Abstract
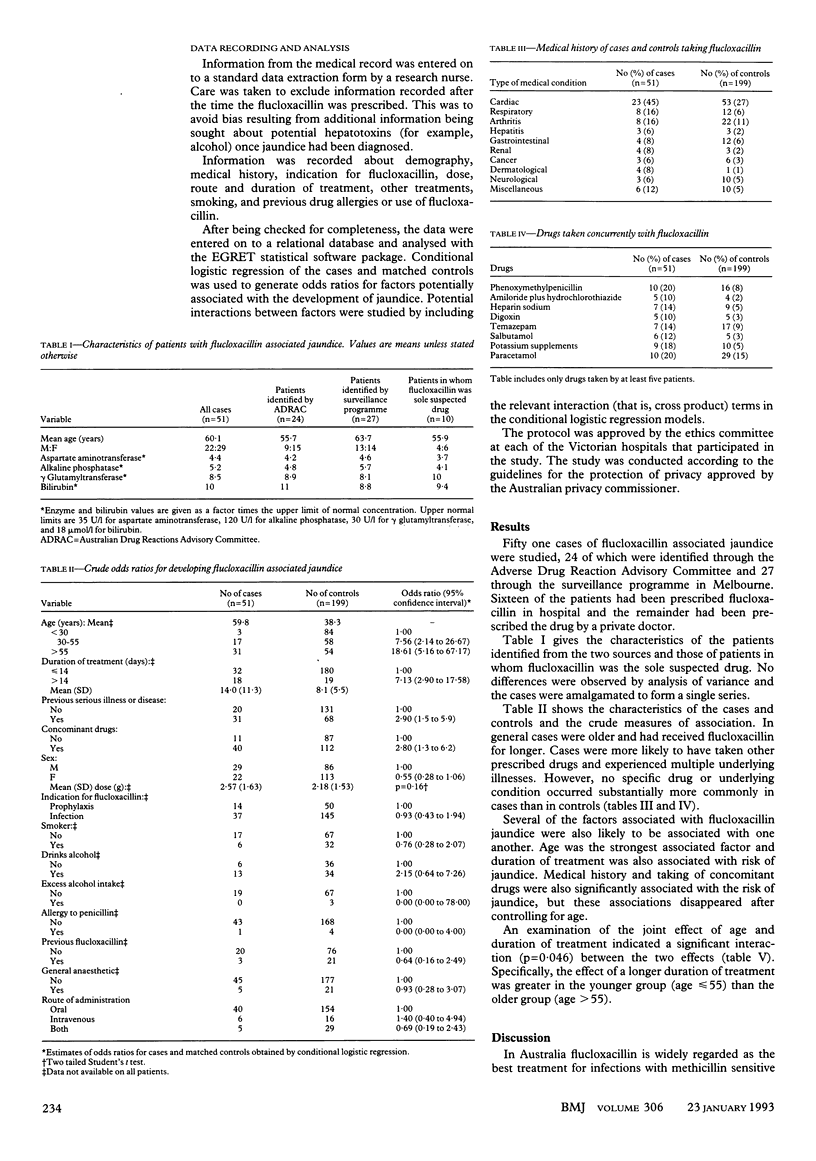
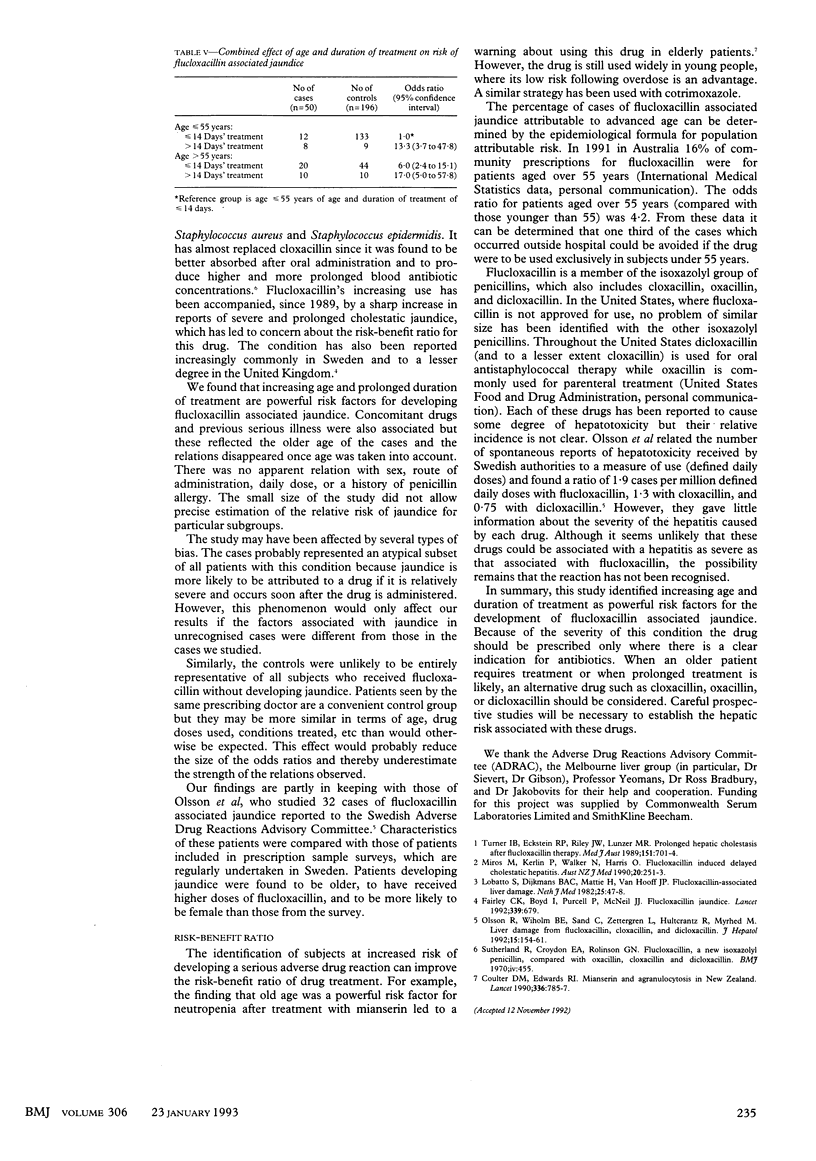
OBJECTIVES--To identify risk factors predisposing to the development of flucloxacillin associated jaundice. DESIGN--Case-control study. Medical records of cases and controls were reviewed and information recorded on standard data collection forms. SETTING--Alfred Hospital recruiting subjects from Melbourne, Sydney, and Brisbane. SUBJECTS--Cases were defined as patients who had developed jaundice within eight weeks of stopping flucloxacillin, biochemical test results suggesting cholestasis, normal calibre bile ducts, and not been taking recognised hepatotoxic drugs. 51 of the 53 patients referred were included in the study. Four controls for each case were randomly selected from the patient register of the prescribing doctor. These were defined as patients who had been prescribed flucloxacillin without developing jaundice. MAIN OUTCOME MEASURES--Demographic characteristics, medical history, indication for flucloxacillin, dose, route and duration of treatment, other drugs, smoking, and previous drug allergies or use of flucloxacillin. RESULTS--Increasing age and a prolonged duration of flucloxacillin treatment were found to be risk factors for the development of jaundice. Patients aged over 55 years had an odds ratio of 18.61 (95% confidence interval 5.16-67.17) compared with patients under 30. The odds ratio for patients prescribed flucloxacillin for over 14 days was 7.13 (2.90 to 17.58) compared with patients treated for 14 days or less. Dose and route of administration were not related to the risk of jaundice. CONCLUSIONS--Older patients and those receiving flucloxacillin for longer than two weeks are at a substantially greater risk of jaundice. Careful consideration of the risk-benefit ratio is required when flucloxacillin is used in these settings.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Coulter D. M., Edwards I. R. Mianserin and agranulocytosis in New Zealand. Lancet. 1990 Sep 29;336(8718):785–787. doi: 10.1016/0140-6736(90)93248-n. [DOI] [PubMed] [Google Scholar]
- Fairley C. K., Boyd I., Purcell P., McNeil J. Flucloxacillin jaundice. Lancet. 1992 Mar 14;339(8794):679–679. doi: 10.1016/0140-6736(92)90837-s. [DOI] [PubMed] [Google Scholar]
- Miros M., Kerlin P., Walker N., Harris O. Flucloxacillin induced delayed cholestatic hepatitis. Aust N Z J Med. 1990 Jun;20(3):251–253. doi: 10.1111/j.1445-5994.1990.tb01032.x. [DOI] [PubMed] [Google Scholar]
- Olsson R., Wiholm B. E., Sand C., Zettergren L., Hultcrantz R., Myrhed M. Liver damage from flucloxacillin, cloxacillin and dicloxacillin. J Hepatol. 1992 May;15(1-2):154–161. doi: 10.1016/0168-8278(92)90029-o. [DOI] [PubMed] [Google Scholar]
- Turner I. B., Eckstein R. P., Riley J. W., Lunzer M. R. Prolonged hepatic cholestasis after flucloxacillin therapy. Med J Aust. 1989 Dec 4;151(11-12):701–705. doi: 10.5694/j.1326-5377.1989.tb139652.x. [DOI] [PubMed] [Google Scholar]


