Abstract
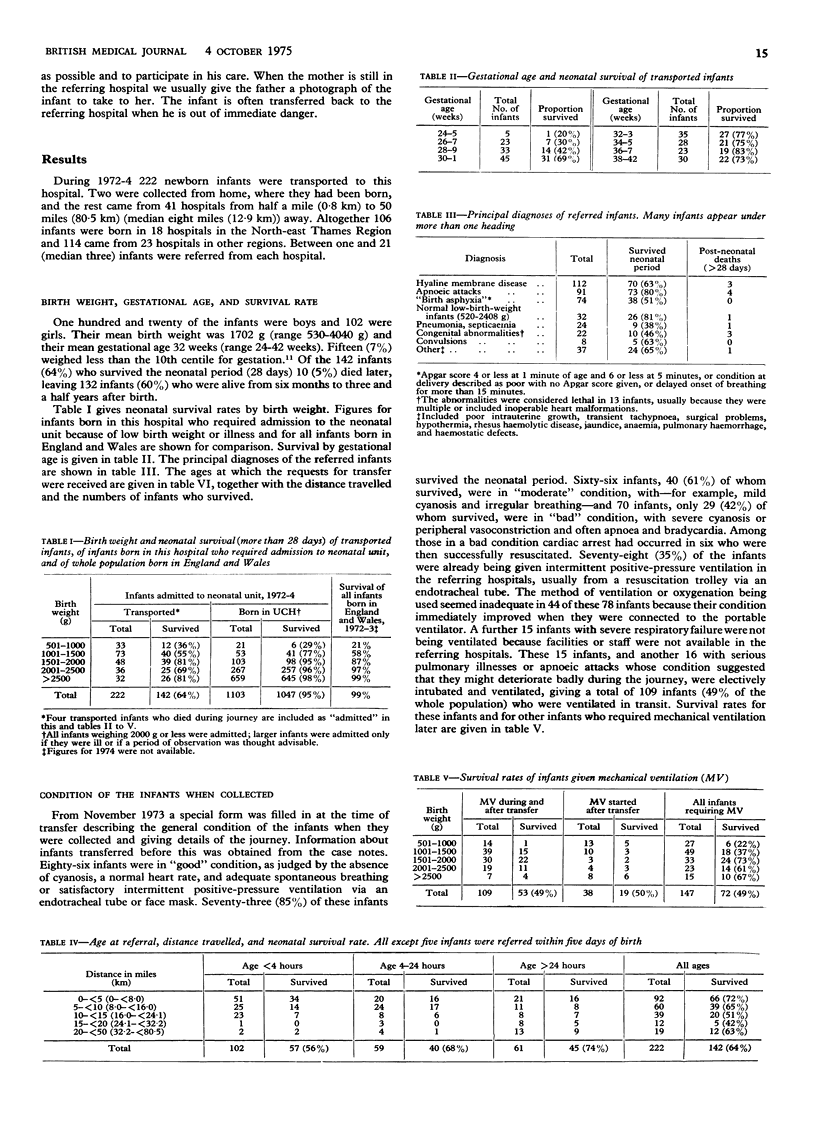
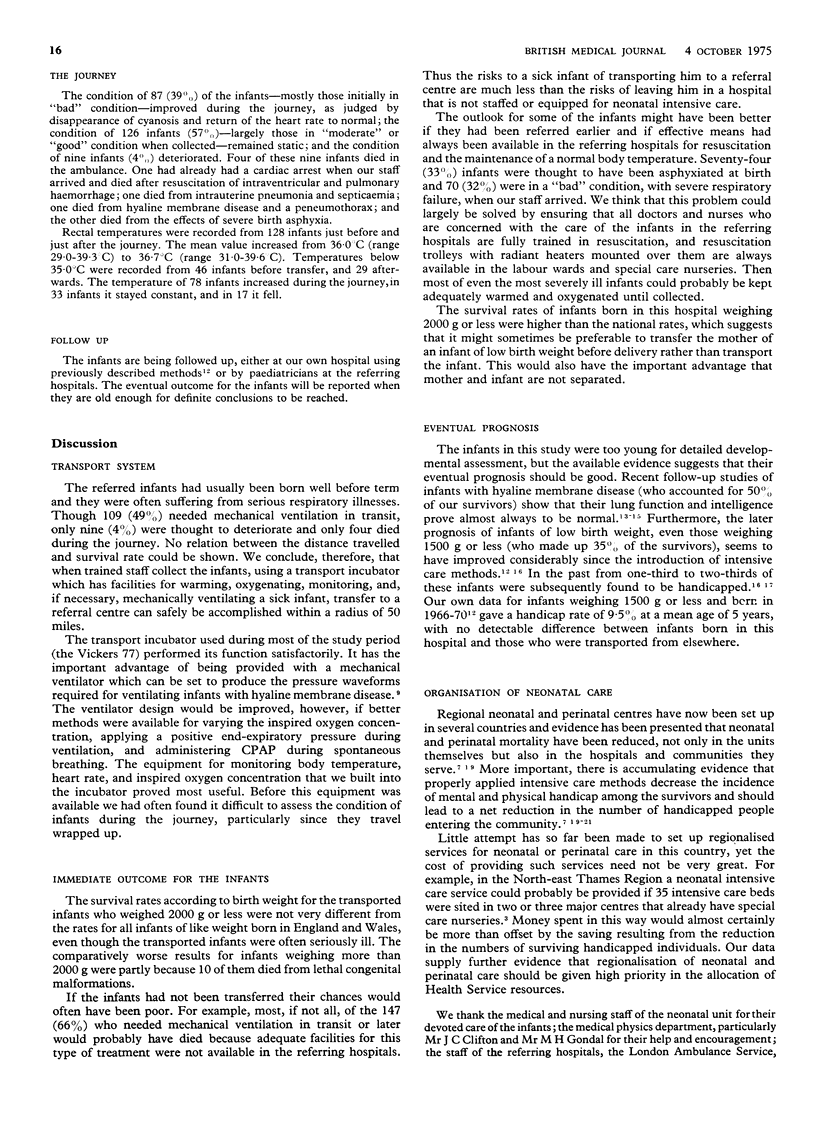
During the three years 1972-4 222 newborn infants were transported to this hospital for intensive care. They were collected by trained staff using a specially modified transport incubator with an in-built mechanical ventilator and facilities for monitoring body temperature, heart rate, and inspired oxygen concentration. Two of the infants came from home and the rest from 41 hospitals from half a mile (0-8 km) to 50 miles (80-5 km) (median eight miles (12-9 km)) away. The mean birth weight of the infants was 1702 g (range 520-4040 g) and their mean gestational age was 32 weeks (range 24-42 weeks). The principal reasons for referral were low birth weight and severe respiratory illnesses. Altogether 109 (49%) of the infants needed mechanical ventilation in transit and another 38 (17%) needed it later. During the journey the condition of 88 (40%) of the infants was thought to improve, in 125 (56%) it was static and in nine (4%)--four of whom died--it deteriorated. A total of 142 infants (64%) survived the neonatal period. There was no correlation between the distance travelled and the survival rate. Seriously ill newborn infants may be transported safely to a referral centre within a radius of 50 miles, and the risks of the journey are negligible compared with the risks of leaving the infant in a hospital that is not staffed or equipped for neonatal intensive care.
Full text
PDF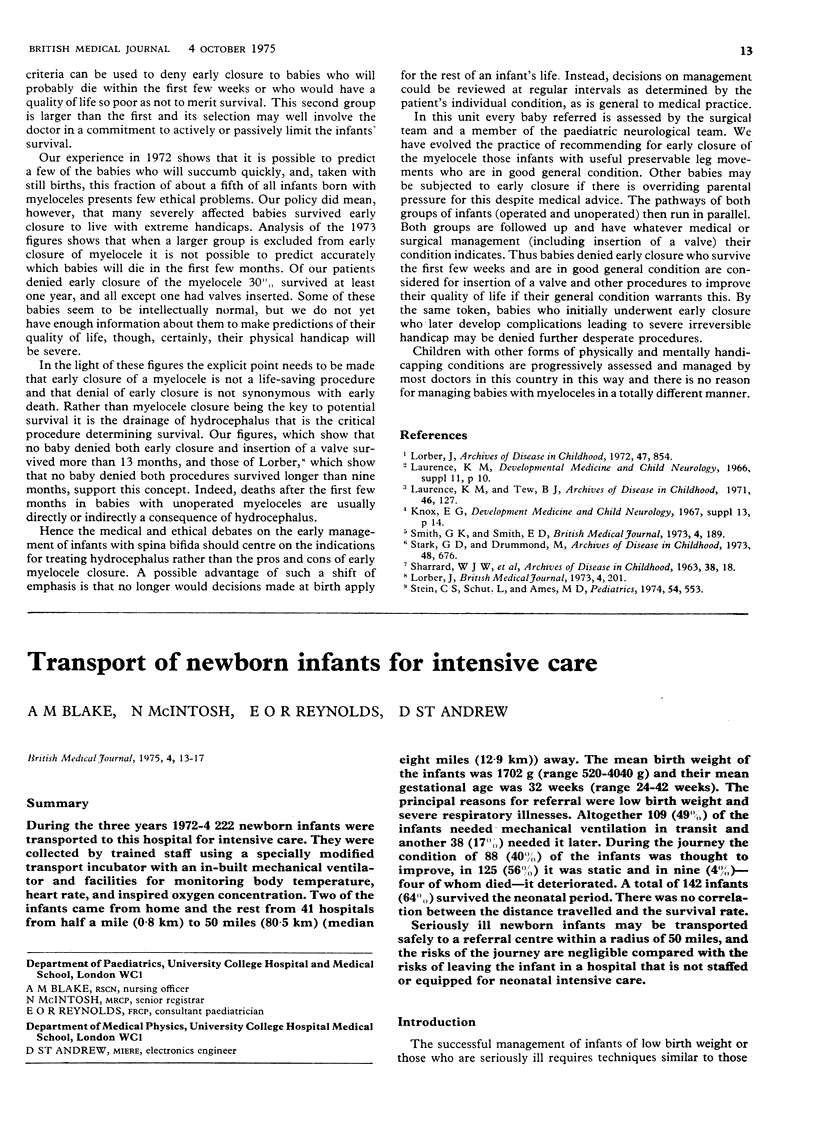

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bryan M. H., Levison H., Swyer P. R. Pulmonary function in infants and children following the acute neonatal respiratory distress syndrome. Bull Physiopathol Respir (Nancy) 1973 Nov-Dec;9(6):1587–1600. [PubMed] [Google Scholar]
- DRILLIEN C. M. Growth and development in a group of children of very low birth weight. Arch Dis Child. 1958 Feb;33(167):10–18. doi: 10.1136/adc.33.167.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisch R. O., Bilek M. K., Miller L. D., Engel R. R. Physical and mental status at 4 years of age of survivors of the respiratory distress syndrome. Follow-up report from the collaborative study. J Pediatr. 1975 Apr;86(4):497–503. doi: 10.1016/s0022-3476(75)80137-5. [DOI] [PubMed] [Google Scholar]
- Gregory G. A., Kitterman J. A., Phibbs R. H., Tooley W. H., Hamilton W. K. Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure. N Engl J Med. 1971 Jun 17;284(24):1333–1340. doi: 10.1056/NEJM197106172842401. [DOI] [PubMed] [Google Scholar]
- LUBCHENCO L. O., HANSMAN C., DRESSLER M., BOYD E. INTRAUTERINE GROWTH AS ESTIMATED FROM LIVEBORN BIRTH-WEIGHT DATA AT 24 TO 42 WEEKS OF GESTATION. Pediatrics. 1963 Nov;32:793–800. [PubMed] [Google Scholar]
- Segal S. Transfer of a premature or other high-risk newborn infant to a referral hospital. Pediatr Clin North Am. 1966 Nov;13(4):1195–1205. doi: 10.1016/s0031-3955(16)31913-7. [DOI] [PubMed] [Google Scholar]
- Stahlman M., Hedvall G., Dolanski E., Faxelius G., Burko H., Kirk V. A six-year follow-up of clinical hyaline membrane disease. Pediatr Clin North Am. 1973 May;20(2):433–446. doi: 10.1016/s0031-3955(16)32853-x. [DOI] [PubMed] [Google Scholar]
- Storrs C. N., Taylor M. R. Transport of sick newborn babies. Br Med J. 1970 Aug 8;3(5718):328–332. doi: 10.1136/bmj.3.5718.328. [DOI] [PMC free article] [PubMed] [Google Scholar]


