Abstract
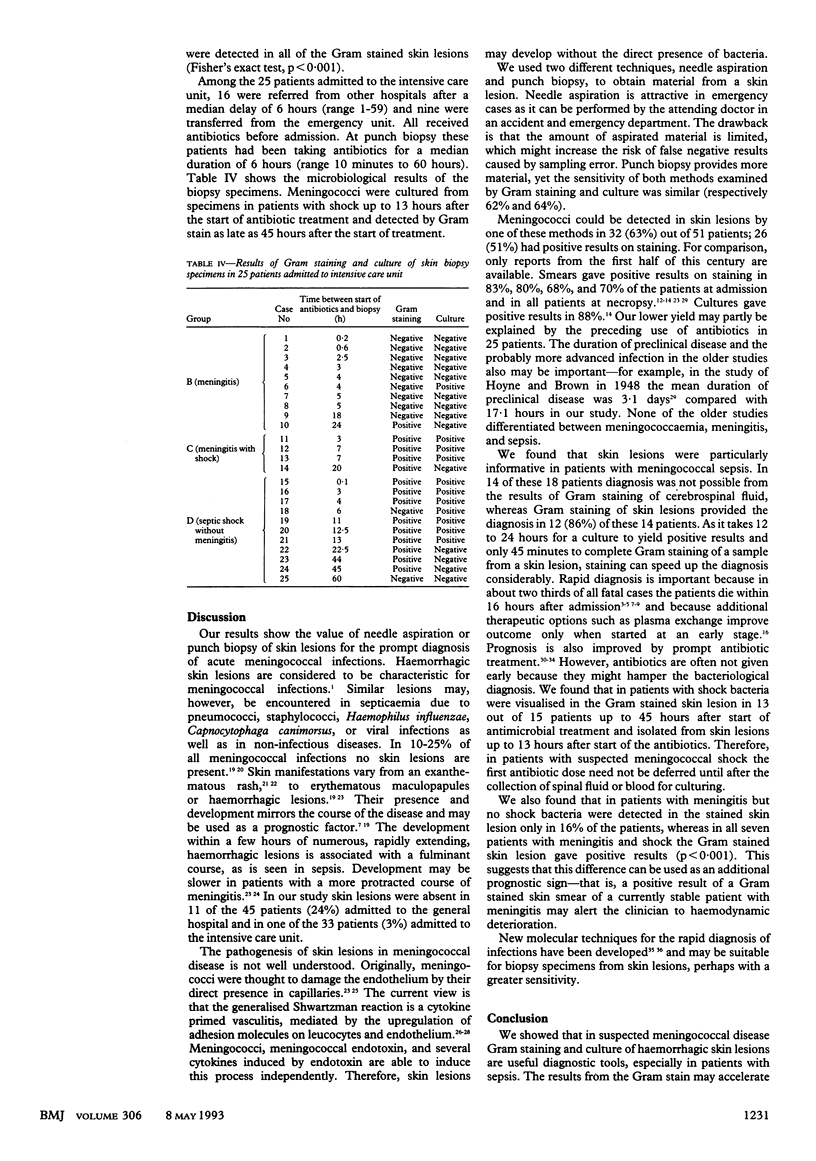
OBJECTIVES--To evaluate the usefulness of Gram staining and culture of skin lesions in patients with acute meningococcal infections. DESIGN--Retrospective study. SETTING--Community hospital and intensive care unit of a teaching hospital. SUBJECTS--51 patients admitted from 1989 to 1993 with proved meningococcal infections and microbiological examination of specimens from skin lesions. INTERVENTIONS--Needle aspiration of a skin lesion before start of antibiotic treatment in 26 patients in the community hospital; punch biopsy of skin lesion after start of antibiotic treatment in 25 patients in the teaching hospital. MAIN OUTCOME MEASURES--Detection of meningococci by Gram staining of specimens from skin lesions according to category of infection (meningococcaemia, meningitis, meningitis with shock, or septic shock without meningitis). RESULTS--Bacteria were detected in the specimen from haemorrhagic skin lesions by culture or Gram staining, or both in 32 (63%) patients. The sensitivity of the Gram stain was 51% and did not differ significantly from its sensitivity in detecting bacteria in cerebrospinal fluid. In meningococcal sepsis, however, a Gram stained skin lesion was significantly more sensitive (72%) than Gram stained cerebrospinal fluid (22%). In patients with meningitis skin lesions gave positive results on staining more often if shock was present. The results for punch biopsy specimens were not affected by antibiotics as Gram staining gave positive results up to 45 hours after the start of treatment and culture gave positive results up to 13 hours. CONCLUSION--Microbiological examination of skin lesions is informative, especially in patients with sepsis and inconclusive results from cerebrospinal fluid, and may provide a diagnosis in such patients within 45 minutes. It differentiates well between meningitis with and without haemodynamic complications, and the result is not affected by previous antibiotic treatment.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Argenbright L. W., Barton R. W. Interactions of leukocyte integrins with intercellular adhesion molecule 1 in the production of inflammatory vascular injury in vivo. The Shwartzman reaction revisited. J Clin Invest. 1992 Jan;89(1):259–272. doi: 10.1172/JCI115570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begg N. Reducing mortality from meningococcal disease. BMJ. 1992 Jul 18;305(6846):133–134. doi: 10.1136/bmj.305.6846.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bone R. C., Fisher C. J., Jr, Clemmer T. P., Slotman G. J., Metz C. A., Balk R. A. Sepsis syndrome: a valid clinical entity. Methylprednisolone Severe Sepsis Study Group. Crit Care Med. 1989 May;17(5):389–393. [PubMed] [Google Scholar]
- Brandtzaeg P., Dahle J. S., Høiby E. A. The occurrence and features of hemorrhagic skin lesions in 115 cases of systemic meningococcal disease. NIPH Ann. 1983 Dec;6(2):183-90, 202-3. [PubMed] [Google Scholar]
- Cahalane S. F., Waters M. Fulminant meningococcal septicaemia. A hospital experience. Lancet. 1975 Jul 19;2(7925):120–121. doi: 10.1016/s0140-6736(75)90017-3. [DOI] [PubMed] [Google Scholar]
- Corey L., Whitley R. J., Stone E. F., Mohan K. Difference between herpes simplex virus type 1 and type 2 neonatal encephalitis in neurological outcome. Lancet. 1988 Jan 2;1(8575-6):1–4. doi: 10.1016/s0140-6736(88)90997-x. [DOI] [PubMed] [Google Scholar]
- Dahle J. S. Pathogenesis of hemorrhagic skin lesions in meningococcal disease. NIPH Ann. 1983 Jun;6(1):49–53. [PubMed] [Google Scholar]
- Davis C. E., Arnold K. Role of meningococcal endotoxin in meningococcal purpura. J Exp Med. 1974 Jul 1;140(1):159–171. doi: 10.1084/jem.140.1.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emparanza J. I., Aldamiz-Echevarria L., Perez-Yarza E. G., Larrañaga P., Jiminez J. L., Labiano M., Ozcoidi I. Prognostic score in acute meningococcemia. Crit Care Med. 1988 Feb;16(2):168–169. doi: 10.1097/00003246-198802000-00015. [DOI] [PubMed] [Google Scholar]
- Gedde-Dahl T. W., Høiby E. A., Eskerud J. R. Unbiased evidence on early treatment of suspected meningococcal disease. Rev Infect Dis. 1990 Mar-Apr;12(2):359, 361-4. doi: 10.1093/clinids/12.2.359-a. [DOI] [PubMed] [Google Scholar]
- Giraud T., Dhainaut J. F., Schremmer B., Regnier B., Desjars P., Loirat P., Journois D., Lanore J. J. Adult overwhelming meningococcal purpura. A study of 35 cases, 1977-1989. Arch Intern Med. 1991 Feb;151(2):310–316. [PubMed] [Google Scholar]
- Halstensen A., Pedersen S. H., Haneberg B., Bjorvatn B., Solberg C. O. Case fatality of meningococcal disease in western Norway. Scand J Infect Dis. 1987;19(1):35–42. doi: 10.3109/00365548709032375. [DOI] [PubMed] [Google Scholar]
- Kilpi T., Anttila M., Kallio M. J., Peltola H. Severity of childhood bacterial meningitis and duration of illness before diagnosis. Lancet. 1991 Aug 17;338(8764):406–409. doi: 10.1016/0140-6736(91)91032-p. [DOI] [PubMed] [Google Scholar]
- Manios S. G., Kanakoudi F., Maniati E. Fulminant meningococcemia. Heparin therapy and survival rate. Scand J Infect Dis. 1971;3(2):127–133. doi: 10.3109/inf.1971.3.issue-2.06. [DOI] [PubMed] [Google Scholar]
- McGehee W. G., Rapaport S. I., Hjort P. F. Intravascular coagulation in fulminant meningococcemia. Ann Intern Med. 1967 Aug;67(2):250–260. doi: 10.7326/0003-4819-67-2-250. [DOI] [PubMed] [Google Scholar]
- Mercier J. C., Beaufils F., Hartmann J. F., Azéma D. Hemodynamic patterns of meningococcal shock in children. Crit Care Med. 1988 Jan;16(1):27–33. doi: 10.1097/00003246-198801000-00006. [DOI] [PubMed] [Google Scholar]
- Ni H., Knight A. I., Cartwright K., Palmer W. H., McFadden J. Polymerase chain reaction for diagnosis of meningococcal meningitis. Lancet. 1992 Dec 12;340(8833):1432–1434. doi: 10.1016/0140-6736(92)92622-m. [DOI] [PubMed] [Google Scholar]
- Niklasson P. M., Lundbergh P., Strandell T. Prognostic Factors in meningococcal disease. Scand J Infect Dis. 1971;3(1):17–25. doi: 10.3109/inf.1971.3.issue-1.03. [DOI] [PubMed] [Google Scholar]
- Rubenstein R., Esterly N. B. Meningococcal meningitis with a benign skin rash. Pediatr Dermatol. 1986 Nov;3(5):414–416. doi: 10.1111/j.1525-1470.1986.tb00553.x. [DOI] [PubMed] [Google Scholar]
- Sinclair J. F., Skeoch C. H., Hallworth D. Prognosis of meningococcal septicaemia. Lancet. 1987 Jul 4;2(8549):38–38. doi: 10.1016/s0140-6736(87)93067-4. [DOI] [PubMed] [Google Scholar]
- Strang J. R., Pugh E. J. Meningococcal infections: reducing the case fatality rate by giving penicillin before admission to hospital. BMJ. 1992 Jul 18;305(6846):141–143. doi: 10.1136/bmj.305.6846.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talan D. A., Hoffman J. R., Yoshikawa T. T., Overturf G. D. Role of empiric parenteral antibiotics prior to lumbar puncture in suspected bacterial meningitis: state of the art. Rev Infect Dis. 1988 Mar-Apr;10(2):365–376. doi: 10.1093/clinids/10.2.365. [DOI] [PubMed] [Google Scholar]
- Toews W. H., Bass J. W. Skin manifestations of meningococcal infection; an immediate indicator of prognosis. Am J Dis Child. 1974 Feb;127(2):173–176. doi: 10.1001/archpedi.1974.02110210023003. [DOI] [PubMed] [Google Scholar]
- Tompkins L. S. The use of molecular methods in infectious diseases. N Engl J Med. 1992 Oct 29;327(18):1290–1297. doi: 10.1056/NEJM199210293271808. [DOI] [PubMed] [Google Scholar]
- Tønjum T., Nilsson F., Bruun J. N., Haneberg B. The early phase of meningococcal disease. NIPH Ann. 1983 Dec;6(2):175–181. [PubMed] [Google Scholar]
- Waage A., Brandtzaeg P., Halstensen A., Kierulf P., Espevik T. The complex pattern of cytokines in serum from patients with meningococcal septic shock. Association between interleukin 6, interleukin 1, and fatal outcome. J Exp Med. 1989 Jan 1;169(1):333–338. doi: 10.1084/jem.169.1.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Deuren M., Santman F. W., van Dalen R., Sauerwein R. W., Span L. F., van der Meer J. W. Plasma and whole blood exchange in meningococcal sepsis. Clin Infect Dis. 1992 Sep;15(3):424–430. doi: 10.1093/clind/15.3.424. [DOI] [PubMed] [Google Scholar]


