Abstract and Introduction
Abstract
The problem of poor patient adherence has been extensively researched, but the rates of nonadherence have not changed much in the past 3 decades. Healthcare providers play a unique and important role in assisting patients' healthy behavior changes. We conducted a narrative review of the current literature to help providers become more familiar with proven interventions that can enhance patient adherence. We then grouped the interventions into categories that can be remembered by the mnemonic “SIMPLE”:
Simplifying regimen characteristics;
Imparting knowledge;
Modifying patient beliefs;
Patient communication;
Leaving the bias; and
Evaluating adherence.
Chronic lifestyle behavior change often requires a combination of all the aforementioned strategies. We suggest a conceptual framework, which calls for a multidisciplinary approach with the above strategies in the context of a healthcare team and system-related factors. We hope that this framework would not only help design scientifically proven interventions, but also reduce the time and cost involved with implementing these strategies in a healthcare setting.
Introduction
The problem of poor adherence to medical treatment is a well-recognized problem in the literature.[1–4] Studies have shown that in the United States alone, nonadherence to medications causes 125,000 deaths annually and accounts for 10% to 25% of hospital and nursing home admissions.[5] This makes nonadherence to medications one of the largest and most expensive disease categories. Moreover, patient nonadherence is not limited to medications alone. It can also take many other forms; these include the failure to keep appointments, to follow recommended dietary or other lifestyle changes, and to follow other aspects of treatment or recommended preventive health practices. Hence, the actual implications of nonadherence go far beyond the financial aspect of medication nonadherence, as estimated above.
Over the last few years, various constructs of adherence have been conceptualized, and extensive research on the efficacy of adherence-enhancing strategies has been performed. One significant development has been the inclusion of the patient in the determination and success of therapy, with the term “adherence” seeming to indicate this action more accurately than “compliance.”[6] However, the rates of nonadherence have not changed much over the past 3 decades. Recent reviews have shown that as many as 40% of patients still do not adhere to their treatment regimens.[7,8]
One possible reason could be the lack of consensus guidelines on this issue. Many of the studies and reviews done have been narrowly focused on one disease condition or one kind of adherence-enhancing strategy. Although this may be useful in a research setting, this fragmented approach may not be practical for healthcare providers dealing with a diverse patient population.[9] In addition, most of the literature on patient adherence has been published in social science journals rather than in the medical literature. This study provides a current review of critical adherence-enhancing interventions across a broad spectrum of patients and diseases and suggests an integrated framework to facilitate their implementation in clinical settings.
Methods
We identified original studies by searching MEDLINE (1990–2002) through Ovid with the MeSH headings “patient compliance” or “treatment refusal” and at least one of the following keywords: “intervention studies,” “prospective studies,” “outcome assessment,” “patient education,” “health promotion,” and “patient dropouts.” Bibliographies of relevant articles were searched to identify studies that might have been missed in the review.
Results
The individual studies were too clinically heterogeneous and methodologically variable to justify a quantitative meta-analysis. Hence, we chose to do a qualitative synthesis and group the studies into 6 broad categories on the basis of the type of intervention used to address nonadherence (see Table 1). This broader focus emphasizes certain common strategies that need to be addressed with respect to all patient-related conditions regardless of their causes.[10] The categories that are described below can be remembered by the mnemonic “SIMPLE.”
Table 1.
Some Commonly Used Interventions in Successful Adherence-Enhancing Strategies
| Strategies | Specific Interventions |
|---|---|
| Simplifying regimen characteristics | Adjusting timing, frequency, amount, and dosage |
| Matching to patients' activities of daily living | |
| Using adherence aids, such as medication boxes and alarms | |
| Imparting knowledge | Discussion with physician, nurse, or pharmacist |
| Distribution of written information or pamphlets | |
| Accessing health-education information on the Web | |
| Modifying patient beliefs | Assessing perceived susceptibility, severity, benefit, and barriers |
| Rewarding, tailoring, and contingency contracting | |
| Patient and family communication | Active listening and providing clear, direct messages |
| Including patients in decisions | |
| Sending reminders via mail, email, or telephone | |
| Convenience of care, scheduled appointment | |
| Home visits, family support, counseling | |
| Leaving the bias | Tailoring the education to patients' level of understanding |
| Evaluating adherence | Self-reports (most commonly used) |
| Pill counting, measuring serum or urine drug levels |
Simplifying Regimen Characteristics
We have known for some time that the complexity of a treatment regimen can affect adherence. Many of the strategies used to simplify a regimen have already become well-standardized practices. For example, adherence improves remarkably when a patient is prescribed a pill that can be taken once a day.[11] This can be done with a longer acting drug (wherever possible) or with a pill that has more than 1 drug. When a drug regimen cannot be reduced in frequency, it should be matched to the patient's activities of daily living. For example, patients are more likely to remember to take a pill before a meal or before going to sleep. Or, the regimen can be broken down into less complex stages that can be introduced sequentially. However, it is important to note that patients often misinterpret common instructions. Eraker and colleagues,[12] for example, found that only 36% of patients correctly interpreted the meaning of “every 6 hours.” Thus, it is important for physicians to use simple, everyday language and have the patient repeat the instructions to ensure proper understanding. Elderly patients are a particular concern because of their common deficits in physical dexterity, cognitive skills and memory, and the number of medications that they are typically prescribed. A variety of adherence aids are available to help patients organize their medications (eg, medication boxes) and remember dose times (alarms). Microelectronic devices can provide feedback that shows patients whether they have been taking their medications as prescribed.[13] Patients can also use devices designed to improve physical dexterity when applying topical preparations, administering insulin injections, operating pressurized inhalers, and administering eye drops. Such devices can help them place drops into their eyes or obviate the need to squeeze an eye drop container.[14]
Imparting Appropriate Knowledge
Research has consistently demonstrated that patients' understanding of their conditions and treatments is positively related to adherence,[15] and that adherence, satisfaction, recall, and understanding are all related to the amount and type of information given.[16]
Many studies have shown that patients do not always understand prescription instructions and often forget considerable portions of what healthcare practitioners tell them.[17,18] Studies have shown that patients who understand the purpose of the prescription are twice more likely to fill it than those who do not understand the purpose.[19]
According to Katz,[20] physicians can provide effective patient education by (1) limiting instructions to 3 or 4 major points during each discussion; (2) using simple, everyday language, especially when explaining diagnosis and giving instructions; (3) supplementing oral teaching with written materials; (4) involving the patient's family members and friends; and (5) reinforcing the concepts discussed.[20] This is especially true for millions of citizens with low literacy skills.
Modifying Beliefs and Human Behavior
For interventions that are complex and require lifestyle modifications, it is worthwhile to address patients' beliefs, intentions, and self-efficacy (perceived ability to perform action). This is because knowledge alone is not sufficient to enhance adherence in recommendations involving complex behavior change.[21,22,23]
Clinicians can optimize behavior change by ensuring that the patients (1) perceive themselves to be at risk due to lack of adoption of healthy behavior (perceived susceptibility), (2) perceive their medical conditions to be serious (perceived severity), (3) believe in the positive effects of the suggested treatment (perceived benefits), (4) have channels to address their fears and concerns (perceived barriers), and (5) perceive themselves as having the requisite skills to perform the healthy behavior (self-efficacy).
Thus, by knowing which of these beliefs is below a level presumed necessary for good adherence, the provider may tailor interventions to suit the unique needs of each patient.[24]
Patient Communication
Patient communication encompasses interventions ranging from physician-patient communication, sending mail or telephonic reminders, to involving patients' families in the dialogue. Of these, the most problematic is physician-patient communication. At least 50% of patients leave their doctors' offices not knowing what they have been told. Studies have shown that (1) 50% of psychosocial and psychiatric problems are missed by physicians due to lack of proper communication[25]; (2) physicians interrupt patients on an average of 18 seconds into the patients' descriptions of the presenting problems[26]; (3) 54% of patients' problems and 45% of patient concerns are neither elicited by the physician nor disclosed by the patient[27]; and (4) 71% of patients stated poor relationships as a reason for their malpractice claims.[28]
Rosenberg and associates[29] devised the following suggestions after conducting a comprehensive review of the existing physician-patient communication literature in books and articles:
Ask a patient about his feelings and concerns (in addition to physical aspects of the problem) and his view about psychological factors on the adherence, so as to arrive at a common understanding to the nature of the problem. Then provide them with information about all areas that [that] individual finds pertinent, and encourage them to share in decision making when a plan for management is formulated.
Most importantly, successful collaboration requires tailoring strategies to individual patients rather than basing communication on general assumptions.[30]
On the same note, communication with the patient's family and the patient's own perception of social support are significantly and positively related to adherence.[31–33] The family's role becomes all the more important if a patient is suffering from a chronic disabling condition requiring continued support and understanding.
Leaving the Bias
Much of the early literature in adherence research focused on demographic factors and personality traits that supposedly caused or led to poor adherence. In a review of 185 studies, Haynes[34] found no clear relationship between adherence and race, sex, educational experience, intelligence, marital status, occupational status, income, and ethnic or cultural background. Although some studies have found a correlation of adherence with sex and education,[35] it is believed that this effect is small and may be overcome by tailoring the education to the patient's level of understanding. Moreover, the fact that an individual's level of adherence may vary over time and between different aspects of treatment proves that demographic factors play a minor role in adherence behavior, if at all.[36,37]
Evaluating Adherence
Of note, doctors uniformly underestimate the problem of nonadherence in their patients.[38,39] If a healthcare professional is unable to detect nonadherence, it is impossible for him or her to correct the problem. Hence, it becomes imperative to measure and evaluate patient adherence reliably. This can be done by self-reports, pill counting, and in some cases measuring serum or urine drug levels. Of these, self-report is the most practical and widely used tool. In general, patients can be very accurate in reporting whether they are adhering to their treatment regimens if they are asked simply and directly.[40] Moreover, regular assessment of patient adherence by itself can lead to increased patient adherence.[29]
A simple, 4-item questionnaire designed by Morisky and colleagues[41] was effective in assessing and predicting adherence in 290 hypertensive patients who had been receiving care for their high blood pressure for 6 years.
The questions asked were:
Do you ever forget to take your medications?
Are you careless at times about taking medications?
When you feel better, do you sometimes stop taking medications?
Sometimes, when you feel worse, do you stop taking your medicine?
Each yes answer was scored with a 0 and each no answer was scored with a 1. The reliability of the scale was found to be .61 with a sensitivity of .81 and specificity of .44.
A Conceptual Framework to Address Patient Nonadherence
The aforementioned strategies have been proven to enhance patient adherence in multiple studies and can have huge implications for cost-savings and improved patient outcomes.[42] The average unweighted effect size for such interventions has been calculated to be around .23.[21] In terms of binomial effect-size display, this difference of 23% may be interpreted as a “success rate” of 62% in intervention subjects vs 38% in control subjects. Although these results are encouraging, the challenge still remains over how to implement and operationalize these strategies in a modern-day busy practice where clinicians are constrained by limited time and budget. To compound this problem, there is no single intervention strategy that has been shown to be effective across all conditions and settings, and hence a combination of the above strategies is often required to make a meaningful difference to patients' adherence[21,43] (see Table 1). To bridge this gap between research and clinical reality, we propose a conceptual framework based on our literature review and the recommendations adopted by some of the leading organizations.[8,44,45] This framework is based on a multidisciplinary approach, which looks at the strategies in the context of healthcare team and system-related factors to help reduce the time and cost involved with implementing these strategies (see Figure 1). The framework considers patient adherence not as a patient or physician issue but as a systems problem and helps integrate the strategies at the systems level. In the framework nurses, pharmacists, case managers, health educators, and others involved in patient care are aware of one another's responsibilities and have an important role to play. For example, understanding and accepting the role that a pharmacist plays in imparting medication-related knowledge to patients may help clinicians to focus on other aspects of the treatment plan. The community pharmacist can help increase adherence to drug regimens by providing patients with additional information about individual drugs, identifying potential adverse drug reactions and interactions, and supplying appropriate drug containers or compliance aids.[46] Similarly, interventions, such as mailing appointment reminders and patient-education materials, may be accomplished by nurses or other healthcare staff. The framework also implies that adherence is a dynamic process that needs to be extensively evaluated. Closing the feedback loop relies on good evaluation, which in turn entails defining specific criteria to measure adherence as well as assessing both the processes and outcomes of an initiative. Developing institutional-wide committees to plan and operationalize the strategies would help incorporate the guidelines smoothly into the existing systems and make them a part of continuous quality-improvement initiatives.
Figure 1.
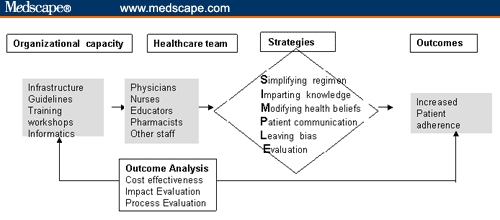
Framework to implement critical adherence-enhancing strategies with a systems approach.
Conclusion
Patient adherence is a complex issue leading to huge burden on our healthcare system. Although strategies to enhance patient adherence exist in the literature, they are often too complex and not practicable for busy practicing physicians. We have provided a simplistic overview of methodologically proven adherence-enhancing strategies so that the research can be translated and applied to patient care settings. Involving multiple stakeholders and other healthcare providers, in addition to physicians, may help reduce the time and cost involved with implementing these strategies.
Contributor Information
Ashish Atreja, Medical Informatics, Department of General Internal Medicine, Cleveland Clinic Foundation, Cleveland, Ohio, atrejaa@ccf.org.
Naresh Bellam, Department of Internal Medicine, University of Alabama at Birmingham.
Susan R. Levy, Community Health Sciences, University of Illinois at Chicago.
References
- 1.Haynes RB. Introduction. In: Haynes RB, Taylor DW, Sackett DL, editors. Compliance in Health Care. Baltimore, Md: Johns Hopkins University Press; 1979. pp. 1–18. [Google Scholar]
- 2.Fawcett J. Compliance: definitions and key issues. J Clin Psychiatry. 1995;56(suppl1):4–8. [PubMed] [Google Scholar]
- 3.Davis MS. Variation in patients' compliance with doctors' orders: medical practice and doctor-patient interaction. Psychiatry Med. 1971;2:31–54. doi: 10.2190/kmpk-19ta-gek8-bftm. [DOI] [PubMed] [Google Scholar]
- 4.Blackwell B. Drug therapy: patient compliance. N Engl J Med. 1973;289:249–252. doi: 10.1056/NEJM197308022890506. [DOI] [PubMed] [Google Scholar]
- 5.Smith DL. Compliance packaging: a patient education tool. Am Pharm. 1989;NS29(2):42–45. 49–53. doi: 10.1016/s0160-3450(15)31856-0. [DOI] [PubMed] [Google Scholar]
- 6.Tilson HH. Adherence or compliance? Changes in terminology. Ann Pharmacother. 2004;38:161–162. doi: 10.1345/aph.1D207. [DOI] [PubMed] [Google Scholar]
- 7.Dunbar-Jacob J, Burke LE, Puczynski S. Clinical assessment and management of adherence to medical regimens. In: Nicassio M, Smith T, editors. Managing Chronic Illness: A Biophysical Perspective. Washington, DC: American Psychological Association; 1995. pp. 313–341. [Google Scholar]
- 8.Haynes RB, McDonald H, Garg AX, Montague P. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2002;(2):CD000011. doi: 10.1002/14651858.CD000011. [DOI] [PubMed] [Google Scholar]
- 9.Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med. 2002;22:267–284. doi: 10.1016/s0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]
- 10.Dunbar-Jacob J, Erlen JA, Schlenk EA, Ryan CM, Sereika SM, Doswell WM. Adherence in chronic disease. Annu Rev Nurs Res. 2000;18:48–90. [PubMed] [Google Scholar]
- 11.Morningstar BA, Sketris IS, Kephart GC, Sclar DA. Variation in pharmacy prescription refill adherence measures by type of oral antihyperglycaemic drug therapy in seniors in Nova Scotia, Canada. J Clin Pharm Ther. 2002;27:213–220. doi: 10.1046/j.1365-2710.2002.00411.x. [DOI] [PubMed] [Google Scholar]
- 12.Eraker SA, Kirscht JP, Becker MH. Understanding and improving patient compliance. Ann Intern Med. 1984;100:258–268. doi: 10.7326/0003-4819-100-2-258. [DOI] [PubMed] [Google Scholar]
- 13.Cramer JA. Enhancing patient compliance in the elderly. Role of packaging aids and monitoring. Drugs Aging. 1998;12:7–15. doi: 10.2165/00002512-199812010-00002. [DOI] [PubMed] [Google Scholar]
- 14.Rivers PH. Compliance aids – do they work? Drugs Aging. 1992;2:103–111. doi: 10.2165/00002512-199202020-00004. [DOI] [PubMed] [Google Scholar]
- 15.Burgoon JK, Pfau M, Parrott R, Birk T, Coker R, Burgoon M. Relational communication, satisfaction, compliance gaining strategies and compliance in communication between physicians and patients. Commun Monogr. 1987;54:307–324. [Google Scholar]
- 16.Hall JA, Roter DL, Katz NR. Meta-analysis of correlates of provider behavior in medical encounters. Med Care. 1988;26:657–675. doi: 10.1097/00005650-198807000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Sarriff A, Aziz NA, Hassan Y, Ibrahim P, Darwis Y. A study of patients' self-interpretation of prescription instructions. J Clin Pharm Ther. 1992;17:125–128. doi: 10.1111/j.1365-2710.1992.tb01280.x. [DOI] [PubMed] [Google Scholar]
- 18.Ley P, Llewellyn S. Improving patients understanding, recall, satisfaction and compliance. In: Broome A, Llewelyn S, editors. Heart Psychology: Processes and Applications. 2nd ed. London, United Kingdom: Chapman & Hall; 1995. [Google Scholar]
- 19.Daltroy LH, Katz JN, Morlino CI, Liang MH. Improving doctor patient communication. Psychiatr Med. 1991;2:31–35. [Google Scholar]
- 20.Katz JR. Back to basics: providing effective patient teaching. Am J Nurs. 1997;97:33–36. [PubMed] [Google Scholar]
- 21.Roter DL, Hall JA, Merisca R, Nordstrom B, Cretin D, Svarstad B. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36:1138–1161. doi: 10.1097/00005650-199808000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Raynor DK, Booth TG, Blenkinsopp A. Effects of computer generated reminder charts on patients' compliance with drug regimens. BMJ. 1993;306:1158–1161. doi: 10.1136/bmj.306.6886.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee S, Wing YK, Wong KC. Knowledge and compliance towards lithium therapy among Chinese psychiatric patients in Hong Kong. Aust N Z J Psychiatry. 1992;26:444–449. doi: 10.3109/00048679209072068. [DOI] [PubMed] [Google Scholar]
- 24.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 25.Davenport S, Goldberg D, Millar T. How psychiatric disorders are missed during medical consultations. Lancet. 1987;2:439–441. doi: 10.1016/s0140-6736(87)90970-6. [DOI] [PubMed] [Google Scholar]
- 26.Frankel R, Beckman H. Evaluating the patient's primary problem(s) In: Stewart M, Roter D, editors. Communicating With Medical Patients. Newbury Park, Calif: Sage Publications; 1989. pp. 86–98. [Google Scholar]
- 27.Stewart MA, McWhinney IR, Buck CW. The doctor/patient relationship and its effect upon outcome. J R Coll Gen Pract. 1979;29:77–81. [PMC free article] [PubMed] [Google Scholar]
- 28.Levinson W. Physician-patient communication. A key to malpractice prevention. JAMA. 1994;272:1619–1620. [PubMed] [Google Scholar]
- 29.Rosenberg EE, Lussier MT, Beaudoin C. Lessons for clinicians from physician-patient communication literature. Arch Fam Med. 1997;6:279–283. doi: 10.1001/archfami.6.3.279. [DOI] [PubMed] [Google Scholar]
- 30.Morrow D. Improving consultations between health-care professionals and older clients: implications for pharmacists. Int J Aging Hum Dev. 1997;44:47–72. doi: 10.2190/GQX9-F4UJ-5RQ2-N1YD. [DOI] [PubMed] [Google Scholar]
- 31.Conn VS, Taylor SG, Casey B. Cardiac rehabilitation program participation and outcomes after myocardial infarction. Rehabil Nurs. 1992;17:58–62. doi: 10.1002/j.2048-7940.1992.tb01513.x. [DOI] [PubMed] [Google Scholar]
- 32.Morisky DE, DeMuth NM, Field-Fass M, Green LW, Levine DM. Evaluation of family health education to build social support for long-term control of high blood pressure. Health Educ Q. 1985;12:35–50. doi: 10.1177/109019818501200104. [DOI] [PubMed] [Google Scholar]
- 33.Waren L, Hixenburgh P. Psychosocial needs and experiences of adults with diabetes: their relationship to regimen adherence from the patient perspective. Proc Psychol Soc. 1995;4:39. [Google Scholar]
- 34.Haynes RB. Introduction. In: Haynes RB, Taylor DW, Sackett DL, editors. Compliance in Health Care. Baltimore, Md: Johns Hopkins University Press; 1979. pp. 1–18. [Google Scholar]
- 35.Blake PG, Korbet SM, Blake R, et al. A multicenter study of noncompliance with continuous ambulatory peritoneal dialysis exchanges in US and Canadian patients. Am J Kidney Dis. 2000;35:506–514. doi: 10.1016/s0272-6386(00)70205-8. [DOI] [PubMed] [Google Scholar]
- 36.Cleary DJ, Matzke GR, Alexander AC, Joy MS. Medication knowledge and compliance among patients receiving long-term dialysis. Am J Health Syst Pharm. 1995;52:1895–1900. doi: 10.1093/ajhp/52.17.1895. [DOI] [PubMed] [Google Scholar]
- 37.Hilbrands LB, Hoitsma AJ, Koene RA. Medication compliance after renal transplantation. Transplantation. 1995;60:914–920. [PubMed] [Google Scholar]
- 38.Roth HP, Caron HS. Accuracy of doctors' estimates and patients' statements on adherence to a drug regimen. Clin Pharmacol Ther. 1978;23:361–370. doi: 10.1002/cpt1978233361. [DOI] [PubMed] [Google Scholar]
- 39.Brody DS. An analysis of patient recall of their therapeutic regimens. J Chronic Dis. 1980;33:57–63. doi: 10.1016/0021-9681(80)90086-7. [DOI] [PubMed] [Google Scholar]
- 40.Duong M, Piroth L, Grappin M, et al. Evaluation of the Patient Medication Adherence Questionnaire as a tool for self-reported adherence assessment in HIV-infected patients on antiretroviral regimens. HIV Clin Trials. 2001;2:128–135. doi: 10.1310/M3JR-G390-LXCM-F62G. [DOI] [PubMed] [Google Scholar]
- 41.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 42.Levy RA. Improving compliance with prescription medications: an important strategy for containing health-care costs. Med Interface. 1989;(March):34–37. [Google Scholar]
- 43.Wagner EH, Grothaus LC, Sandhu N, et al. Chronic care clinics for diabetes in primary care: a system-wide randomized trial. Diabetes Care. 2001;24:695–700. doi: 10.2337/diacare.24.4.695. [DOI] [PubMed] [Google Scholar]
- 44.Miller NH, Hill MN, Kotke T, Ockene I. The multilevel compliance challenge: recommendations for a call to action. Circulation. 1997;95:1085–1090. doi: 10.1161/01.cir.95.4.1085. [DOI] [PubMed] [Google Scholar]
- 45.World Health Organization. Adherence to long-term therapies: evidence for action World Health Organization. 2003 Available at: http://www.who.int/entity/chronic_conditions/en/adherence_report.pdf" Accessed December 15, 2004.
- 46.Denham MJ, Barnett NL. Drug therapy and the older person: role of the pharmacist. Drug Saf. 1998;19:243–250. doi: 10.2165/00002018-199819040-00001. [DOI] [PubMed] [Google Scholar]


