Abstract
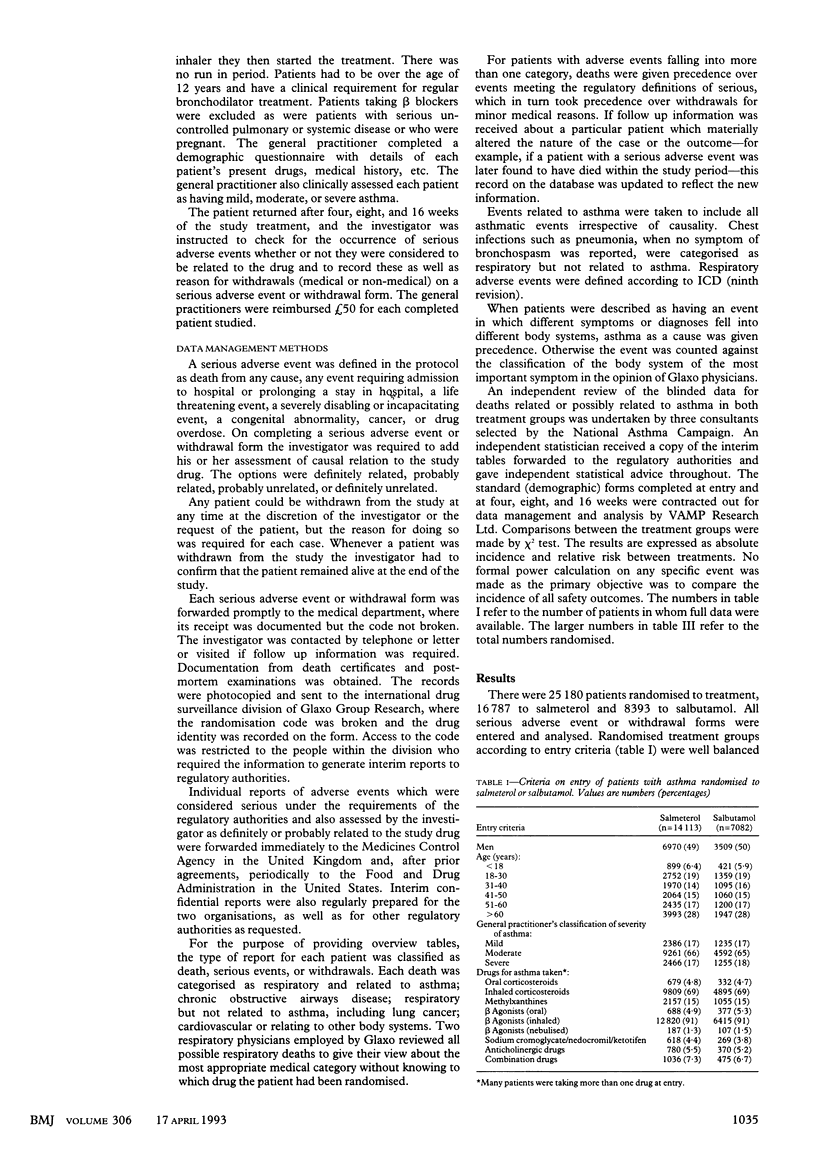
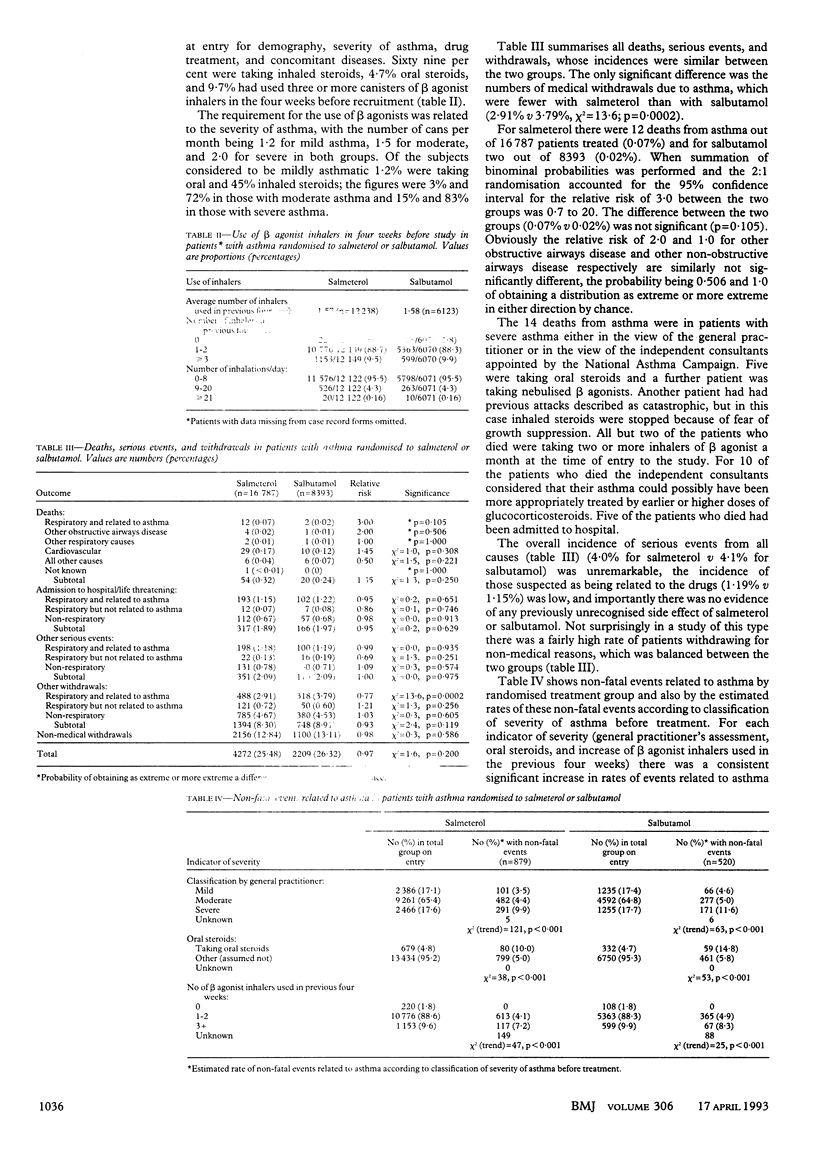
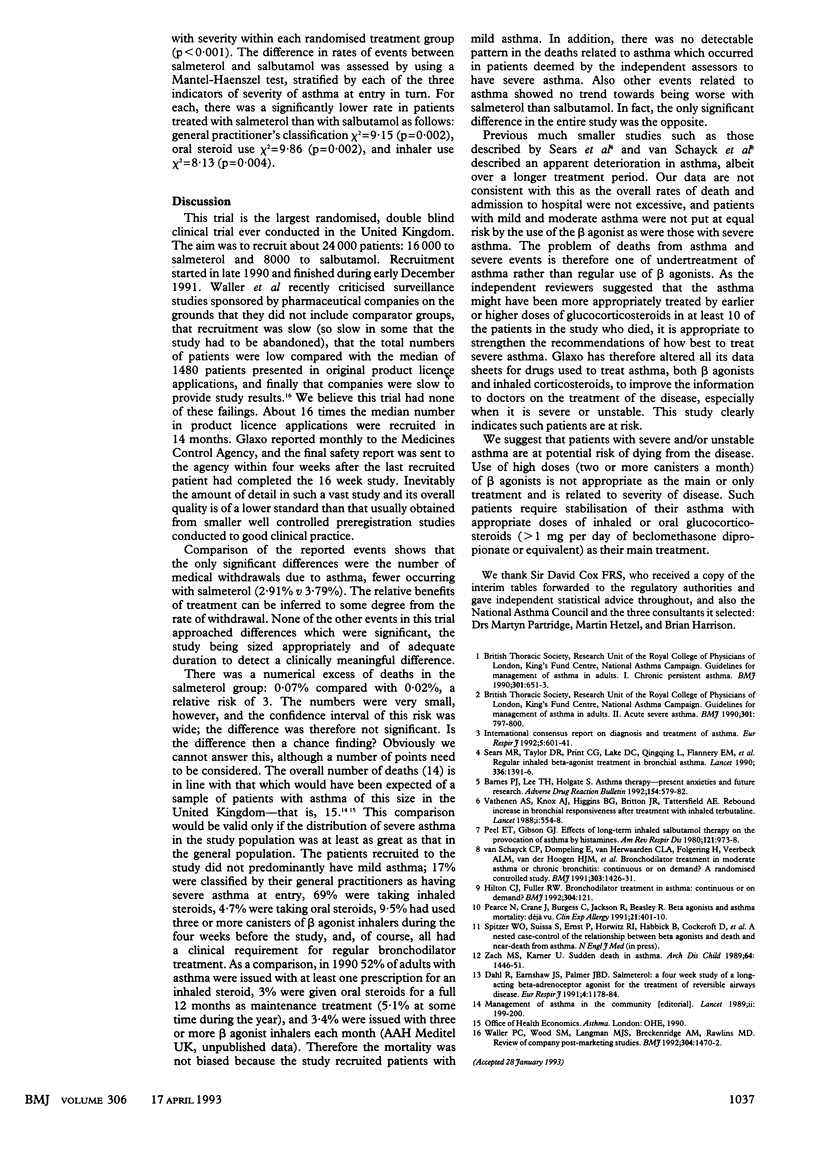
OBJECTIVE--To compare safety of salmeterol and salbutamol in treating asthma. DESIGN--Double blind, randomised clinical trial in parallel groups over 16 weeks. SETTING--General practices throughout the United Kingdom. SUBJECTS--25,180 patients with asthma considered to require regular treatment with bronchodilators who were recruited by their general practitioner (n = 3516). INTERVENTIONS--Salmeterol (Serevent) (50 micrograms twice daily) or salbutamol (200 micrograms four times a day) randomised in the ratio of two patients taking salmeterol to one taking salbutamol. All other drugs including prophylaxis against asthma were continued throughout the study. MAIN OUTCOME MEASURES--All serious events and reasons for withdrawals (medical and non-medical) whether or not they were considered to be related to the drugs. RESULTS--Fewer medical withdrawals due to asthma occurred in patients taking salmeterol than in those taking salbutamol (2.91% v 3.79%; chi 2 = 13.6, p = 0.0002). Mortality and admissions to hospital were as expected. There was a small but non-significant excess mortality in the group taking salmeterol and a significant excess of asthma events including deaths in patients with severe asthma on entry. Use of more than two canisters of bronchodilator a month was particularly associated with the occurrence of an adverse asthma event. CONCLUSIONS--Treatment over 16 weeks with either salmeterol or salbutamol was not associated with an incidence of deaths related to asthma in excess of that predicted. Overall control of asthma was better in patients allocated to salmeterol. Serious adverse events occurred in patients most at risk on entry and were probably due to the disease rather than treatment.
Full text
PDF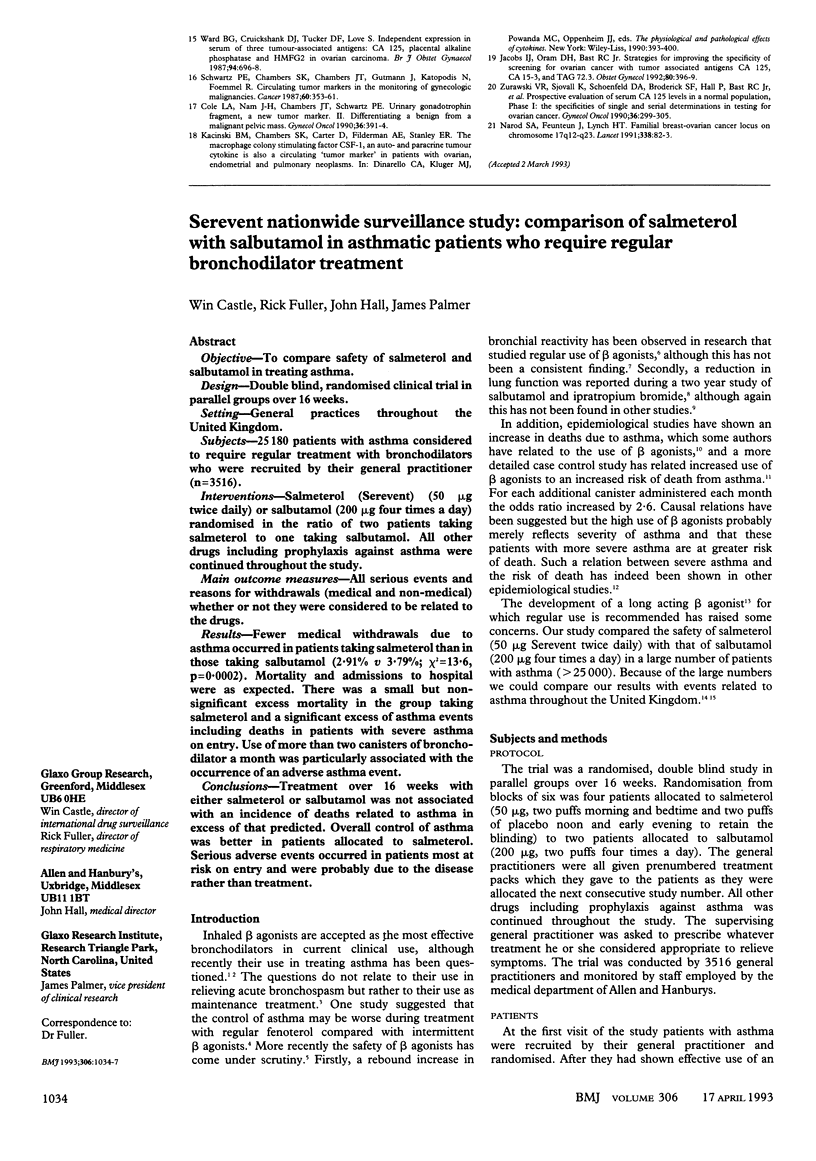
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Pearce N., Crane J., Burgess C., Jackson R., Beasley R. Beta agonists and asthma mortality: déjà vu. Clin Exp Allergy. 1991 Jul;21(4):401–410. doi: 10.1111/j.1365-2222.1991.tb01679.x. [DOI] [PubMed] [Google Scholar]
- Peel E. T., Gibson G. J. Effects of long-term inhaled salbutamol therapy on the provocation of asthma by histamine. Am Rev Respir Dis. 1980 Jun;121(6):973–978. doi: 10.1164/arrd.1980.121.6.973. [DOI] [PubMed] [Google Scholar]
- Sears M. R., Taylor D. R., Print C. G., Lake D. C., Li Q. Q., Flannery E. M., Yates D. M., Lucas M. K., Herbison G. P. Regular inhaled beta-agonist treatment in bronchial asthma. Lancet. 1990 Dec 8;336(8728):1391–1396. doi: 10.1016/0140-6736(90)93098-a. [DOI] [PubMed] [Google Scholar]
- Vathenen A. S., Knox A. J., Higgins B. G., Britton J. R., Tattersfield A. E. Rebound increase in bronchial responsiveness after treatment with inhaled terbutaline. Lancet. 1988 Mar 12;1(8585):554–558. doi: 10.1016/s0140-6736(88)91352-9. [DOI] [PubMed] [Google Scholar]
- Waller P. C., Wood S. M., Langman M. J., Breckenridge A. M., Rawlins M. D. Review of company postmarketing surveillance studies. BMJ. 1992 Jun 6;304(6840):1470–1472. doi: 10.1136/bmj.304.6840.1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zach M. S., Karner U. Sudden death in asthma. Arch Dis Child. 1989 Oct;64(10):1446–1451. doi: 10.1136/adc.64.10.1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Schayck C. P., Dompeling E., van Herwaarden C. L., Folgering H., Verbeek A. L., van der Hoogen H. J., van Weel C. Bronchodilator treatment in moderate asthma or chronic bronchitis: continuous or on demand? A randomised controlled study. BMJ. 1991 Dec 7;303(6815):1426–1431. doi: 10.1136/bmj.303.6815.1426. [DOI] [PMC free article] [PubMed] [Google Scholar]



