Abstract and Introduction
Abstract
Brain metastases from cervical carcinomas are extremely rare. We report a patient with squamous cell carcinoma of the cervix who developed an isolated left parietooccipital lobe metastasis within 4 months of treatment of the primary disease. The presenting symptoms of the metastatic disease were visual disturbance, headache, and vomiting. The patient was successfully treated by surgical excision of the metastasis and adjuvant whole brain radiation therapy, and she was disease-free at the 6-month follow-up after treatment of the recurrence.
Introduction
Cervical cancer is the most common malignancy in Indian women, with an annual incidence of approximately 100,000 cases. Cervical cancers usually spread by local extension and through the lymphatics to the retroperitoneal lymph nodes. Metastases to the central nervous system from cervical cancer are extremely rare. They are usually seen late in the course of the disease, and have poor prognosis. Due to the rarity of this event, there are very few reports in the literature regarding the optimal management and prognosis of these patients. We report the case of a woman with squamous cell carcinoma of the cervix, with a left parietooccipital lobe metastasis, who was managed successfully. A summary of the relevant literature is also presented.
Case Report
A 54-year-old woman came to observation on July 2003 with a complaint of postmenopausal bleeding per vaginum for 2 months. She had entered menopause 8 years earlier. Her general and systemic exams were within normal limits. Pelvic examination revealed an ulceroproliferative cervical growth, with involvement of the vaginal fornices and the upper half of the anterior vaginal wall. A biopsy of the lesion showed a poorly differentiated squamous cell carcinoma. After a thorough clinicoradiologic workup, the disease was staged as FIGO stage-IIa. The patient was treated with concurrent chemoradiation. She was given 40 Gy by external beam radiation and 33.5 Gy by brachytherapy. Intravenous cisplatin at a dose of 40 mg/m2 per week was also given during the entire course of radiation therapy. The treatment was completed in August 2003, and the patient attained complete remission. The patient remained asymptomatic for 4 months after completion of treatment.
In December 2003, she experienced sudden-onset visual disturbance with difficulty in seeing the objects on the right side of her field of vision. This was soon followed by difficulties in walking, headache, and vomiting. A magnetic resonance imaging (MRI) scan of the brain revealed a 5- × 3.8-cm lesion in the left posterior parietal and occipital regions, associated with extensive brain edema (Figures 1 and 2). The metastatic workup, including computed tomographic (CT) scans of the thorax, abdomen, and pelvis, did not reveal other metastases. The positron emission tomographic (PET) scan was normal, except for the site of the brain metastasis.
Figure 1.
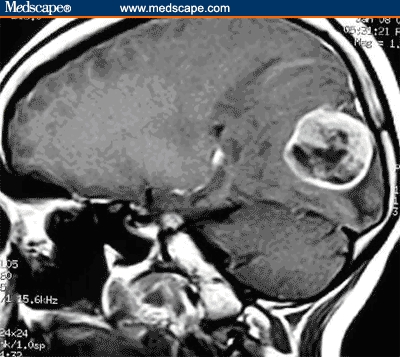
MRI of the patient's brain (sagittal view) showing a metastasis in the left parietooccipital region.
Figure 2.

MRI of the patient's brain showing a metastasis in the left parietooccipital region.
In view of the localized nature of the lesion, surgical excision of the tumor was planned. Following a left occipital craniotomy with excision of the tumor, the postoperative recovery of the patient was uneventful. Histologic examination of the mass showed “metastasis from poorly differentiated squamous cell carcinoma consistent with known primary in the cervix.” Postoperatively, 30 Gy to the whole brain, with a 10-Gy boost to the posterior fossa, were given as adjuvant radiation therapy. At 6 months, following the treatment of brain metastasis, the patient is asymptomatic and free of disease.
Discussion
The overall incidence of brain metastases from various malignant tumors can vary from 13.5% to 37%.[1] The lungs, breasts, kidneys, and gastrointestinal tract are the most frequent sites resulting in brain metastases.[1] Gynecologic malignancies, on the other hand, usually have a low propensity to metastasize to the brain. The gynecologic tumor that most frequently metastasizes to the brain is choriocarcinoma, which yields up to 35% of all brain metastases in this group.[2] Brain metastases from cervical cancer are extremely rare. However, an increase in the incidence of brain metastases from cervical cancer has been noted in recent years. This increase may be related to an improved treatment of the primary lesions and, thus, a better survival of these patients.[3]
Henriksen[4] first reported brain metastases from cervical carcinoma in an autopsy study, in 1949. Few reports have been published since then on this clinical entity. The incidence of brain metastases in this setting has been reported to be about .5% to 1.2% in various clinical studies.[5,6]
The route of spread to the brain from cervical cancer is hematogenous. However, the presence of intravascular tumor cells in the cerebral circulation does not always lead to the development of brain metastases. The development of brain metastases depends on the host immune response, tissue neovascularization, the number of tumor emboli, and characteristics of the tumor.[7] Brain metastases are more frequently seen with poorly differentiated cervical tumors. In our case, both the primary and metastatic tumors had poorly differentiated histologies.
Neuroendocrine carcinomas of the cervix, which represent a rare and aggressive type of tumor, show an increased incidence of metastasis in the central nervous system. Weed and colleagues,[8] in a retrospective study of 15 cases of neuroendocrine carcinomas of the cervix, reported the presence of brain metastases in 5 cases (33%). Based on this and other reports, they suggested a possible benefit from prophylactic whole brain radiation to prevent central nervous system metastasis in these cases. More than 80% of brain metastases are located in the supratentorial region of the brain, a phenomenon that may be related to the vascularity and the spatial characteristics of this region. Also, in our case the tumor was located in the supratentorial region.
The reported interval between the initial diagnosis of cervical cancer and presentation of the brain metastasis is variable in different cases, ranging from the time of first diagnosis of the primary tumor to 8 years, with an overall mean of 3 months.[9] Although the clinical presentation of a patient with brain metastasis is likely to depend on the site of the lesion, headache and hemiparesis are the most commonly reported symptoms and signs in this setting.[10] The metastatic tumor, the surrounding tissue edema, or both is responsible for the neurologic symptoms. In this case, because the lesion was located in the left occipital lobe, a disturbance of the visual field was the main presenting symptom. In most of the reported cases, symptoms are sudden in onset and appear severe, as seen in our case.
The treatment of brain metastasis usually involves radiation therapy, surgery, or both, depending on the clinical situation. In general, surgical excision is done in those cases with a solitary lesion or adjacent multiple metastases, cases with diagnostic uncertainty, or with life-threatening and critically located metastases. Patients with nonadjacent, multiple, or inoperable lesions are usually treated with palliative whole brain radiotherapy. Surgical excision of the solitary lesion combined with adjuvant postoperative radiotherapy yields a better survival than radiotherapy alone.[11] Radiation surgery, stereotactic radiation therapy, and chemotherapy have also been used for the management of brain metastases with variable success. Overall, however, the prognosis of cervical cancer patients with brain metastases is frequently poor. Most studies have reported a median survival of only a few months, but there are a few anecdotal reports of long-term, disease-free survival in these patients.[9]
In conclusion, our case provides an example of successful management of brain metastasis in a case of cervical carcinoma, with the use of surgery and adjuvant radiation therapy. This line of treatment should be strongly considered in patients of cervical carcinoma with solitary, resectable brain metastases.
Contributor Information
Maheshwari Amita, Genito-Urinary and Gynecologic Oncology services, Department of Surgery, Tata Memorial Hospital, Mumbai, India.
Gupta Sudeep, Department of Medical Oncology, Tata Memorial Hospital, Mumbai, India.
Wuntkal Rekha, Genito-Urinary and Gynecologic Oncology services, Department of Surgery, Tata Memorial Hospital, Mumbai, India.
Kulkarni Yogesh, Genito-Urinary and Gynecologic Oncology services, Department of Surgery, Tata Memorial Hospital, Mumbai, India.
Tongaonkar Hemant, Genito-Urinary and Gynecologic Oncology services, Department of Surgery, Tata Memorial Hospital, Mumbai, India.
References
- 1.Stortbecker TP. Metastatic tumors of the brain from a neurosurgical point of view: a follow-up of 158 cases. J Neurosurg. 1954;11:84–111. doi: 10.3171/jns.1954.11.1.0084. [DOI] [PubMed] [Google Scholar]
- 2.Yordan LL, Jr, Schlaerth J, Gaddis O, Morrow CP. Radiation therapy in the management of gestational choriocarcinoma metastatic to the central nervous system. Obstet Gynecol. 1987;69:627–630. [PubMed] [Google Scholar]
- 3.Lefkowitz D, Asconape J, Biller J. Intracranial metastases from carcinoma of the cervix. South Med J. 1983;76:519–521. doi: 10.1097/00007611-198304000-00032. [DOI] [PubMed] [Google Scholar]
- 4.Henriksen E. The lymphatic spread of carcinoma of the cervix and of the body of the uterus. Am J Obstet Gynecol. 1949;58:924–942. doi: 10.1016/0002-9378(49)90200-8. [DOI] [PubMed] [Google Scholar]
- 5.Cormio G, Pellegrino A, Landoni F, Regallo M, Zanetta G, Colombo A. Brain metastases from cervical carcinoma. Tumori. 1996;82:394–396. doi: 10.1177/030089169608200420. [DOI] [PubMed] [Google Scholar]
- 6.Saphner T, Gallion H, Nagell JR, Kryscio R, Patchell RA. Neurologic complications of cervical cancer. A review of 2261 cases. Cancer. 1989;64:1147–1151. doi: 10.1002/1097-0142(19890901)64:5<1147::aid-cncr2820640530>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 7.Nielsen SL, Posner JB. Brain metastasis localized to an area of infarction. J Neuro-Oncol. 1983;1:191–195. doi: 10.1007/BF00165602. [DOI] [PubMed] [Google Scholar]
- 8.Weed JC, Graff AT, Shoup B, Tawfik O. Small-cell undifferentiated (neuroendocrine) carcinoma of the uterine cervix. J Am Coll Surg. 2003;197:44–51. doi: 10.1016/S1072-7515(03)00120-0. [DOI] [PubMed] [Google Scholar]
- 9.Robinson JB, Morris M. Cervical carcinoma metastatic to the brain. Gynecol Oncol. 1997;66:324–326. doi: 10.1006/gyno.1997.4763. [DOI] [PubMed] [Google Scholar]
- 10.Kishi K, Nomura K, Miki Y, Shibui S, Takakura K. Metastatic brain tumors: a clinical and pathologic analysis of 101 cases with biopsy. Arch Pathol Lab Med. 1982;106:133–135. [PubMed] [Google Scholar]
- 11.Ikeda SI, Yamada T, Katsumata N, et al. Cerebral metastasis in patients with uterine cervical cancer. Jpn J Clin Oncol. 1998;28:27–29. doi: 10.1093/jjco/28.1.27. [DOI] [PubMed] [Google Scholar]


