain the target serum lithium concentration of 0.8 mmol/L (Fig. 1).
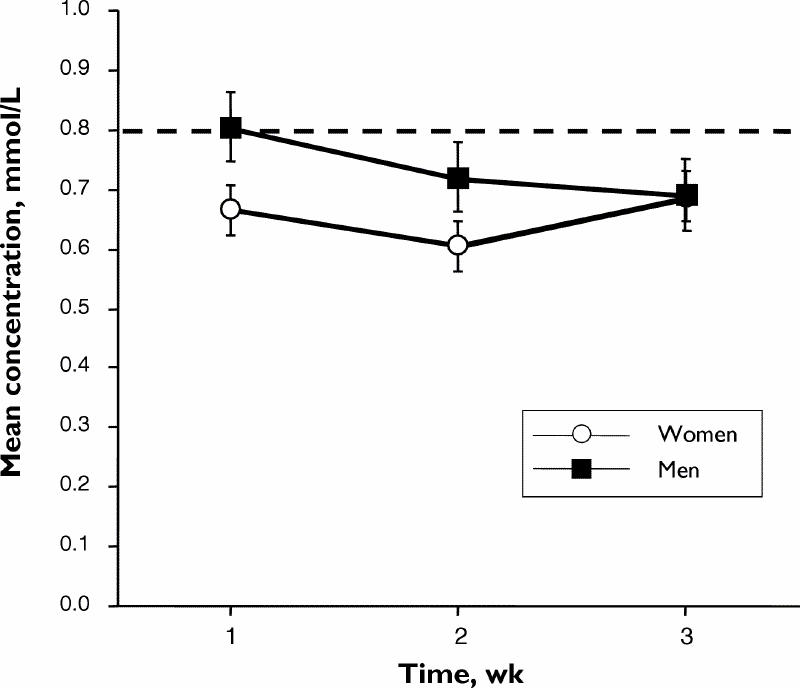
Fig 1: Mean serum concentrations of lithium in men (n = 7) and women (n = 6) participating in the study over a 3-week period.
The variation between subjects was greater than that within subjects over time. In fact, the difference between weeks was not significant. To assess the proportion of subjects falling outside the “optimal” therapeutic concentration range, the between-subject variance (i.e., 0.018) was used. Sixty-eight percent of the serum sample concentrations were between 0.57 mmol/L and 0.83 mmol/L, and 84% were in the therapeutic range between 0.6 mmol/L and 1.2 mmol/L.
Because the Pepin method was used to achieve a steady-state concentration of 0.8 mmol/L, its predictive performance was estimated by the absolute differences from the 0.8 mmol/L. We first tested, using a general linear model, in function of time, whether the mean of the differences was null. There was no significant statistical difference between times. However, the overall mean serum lithium level of 0.70 mmol/L was significantly different from 0.8 mmol/L (F = 5.7, p = 0.034).
Because the actually administered dosage did not correspond to the Pepin dosage, we considered the relative error between the observed lithium concentration and the expected concentrations according to Pepin formula. Once again, there was no significant statistical trend over time. The difference between the overall mean concentration of lithium (0.70 mmol/L, SD 0.15 mmol/L) and the mean of expected concentrations (0.79 mmol/L, SD 0.05 mmol/L) approached significance (F = 4.34, p = 0.05). We also examined the difference between the dosage administered and the Pepin dosage needed to reach the concentrations observed. Once again, there was no significant statistical effect of time, but the difference between the mean actual dosage and the mean Pepin dosage required to obtain the observed concentrations was significant (F = 8.28, p = 0.014).
Discussion
The Pepin method gave reasonable estimates of the required dosages to obtain serum lithium levels within the range of 0.6 mmol/L to 1.2 mmol/L for 84% of the samples taken in the study. However, the concentrations of lithium reached were statistically lower than those expected from the Pepin formula. It would appear that the dosages from Pepin formula are conservative. This study confirms Wright and Crismon's20 report that the Pepin method underpredicts dosage.
Potential limitations to the generalization of our results must be considered. The number of subjects in this study was small and the age range was narrow. In addition, these healthy volunteers were likely to be more treatment compliant than patients with psychiatric disorders. If patients had been included in the investigation, we would have been able to assess the effects of non-adherence.
Because our study was conducted in an outpatient setting, potential biases such as sodium intake and concurrent treatment could not be assessed, particularly with respect to the use of nonsteroidal anti-inflammatory drugs and alcohol. Although subjects were asked to report any changes in their habits, including alcohol and drug use, a lack of such reports should not be interpreted to mean abstinence.
One would also predict that healthy young volunteers would be less likely to be outliers (i.e., require dosages much higher or lower than the mean); but this is where the real clinical value of prediction techniques lies.
Our study was not designed to provide data that we could compare with results obtained using other mathematical methods to predict initial lithium dosage. Therapeutic monitoring of lithium is highly amenable to a mathematical approach because of the lack of metabolic confounds. Moreover, Sproule et al42 report that “fuzzy logic” can be used for pharmacokinetic modelling for predicting serum lithium concentrations.42
Prediction of the daily dose of lithium necessary to achieve concentrations within the therapeutic range is highly relevant to clinical practice, and our results indicate that Pepin method is probably a safe method to predict the appropriate daily dose of lithium.
Conclusion
An accurate, unbiased and safe method for predicting appropriate lithium dosage would be an asset to clinical practice. There have been a number of methods proposed in the literature, but none are used in routine clinical practice. Although our data support the use of the Pepin method, the method relies heavily on the calculated creatinine clearance for parameter estimations. It is therefore not surprising that a small group of young healthy subjects with normal renal function would perform similarly with this prediction method. What is needed in the future is an evaluation of this method in a wide range of patients with varying degrees of renal dysfunction.
Acknowledgments
We thank Technilab in Montreal, Que., for providing Lithizine and Dr. Lakshmi N. Yatham for reviewing the manuscript.
Footnotes
Competing interests: None declared.
Correspondence to: Dr. Emmanuel Stip, Centre de Recherche Fernand-Seguin, Hôpital Louis-H. Lafontaine, 7331 Hochelaga St., Montreal QC H1N 3V2; fax 514 251-2617; emmanuel.stip@umontreal.ca
Submitted Mar. 14, 2000 Revised Feb. 20, 2001 Accepted Mar. 6, 2001
References
- 1.American Psychiatric Association. Practice guideline for the treatment of patients with bipolar disorder. Am J Psychiatry 1994;151(Suppl 12):1-36. [DOI] [PubMed]
- 2.Sharma V, Yatham L, Haslam D, Silverstone P, Parikh S, Matte R, et al. Continuation and prohylactic treatment of bipolar disorder. Can J Psychiatry 1997;42(Suppl 2):92S-100S. [PubMed]
- 3.Peterse JW, Havenaar J, Van Rijn H. Possible hazard in use of priming dose to determine lithium dosage. Am J Psychiatry 1999;156(1):157-8. [DOI] [PubMed]
- 4.Cooper TB, Simpson GM. The 24 hour lithium level as a progosticator of dosage requirements. Am J Psychiatry 1976;133: 440-3. [DOI] [PubMed]
- 5.Perry PJ, Prince RA, Alexander B, Dunner FJ. Prediction of lithium maintenance doses using a single point prediction protocol. J Clin Psychopharmacol 1983;3(1):13-7. [PubMed]
- 6.Marr MA, Djuric PE, Ritschel WA, Garver DL. Prediction of lithium carbonate dosage in psychiatric inpatients using the repeted one-point method. Clin Pharm 1983;2(3):243-8. [PubMed]
- 7.Taright N, Mentre F, Mallet A, Jouvent R. Nonparametric estimation of population characteristics of the kinetics of lithium from observational and experimental data: individualization of chronic dosing regimen using a new Bayesian approach. Ther Drug Monit 1994;16:258-69. [DOI] [PubMed]
- 8.Dugas JE, Feeney AM. Evaluation of a new lithium dosage-prediction technique. Clin Pharm 1983;2(3):249-52. [PubMed]
- 9.Pepin SM, Baker DE, Nance KS. Lithium dosage calculation from age, sex, height, weight, amd serum creatinine. Proceedings of the 15th Annual ASHP Midyear Clinical Meeting; Dec. 1980; San Francisco.
- 10.Patrias J, Moore F. Evaluating of two methods for predicting initial lithium dosage without measuring serum concentrations. Clin Pharm 1985;4:77-9. [PubMed]
- 11.Zetin M, Garber D, Cramer M. A simple mathematical model for predicting lithium dose requirements. J Clin Psychiatry 1983; 44:144-5. [PubMed]
- 12.Valecha N, Tayal G, Tripathi K. Single dose pharmacokinetics of lithium and prediction of maintenace dose in manic depressive patients. Indian J Med Res 1990;409-416. [PubMed]
- 13.Zetin M, Garber D, De Antonio M, Schlegel A, Feureisen S, Fieve R, et al. Prediction of lithium dose: a mathematical alternative to the test-dose method. J Clin Psychiatry 1986;47(4):175-8. [PubMed]
- 14.Lobeck F. A review of lithium dosing methods. Pharmacotherapy 1988;8(4):248-55. [DOI] [PubMed]
- 15.Lobeck F, Nelson MV, Evans RL, Hornstra RK. Evaluation of four methods for predicting lithium dosage. Clin Pharm 1987; 6(3):230-3. [PubMed]
- 16.Yukawa E, Nomiyama N, Higuchi S, Aoyama T. Lithium population pharmacokinetics from routine clinical data: role of patient characteristics for estimating dosing regimens. Ther Drug Monit 1993;15(2):75-82. [DOI] [PubMed]
- 17.Terao T, Oga T, Nozaki S, Ota A, Otsubo Y, Yammamoto S, et al. A further prospective evaluation of an equation to predict daily lithium dose. J Clin Psychiatry 1995;56(5):193-5. [PubMed]
- 18.Ubeta B, Sanchez A, Sangrador G. Predictive capacity of four methods of lithium dosage. Farmacia e Clinicia 1990;7(7):572-8.
- 19.Valenca J, Klepacz, Calil HM. Prediction of lithium therapeutic dose. Revista APB-APAL 1989;11(2):76-80.
- 20.Wright R, Crismon ML. Comparison of three a priori methods and one empirical method in predicting lithium dosage requirements. Am J Health Syst Pharm 2000;57(18):1698-702. [DOI] [PubMed]
- 21.Jermain DM, Crismon ML, Martin ES. Population pharmacokinetics of lithium. Clin Pharm 1991;10:376-81. [PubMed]
- 22.Cummings MA, Haviland MG, Wareham JG, Fontana LA. A prospective clinical evaluation of an equation to predict daily lithium dose. J Clin Psychiatry 1993;54(2):55-8. [PubMed]
- 23.Perry PJ, Alexander B, Prince RA, Dunner FJ. The utility of a single-point dosing protocol for predicting steady-state lithium levels. Br J Psychiatry 1986;148:401-5. [DOI] [PubMed]
- 24.Rosenberg JG, Binder RL, Berlant J. Prediction of therapeutic lithium dose: comparison and improvement of current methods. J Clin Psychiatry 1987;48(7):284-6. [PubMed]
- 25.Markoff RA, King M. Does lithium dose prediction improve treatment efficiency? Prospective evaluation of a mathematical method. J Clin Psychopharmacol 1992;12(5):305-8. [PubMed]
- 26.Browne JL, Huffman CS, Golden RN. A comparison of pharmacokinetic versus empirical lithium dosing techniques. Ther Drug Monit 1989;11(2):149-54. [DOI] [PubMed]
- 27.Carson SW. Lithium. In: Evans WE, Schentag JJ, Jusko W, editors. Applied pharmacokinetics. 3rd ed. Vancouver: Applied Therapeutics; 1992. p. 34:1-26.
- 28.Amdisen A. Monitoring of lithium treatment through determination of lithium concentration. Dan Med Bull 1975;22:277-91. [PubMed]
- 29.Dugas JE. Slowly titrated lithium doses delay therapeutic response. Clin Pharm 1984;3:236-7. [PubMed]
- 30.Slattery JT, Gibaldi M, Koup J. Prediction of maintenance dose required to attain a desired drug concentration at steady state from a single determination after an initial dose. Clin Pharmacokinet 1980;5:377-85. [DOI] [PubMed]
- 31.Slattery JT. Single-point maintenance prediction: role of interindividual differences in clearance and volume of distribution in choice of sampling. J Pharm Sci 1981;70:1174-6. [DOI] [PubMed]
- 32.Browne JL, Huffman CS, Golden RN. A comparison of pharmacokinetic versus empirical lithium dosing techniques. Ther Drug Monit 1989;2:149-54. [DOI] [PubMed]
- 33.Amidisen A. Serum level monitoring and clinical pharmacokinetics of lithium. Clin Pharmacokinet 1977;2:73-92. [DOI] [PubMed]
- 34.Sheiner LB, Beal SL. Some suggestions for measuring predictive performance. J Pharmacokinet Biopharm 1981;9:503-12. [DOI] [PubMed]
- 35.Marken PA, McCrary KE, Lacombe S, Sommi RW, Hornstra RK Jr, Pierce CA, et al. Preliminary comparison of predictive and empiric lithium dosing: impact on patient outcome. Ann Pharmacother 1994;28:1148-52. [DOI] [PubMed]
- 36.Connelly CE. Compliance with outpatient lithium therapy. Perspect Psychiatr Care 1984;22(2):44-50. [DOI] [PubMed]
- 37.Cochran SD, Gitlin MJ. Attitudinal correlates of lithium compliance in bipolar affective disorder. J Nerv Ment Dis 1988;176(8): 457-64. [DOI] [PubMed]
- 38.Ulrich G, Frick K, Stieglitz RD, Muller-Oerlinghausen B. Interindividual variability of lithium-induced EEG changes in healthy volunteers. Psychiatry Res 1987;20(2):117-27. [DOI] [PubMed]
- 39.Silverstone PH, Hanstock CC, Rotzinger S. Lithium does not alter the choline/creatine ratio in the temporal lobe of human volunteers as measured by proton magnetic resonance spectroscopy. J Psychiatry Neurosci 1999;24(3):222-6. [PMC free article] [PubMed]
- 40.Stip E, Dufresne J, Lussier I, Yatham L. A double-blind, placebo-controlled study of the effects of lithium on cognition in healthy subjects. J Affect Disord 2000;60:147-57. [DOI] [PubMed]
- 41.Calil HM, Zwicker P, Kleepacz S. The effect of lithium carbonate on healthy volunteers: mood stabilization. Biol Psychiatry 1990;27:711-22. [DOI] [PubMed]
- 42.Sproule BA, Bazoon M, Shulman KI, Turksen IB, Naranjo CA. Fuzzy logic pharmakokinetic modeling: application to lithium concentration prediction. Clin Pharmacol Ther 1997;62(1):29-40. [DOI] [PubMed]