Abstract and Introduction
Abstract
Background
Prevention programs often promote HIV testing as one possible strategy of combating the spread of the disease.
Objective
To examine levels of HIV testing practices among a large sample of university students and the relationship among HIV testing, sociodemographic variables, and HIV-related behaviors.
Methods
A total of 1252 students were surveyed between June 2001 and February 2002 using a 193-item questionnaire measuring a variety of HIV-related knowledge and attitudinal and behavioral items.
Results
Hierarchical logistic regression analyses revealed that youths, married persons, persons who had attended an HIV education forum, and those who knew someone with HIV/AIDS were more likely to report a previous HIV test. However, HIV testing was not associated with condom use or number of sex partners.
Conclusion
The lack of significant findings between testing and risky sexual behaviors should not negate the importance of HIV testing. Being informed regarding personal HIV serostatus is one of the first steps in self-protection. Effective messages and programs need to be developed and implemented in Jamaica to promote HIV testing and help persons to adequately assess their level of risk with respect to contracting HIV.
Introduction
Well into its third decade, the HIV/AIDS epidemic continues to pose a major public health challenge. Currently, UNAIDS estimates that 40 million persons are living with the disease worldwide and that there are more than 20 million related deaths.[1] The Caribbean region hosts the highest incidence rates for HIV/AIDS in the Americas and the second highest prevalence rates in the world among adults age 15–49 years. It is estimated that between 350,000 and 560,000 adults in the region are living with HIV, resulting in a prevalence rate of 2.3%.[1,2] In Jamaica, as of December 2003, 8097 cases of AIDS have been reported with more than 1000 new cases identified in 2003; an estimated 1.6% of the adult population is infected with HIV.[3] Even in light of a number of education campaigns and interventions, HIV/AIDS and other sexually transmitted infections (STIs) remain the second leading cause of death among males and females age 30–34 years in Jamaica.[3]
Prevention programs have been promoting HIV testing as one possible way to combat the spread of the disease.[4,5] This strategy is based on the premise that an awareness of the risk and severity of HIV will lead to HIV testing and protective behavior adoption.[6] However, research examining the relationship between HIV testing and subsequent protective behavior has found mixed results. Although some studies did find a significant relationship between awareness of one's HIV serostatus and protective sexual behaviors, others found no such relationship.[7–10]
When looking specifically at HIV testing behaviors among university students, a limited number of studies were identified. One study revealed that students seeking HIV testing were more likely to report previous unsafe vaginal and oral sex compared with non-test seekers.[11] However, those engaging in unprotected sex did not perceive themselves to be at risk of contracting HIV. Another study found similar results, with 40% describing sexual activities that placed them at some risk for HIV infection and other STIs.[12] With respect to predictors of HIV testing, one study found that age was significantly associated with testing; older students were more likely to seek testing than were younger students.[13] Another study focused on the psychosocial differences between those seeking a test and those who had never had a test. Those seeking testing perceived more benefits and fewer barriers and were ranked higher in consideration of future consequences. They were also at higher risk of becoming infected with HIV according to reports of risky sexual behavior as compared with those not seeking HIV testing.[14]
Very few Caribbean-based studies were identified that specifically examined predictors of testing or subsequent behaviors associated with testing. A study of Puerto Rican youth in drug treatment found that 66% of those enrolled in ambulatory drug treatment centers agreed to take an HIV test; volunteers, when compared with nonvolunteers, were more likely to be males who reported fewer years of education and engaged in risky sex and drug behaviors.[15] With respect to posttest behaviors, a study of adult drug users in Puerto Rico found that after receiving a positive test result, persons were significantly less likely to continue to engage in unprotected vaginal sex.[16] Another study of at-risk persons from Trinidad found that persons who received HIV testing and subsequent counseling decreased their high-risk sexual behaviors with nonprimary partners, but not with primary or steady partners.[17]
In an effort to identify studies that specifically targeted university students in the Caribbean for the purpose of measuring HIV-related attitudes and behaviors, only 1 published report was found. Survey data from 7000 university students in Puerto Rico revealed that students held attitudes that are associated with high-risk sexual behavior; furthermore, a number of students were engaging in risky sexual activities.[18] However, HIV testing was not addressed in the study.
Therefore, in an attempt to address the apparent gap in HIV testing research among university students in the Caribbean, we drew from research with other populations to develop an explanatory model to examine HIV testing. A hierarchical model was developed, using submodels that reflect the various factors hypothesized to be related to HIV testing. The following hypotheses were developed:
Submodel 1: Sociodemographic characteristics (age, sex, marital status, HIV education, HIV awareness) are directly related to perceived risk of HIV. Previous research indicates that perceived risk of HIV varies by sociodemographic characteristics.[17,19,20]
Submodel 2: Perceived risk of HIV is directly related to HIV testing. Perceived risk has been found in previous studies to be associated with HIV-testing behaviors.[21–24]
Submodels 3a-3c: HIV testing is directly related to sexual behaviors such as condom use and number of sex partners. Previous research has found associations between HIV testing and a number of HIV-related behaviors.[7–10]
Therefore, the present study seeks to identify the predictors of HIV testing (sociodemographics, perceived risk of HIV) and the role of HIV testing on sex-related behaviors (condom use, number of sex partners).
Methods
Data Collection
Data for these analyses were taken from the University of the West Indies HIV/AIDS Knowledge, Attitudes and Behaviors Study 2001/2002, a collaborative research effort between the University of the West Indies and the Ministry of Health, Kingston, Jamaica. A 193-item questionnaire was developed related to HIV/AIDS education and prevention. The questionnaire was based upon social-psychological theories of behavior change, including the Health Belief Model, Theory of Reasoned Action, and Social Cognitive Theory.[6,25,26] In addition, instruments from other universities conducting HIV research with students, the US Centers for Disease Control and Prevention (CDC), and the Ministry of Health, Jamaica, were used to facilitate the development and inclusion of standard questions that have been found to employ reliable and valid measures of HIV-related attitudes and behaviors across various samples.[27–30] Our survey instrument was reviewed and approved by the Research and Ethics Committee, Ministry of Health, and included items addressing knowledge of transmission, knowledge of risks associated with specific sexual behaviors, attitudes toward persons living with HIV/AIDS, HIV testing behaviors, sexual history, attitudes toward condoms and safer sex, sexual behaviors by steady and nonsteady sex partners, and drug and alcohol use during sexual activity.
The instrument was piloted with a sample of 15 students in order to assess the ease of completing the instrument, to determine whether the questions were easily understood, and to ensure that the instrument could be completed in a timely fashion. On the basis of the first piloting phase, revisions were made and the instrument was piloted again with 10 additional students. Following the results of the second piloting phase, minor revisions were made and the instrument was finalized. Due to the nature of the questions and the possible perceived threat of addressing issues of a sexual nature, the instrument was self-administered with no identifiers, providing anonymity to the respondents.
A nonprobability sampling frame was employed for the study. Data were gathered between June 2001 and February 2002 from 1252 students in various classes across the university faculties, representing 11% of the total student population for the enrollment period. It is important to note that although the study employed nonrandom sampling, statistical testing indicated no significant differences between the study sample and the university population for both age and sex distributions.[31] Because sexual transmission of HIV is the predominant mode of transmission in Jamaica (less than 2% of reported cases among adults are attributed to injecting drug use),[3] sexually inexperienced persons would not be considered at risk of HIV transmission nor an important group to target for HIV testing. Therefore, only data for 961 students (77%) who reported being sexually experienced were included in the present study.
Variables
A number of variables were used in these analyses. Some variables were recoded to facilitate the logistic regression analyses. The following operationalizations were used:
HIV testing: Students were asked if they had ever had an HIV test with responses being categorized as yes (1) and no (0).
Consistent condom use: Frequency of condom use was measured separately with both steady and nonsteady sex partners. A steady sex partner was defined as “someone with whom you have sexual intercourse on a regular or consistent basis, like a husband/wife or boy/girlfriend.” A nonsteady sex partner was defined as “someone with whom you have sexual intercourse but only occasionally or even just once.” For both partner types, students who reported always using condoms during the 3 months prior to the survey were coded as consistent condom users (1). Remaining students who reported using condoms usually, about half the time, seldom, or never were coded as inconsistent condom users (0). Those reporting no sexual partner during the 3 months prior to the survey were excluded from the regression analyses.
Multiple sex partners: Students reporting 2 or more sex partners in the 12 months prior to the survey were coded as having multiple sex partners (1), while those with 1 partner were coded as not having multiple sex partners (0). Due to issues of reliability associated with long recall periods, those reporting no sex partner during this time period were not surveyed about sexual behaviors.
Perceived risk of HIV: Students were asked to report their perceived risk of becoming infected with HIV. Response categories included great risk, some risk, not much risk, and no risk. Responses were dichotomized into categories of great/some risk (1) and little/no risk (0).
HIV education: Students were asked if they had attended a lecture, course, or community forum about HIV/AIDS in the 12 months before the survey. Those who reported attending such an activity were coded as receiving HIV/AIDS education (1), while remaining students were coded as not receiving such education (0).
HIV awareness: Students were asked if they knew someone who was infected with HIV or had died from AIDS. Those responding yes were coded as having a personal awareness of HIV (1), while those reporting knowing no such person were coded as having no personal awareness of HIV (0).
Marital status: Students were asked to report their current relationship status with categories including legally married, common-law, visiting partner (steady sex partner), boy/girlfriend, or no relationship. Students who reported being legally married or involved in a common-law relationship were coded as being married (1), while remaining students were coded as not being married (0).
Age: Students were asked to report their age, in years, on their last birthday. Those reporting being under the age of 25 were coded as youth (1) while those 25 years of age and older were coded as adults (0). This categorization was based on the World Health Organization's (WHO) definition of youth.[32]
Sex: Students were asked to report if they were male (1) or female (0).
Data analysis
Both bivariate (chi-square) and multivariate (hierarchical logistic regression) analyses were employed. Chi-square analyses were used to examine the differences between persons who reported previous HIV testing and those with no previous HIV testing. In addition, in order to understand the relationship among all the model variables with respect to the dependent variables of interest, hierarchical logistic regression modeling was used. This type of regression analysis takes an iterative form; an initial simple model is followed by more complex models in which the dependent variable from the immediately preceding model becomes a predictor along with the previous predictors.[33] All model variables have been dichotomized to facilitate the logistic regression analyses with the comparison group for each variable coded as (1) as described in the above section. The Figure illustrates the explanatory model.
Results
Sample Characteristics
The sample was predominantly female (67.8%) with a mean age of 28.2 years (Sx = 9.05). Almost one third were married or involved in a common-law relationship (31.9%) with slightly less than one quarter reporting being in no relationship at the time of the survey (23.1%). The majority of students (77.0%) had not attended any type of HIV education forum or lecture in the previous 12 months. However, approximately half (51.0%) did report knowing someone who was infected with HIV or had died from AIDS.
With respect to behaviors, less than half of students (41.8%) reported having been previously tested for HIV. Consistent condom use was low, with only one quarter (25.8%) of those engaging in sex with a steady partner in the previous 3 months reporting always using condoms. Among those who engaged in sex with a nonsteady partner during the same time, a slight majority (58.4%) reported always using condoms. Among those reporting at least 1 sex partner in the 12 months prior to the survey, less than one third (30.3%) reported having 2 or more partners during this time.
Bivariate Models
Table 1 presents the results of the bivariate analysis of HIV testing and selected variables. A number of statistically significant relationships emerged. Overall, persons who reported previous HIV testing, compared with those with no history of testing, were more likely to be older, married or in a common-law relationship, and female. They were also more likely to have attended an HIV education forum or lecture and know someone who is or has been infected with HIV, and were less likely to report condom use with steady partners.
Table 1.
Bivariate Results for Selected Sociodemographic, Attitudinal, and Behavioral Variables by HIV Testing (N = 961)
| Variable | Tested Number (%)* | Untested Number (%)* | Chi-Square X2 (P value) |
|---|---|---|---|
| Age | |||
| Less than 25 years | 102 (26.1) | 332 (61.1) | X2 = 111.29 |
| 25 years or older | 289 (73.9) | 211 (38.9) | (.0000) |
| Marital Status | |||
| Married/common-law | 174 (44.8) | 118 (22.2) | X2 = 53.20 |
| Not married/common-law | 214 (55.2) | 414 (77.8) | (.0000) |
| Sex | |||
| Male | 108 (27.2) | 197 (35.6) | X2 = 7.52 |
| Female | 289 (72.8) | 356 (64.4) | (.0061) |
| HIV Education in Previous 12 Months | |||
| Yes | 111 (28.5) | 104 (19.0) | X2 = 11.65 |
| No | 278 (71.5) | 443 (81.0) | (.0006) |
| HIV Personal Awareness | |||
| Yes | 235 (59.8) | 245 (44.5) | X2 = 21.33 |
| No | 158 (40.2) | 305 (55.5) | (.0000) |
| Perceived Risk of HIV | |||
| Great/some risk | 154 (42.9) | 231 (42.4) | X2 = 0.23 |
| Little/no risk | 205 (57.1) | 314 (57.6) | (.8790) |
| Condom Use With Most Recent Steady Sex Partner | |||
| Consistent | 60 (20.8) | 111 (29.8) | X2 = 6.86 |
| Inconsistent | 228 (79.2) | 261 (70.2) | (.0088) |
| Condom Use With Most Recent Nonsteady Sex Partner | |||
| Consistent | 47 (58.0) | 62 (57.9) | X2 = 0.00 |
| Inconsistent | 34 (42.0) | 45 (42.1) | (.9911) |
| Number of Sex Partners in Previous 12 Months | |||
| Multiple (2+) | 106 (28.7) | 158 (31.3) | X2 = 0.66 |
| Single (1) | 263 (71.3) | 347 (68.7) | (.4154) |
Valid percentages presented based on number of respondents providing for each measure.
Multivariate Models
Table 2 presents the results of the hierarchical logistic regression analyses and consists of 5 models. The model chi-square test assesses the extent to which the model independent variables, as a whole, are related to the log odds of the dependent variable for a given regression analysis. The model chi-square results indicated that 4 of the 5 submodels (submodels 1, 2, 3a, and 3c) in the hierarchical model were statistically significant, P < .001.
Table 2.
Hierarchical Logistic Regression Results*
| Model and Independent variables** | B | S.E. | Significance | Odds Ratio | 95% CI |
|---|---|---|---|---|---|
| Submodel 1: Perceived HIV Risk | |||||
| Age | .2359 | .1747 | .1767 | 1.27 | 0.90, 1.78 |
| Marital status | −.4864 | .1907 | .0108 | 0.61 | 0.42, 0.89 |
| Sex | .0649 | .1533 | .6719 | 1.07 | 0.79, 1.44 |
| HIV education | −.1975 | .1754 | .2601 | 0.82 | 0.58, 1.16 |
| HIV awareness | .3763 | .1498 | .0120 | 1.46 | 1.09, 1.95 |
| Submodel 2: HIV Testing | |||||
| Age | −1.1357 | .1865 | .0000 | 0.32 | 0.22, 0.46 |
| Marital Status | .4104 | .1902 | .0310 | 1.51 | 1.04, 2.19 |
| Sex | −.1274 | .1673 | .4463 | 0.88 | 0.63, 1.22 |
| HIV education | .4252 | .1827 | .0199 | 1.53 | 1.07, 2.19 |
| HIV awareness | .3310 | .1589 | .0372 | 1.39 | 1.02, 1.90 |
| Perceived HIV risk | .2224 | .1571 | .1569 | 1.25 | 0.92, 1.70 |
| Submodel 3a: Consistent Condom Use With Last Steady Partner | |||||
| Age | .1445 | .2461 | .5572 | 1.56 | 0.71, 1.87 |
| Marital status | −1.0798 | .2859 | .0002 | 0.34 | 0.19, 0.59 |
| Sex | .0936 | .2125 | .6596 | 1.10 | 0.72, 1.67 |
| HIV education | .1573 | .2525 | .5332 | 1.17 | 0.71, 1.92 |
| HIV awareness | .2409 | .2136 | .2595 | 1.27 | 0.84, 1.93 |
| Perceived HIV risk | −.6471 | .2104 | .0021 | 0.52 | 0.35, 0.79 |
| HIV testing | −.0660 | .2214 | .7657 | 0.94 | 0.62, 1.44 |
| Submodel 3b: Consistent Condom Use With Last Nonsteady Partner | |||||
| Age | .1180 | .4039 | .7701 | 1.13 | 0.51, 2.48 |
| Marital status | −1.2633 | .5584 | .0237 | 0.28 | 0.09, 0.84 |
| Sex | .5292 | .3365 | .1159 | 1.70 | 0.88, 3.28 |
| HIV education | .1713 | .4439 | .6996 | 1.19 | 0.50, 2.83 |
| HIV awareness | .1095 | .3490 | .7538 | 1.12 | 0.56, 2.21 |
| Perceived HIV risk | −.3827 | .3351 | .2535 | 0.68 | 0.35, 1.32 |
| HIV testing | .3626 | .3744 | .3328 | 1.44 | 0.69, 2.99 |
| Submodel 3c: Multiple Sex Partners | |||||
| Age | .4439 | .2141 | .0381 | 1.56 | 1.02, 2.37 |
| Marital status | −1.1461 | .2645 | .0000 | 0.32 | 0.19, 0.53 |
| Sex | 1.2606 | .1785 | .0000 | 3.53 | 2.49, 5.01 |
| HIV education | −.3969 | .2225 | .0744 | 0.67 | 0.43, 1.04 |
| HIV awareness | .2753 | .1844 | .1355 | 1.32 | 0.92, 1.90 |
| Perceived HIV risk | .5718 | .1750 | .0011 | 1.77 | 1.26, 2.50 |
| HIV testing | .3148 | .1952 | .1068 | 1.37 | 0.93, 2.01 |
For submodel 1, in which perceived risk of HIV is the dependent variable, 2 of the 5 independent variables emerged as significant. Persons who were married or had a common-law partner were less likely to perceive some level of HIV risk (odds ratio [OR] = 0.61; 95% confidence interval [CI] = 0.42–0.89) than were unmarried persons. Also, persons who reported knowing someone who was HIV-positive or had died from AIDS were more likely to report some level of HIV risk (OR = 1.46; 95% CI = 1.09–1.95) than were those who knew no such person.
For submodel 2, in which HIV testing is the dependent variable, 4 of the 6 independent variables were significant. Youth, compared with adults, were much less likely to report ever having been tested for HIV (OR = 0.32; 95% CI = 0.22–0.46), while married persons, compared with those not married, were more likely to report previous HIV testing (OR = 1.51; 95% CI = 1.04–2.19). HIV education and awareness were both associated with HIV testing; persons who reported attending an HIV education forum and those who reported knowing someone infected with HIV were more likely to report a previous HIV test (OR = 1.53; 95% CI = 1.07–2.19; and OR = 1.39; 95% CI = 1.02–1.90, respectively) than were those with no previous HIV education or personal awareness.
For submodel 3a, in which consistent condom use with most recent steady sex partner is the dependent variable, only 2 of the 7 independent variables were significant. Persons who were married or in common-law relationships were much less likely to report consistent condom use (OR = 0.34; 95% CI = 0.19–0.59) than were persons in no such relationships. Also, persons who perceived themselves to be at some risk for HIV were less likely to report consistent condom use than were persons who perceived little or no HIV risk (OR = 0.52; 95% CI = 0.35–0.79).
For submodel 3b, in which consistent condom use with most recent nonsteady sex partner is the dependent variable, the overall model was not significant (P = .13). However, 1 independent variable was associated with consistent condom use. Persons who were married or in common-law relationships were much less likely to report consistent condom use with their most recent nonsteady sex partner (OR = 0.28; 95% CI = 0.09–0.84) than were persons in no such relationship.
For submodel 3c, in which having multiple sex partners in the previous 12 months was the dependent variable, 4 of the 7 independent variables were significant. Males were far more likely than females to report having multiple sex partners during this time (OR = 3.53; 95% CI = 2.49–5.01). Youth, when compared with adults, were more likely to report having multiple sex partners (OR = 1.56; 95% CI = 1.02–2.37). Persons married or in common-law relationships were less likely than those in no such relationship to report multiple partners (OR = 0.32; 95% CI = 0.19–0.53). Lastly, persons reporting being at some or great risk of HIV were more likely to report multiple partners than were those who perceived no such risk (OR = 1.77; 95% CI = 1.26–2.50).
Discussion
First, it is important to note that although the proportion of university students reporting HIV testing was higher than in the sexually experienced Jamaican population,[34] the reported levels of testing were still too low to serve as an effective HIV prevention tool. Unfortunately, the stigma, discrimination, and violence faced by Jamaicans living with HIV/AIDS contribute to the avoidance of HIV testing by most people in the country.[35,36] Concerns regarding violations of confidentiality and test privacy, which may be compounded by negative social conditions, can serve as major barriers to testing.[37] These issues must be addressed by prevention programs if progress is to be made in promoting universal testing in Jamaica. Recognizing this need, a number of organizations in Jamaica have recently been awarded grants to address this barrier in hopes of improving the social climate and, as such, increasing persons' willingness to seek HIV testing and counseling.[38]
In addition to fear, students in the present study reported not having an HIV test because they believed they were not at risk of contracting HIV nor infected with the virus. This finding is similar to other research with college students.[8,9,39] Unfortunately, among those who reported being at no risk, a number of them were engaging in high-risk sexual behaviors. In order for programs promoting HIV testing to be effective, persons must be able to accurately assess their HIV risk. Previous research indicates that encouraging individuals to be tested if they engage in at-risk activities will not be appropriate or effective for individuals who have no perception of risk.[40] The identification of the barriers to HIV testing can help guide the development of appropriate interventions to promote universal testing among persons who may have placed themselves at risk, knowingly or unknowingly, of contracting or transmitting HIV.
As noted earlier, hierarchical modeling was employed to examine the correlates of HIV testing. The statistical results of the hierarchical modeling provide insight into HIV testing among university students in Jamaica. In the first submodel, perception of HIV risk was the dependent variable. Married persons perceived less risk of HIV than did persons with no legal or common-law partner. This finding supports previous research that has found that persons in stable relationships, due to issues of perceived trust and commitment, perceive less HIV risk than those in unstable relationships.[41] Also, knowing someone who is HIV-infected or had died from AIDS was positively associated with perceived risk of HIV. It is possible that as persons become more aware of HIV/AIDS, they are more likely to internalize the disease as a personal danger and recognize the consequences of the disease as well as the importance of protective measures.[21,42] It is important for programs to develop strategies that enable persons to accurately assess their risk of contracting HIV. Including persons living with HIV/AIDS as part of the intervention may be beneficial in achieving this goal.
In the second submodel, HIV testing was the dependent variable, and perceived risk of HIV became an independent variable along with the sociodemographic variables. A number of variables were associated with HIV testing, including both age and marital status, a differential that has been documented in previous research.[43] Within the Jamaican context, this finding may be more reflective of the fact that older and married persons in the sample were more likely to be employed, and in Jamaica, many employers enforce mandatory HIV testing.[44] Therefore, persons who are less likely to perceive themselves at risk for contracting HIV, such as married persons, may be more likely to actually be tested for HIV. It will be critical for programs to specifically target those at-risk persons who are not employed or are not required to take an HIV test and encourage voluntary HIV testing.
What may be more interesting and informative for developing and implementing programs promoting voluntary HIV testing is the finding that persons who had attended an HIV education forum or lecture and those who reported knowing someone who was living or had lived with HIV/AIDS were more likely to have had an HIV test. These findings are not surprising; previous research has found that persons who have higher levels of HIV knowledge and awareness are more likely to seek HIV testing. Also, knowing someone with HIV/AIDS may result in more positive attitudes towards HIV testing.[45–49] Increased knowledge and more positive attitudes, as well as a personal awareness of the consequences of the disease, may help persons to see the benefits of HIV testing and decrease some of the perceived barriers. These findings suggest that bringing those living with HIV/AIDS into contact with untested persons may have positive outcomes, such as increased knowledge and awareness, improved attitudes, and willingness to seek HIV testing.
In the last 3 submodels, when examining the relationship between HIV testing and sexual behaviors, we found no significant relationship between testing and condom use or number of sex partners. Although the bivariate analyses indicated a significant difference between those with previous testing and those with no testing, with respect to consistent condom use with most recent steady sex partner, once the variable was entered into the multivariate model, the effect disappeared, indicating that HIV testing, alone, was not an important correlate of condom use. As noted earlier, a review of HIV testing research has found mixed results with respect to the adoption of behavior change after testing.[10,50] It is possible that the adoption of protective sexual behavior is more a function of a test result and not the test itself. When attempting to study behavioral effects of HIV testing, it will be important to gather data on testing results.
When persons in the present study who reported previous HIV testing were specifically asked what behavioral changes, if any, had they made after testing, the majority reported no behavior change. This may be reflective of an attitude that if an optimal test result was received then it is not necessary to change or adopt protective behavior. However, a significant proportion of tested persons reported engaging in behaviors associated with increased risk of HIV transmission, including inconsistent condom use and having multiple sex partners. The risks associated with unprotected sex and multiple partnerships must be elucidated to sexually active persons and the importance of protective sexual behavior, even if a negative test result is received. It is critical that persons understand that a negative test result does not equate to an absence of HIV risk.
Although the present study has provided insight into some of the factors associated with HIV testing among university students in Jamaica, it is important to note the limitations of the study that may affect the validity of the findings. First, the sample was a nonrandom sample, consisting of persons who volunteered to participate in the study. Although the study sample was not statistically different from the university population in terms of age and sex,[31] the generalizability of the results to the university population in Jamaica may, nonetheless, be limited. Also, the use of self-reported data may have contributed to threats of internal validity. The interview instrument had a number of sex-related items. As with all surveys of sensitive issues, such data are likely to contain some bias. Intentional misreporting, incomplete recall, and misunderstanding of survey questions can reduce both the reliability and internal validity of the data.[51] Lastly, data on HIV serostatus would have been important for explaining the relationship between HIV testing and sexual risk behaviors. However, considering the social climate in Jamaica with respect to persons living with HIV/AIDS, we felt that students would not be likely to provide valid information regarding HIV test results,[40] and as such, we did not include this measure in the survey instrument.
Conclusion
Irrespective of the study finding that previous HIV testing was not significantly associated with risky sexual behaviors, this should not negate the importance of receiving an HIV test. One of the first steps in self-protection from HIV is to be informed of one's HIV status and make appropriate and responsible sexual decisions. Although previous research has found mixed results with respect to HIV testing and subsequent behaviors, most studies have found HIV testing and knowledge of serostatus to be important, to some degree, in the adoption of safer sex behaviors. Effective messages and prevention programs need to be developed and implemented to promote universal HIV testing and counseling, especially among younger, sexually experienced students, so that these persons may make informed sexual decisions with respect to protective sexual behaviors, including having discussions about safer sex, inquiring about a potential partner's HIV status, and the adoption of condom use with all sex partners, especially where HIV status is unknown. Considering the actual and estimated number of HIV/AIDS cases in Jamaica, it is clear that effective strategies are urgently needed to prevent both primary and secondary HIV transmission. Programs that can increase persons' knowledge of HIV, including risks associated with various behaviors, as well as personal awareness, may be more efficacious than current efforts in increasing HIV testing among sexually experienced persons in Jamaica.
Figure 1.
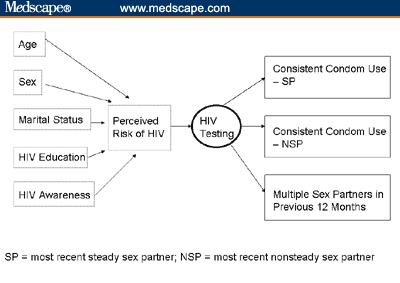
Explanatory model.
Contributor Information
Lisa R. Norman, Social and Behavioral Sciences, Brewton-Parker College, Mount Vernon, Georgia ladyle64@yahoo.com.
Yitades Gebre, National HIV/STI Control and Prevention Program, Ministry of Health, Kingston, Jamaica.
References
- 1.Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2003. UNAIDS. AIDS Epidemic Update – December 2003. [Google Scholar]
- 2.Camara B, Branson B. Trinidad: Caribbean Epidemiology Center; 2002. Jun, CAREC-CDC Estimates of Persons Living with HIV/AIDS in the CAREC Countries at the End of 2002. [Google Scholar]
- 3.Gebre Y. Kingston, Jamaica: Epidemiology Unit, Ministry of Health; National HIV/STD Prevention and Control Programme Facts and Figures, Jamaica AIDS Report, 2004, June 2004. [Google Scholar]
- 4.2001. pp. 1–58. CDC. Revised guidelines for HIV counseling, testing, and referral. MMWR Morb Mortal Wkly Rep.
- 5.Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; UNAIDS. UNAIDS/WHO Policy Statement on HIV Testing. June 2004. [Google Scholar]
- 6.Becker MH. Thorafore, NJ: Charles B. Slack, Inc.; 1974. The Health Belief Model and Personal Health Behavior. [Google Scholar]
- 7.Kok G. Targeted prevention for people with HIV/AIDS: feasible and desirable? Patient Educ Couns. 1999;36:239–246. doi: 10.1016/s0738-3991(98)00141-4. [DOI] [PubMed] [Google Scholar]
- 8.Gielen AC, Faden RR, O'Campo P, Kass N, Anderson J. Women's protective sexual behaviors: a test of the health belief model. AIDS Educ Prev. 1994;6:1–11. [PubMed] [Google Scholar]
- 9.Higgins DL, Galavotti C, O'Reilly K. Evidence for the effects of HIV antibody counseling and testing on risk behaviors. JAMA. 1991;266:2419–2429. [PubMed] [Google Scholar]
- 10.Wolitizki RJ, MacGowan RJ, Higgins DL, Jorgensen CM. The effects of HIV counseling and testing on risk-related practices and help-seeking behavior. AIDS Educ Prev. 1997;9(3 suppl B):52–67. [PubMed] [Google Scholar]
- 11.Mattson M. Impact of HIV test counseling on college students' sexual beliefs and behaviors. Am J Health Behav. 2002;26:121–136. doi: 10.5993/ajhb.26.2.5. [DOI] [PubMed] [Google Scholar]
- 12.Anastasi MC, Sawyer RG, Pinciaro PJ. A descriptive analysis of students seeking HIV antibody testing at a university health service. J Am Coll Health. 1999;48:13–19. doi: 10.1080/07448489909595667. [DOI] [PubMed] [Google Scholar]
- 13.Siegel DM, Klein DI, Roghmann KJ. Sexual behavior, contraception, and risk among college students. J Adolesc Health. 1999;25:336–343. doi: 10.1016/s1054-139x(99)00054-3. [DOI] [PubMed] [Google Scholar]
- 14.Dorr N, Krueckeberg S, Strathman A, Wood MD. Psychosocial correlates of voluntary HIV antibody testing in college students. AIDS Educ Prev. 1999;11:14–27. [PubMed] [Google Scholar]
- 15.Velez CN, Rodriguez LA, Schoenbaum E, Ungemack JA. Puerto Rican youth in drug treatment facilities: who volunteers for HIV testing? P R Health Sci J. 1997;16:37–44. [PubMed] [Google Scholar]
- 16.Robles RR, Matos TD, Colon HM, Marrero CA, Reyes JC. Effects of HIV testing and counseling on reducing HIV risk behavior among two ethnic groups. Drugs Soc. 1996;9:173–184. doi: 10.1300/J023v09n01_10. [DOI] [PubMed] [Google Scholar]
- 17.Voluntary HIV-1 Counseling and Testing Efficacy Study Group. Efficacy of voluntary HIV-1 counselling and testing in individuals and couples in Kenya, Tanzania, and Trinidad: a randomized trial. Lancet. 2000;356:103–212. [PubMed] [Google Scholar]
- 18.Cunningham I. An innovative HIV/AIDS research and education program in Puerto Rico. SIECUS Report. 1998;26:18–20. [PubMed] [Google Scholar]
- 19.Norman LR, Carr R. The role of HIV knowledge on HIV-related behaviors: a hierarchical analysis of adults in Trinidad. Health Educ. 2003;103:145–155. [Google Scholar]
- 20.Norman LR. Predictors of consistent condom use: a hierarchical analysis of adults from Kenya, Tanzania and Trinidad. Int J STD AIDS. 2003;14:584–590. doi: 10.1258/095646203322301022. [DOI] [PubMed] [Google Scholar]
- 21.Worthington C, Myers T. Factors underlying anxiety in HIV testing: risk perceptions, stigma, and the patient-provider power dynamic. Qual Health Res. 2003;13:636–655. doi: 10.1177/1049732303013005004. [DOI] [PubMed] [Google Scholar]
- 22.de Paoli MM, Manongi R, Klepp KI. Factors influencing acceptability of voluntary counseling and HIV-testing among pregnant women in Northern Tanzania. AIDS Care. 2004;16:411–425. doi: 10.1080/09540120410001683358. [DOI] [PubMed] [Google Scholar]
- 23.Zak-Place J, Stern M. Health belief factors and dispositional optimism as predictors of STD and HIV preventive behavior. J Am Coll Health. 2004;52:229–236. doi: 10.3200/JACH.52.5.229-236. [DOI] [PubMed] [Google Scholar]
- 24.Maguen S, Armistead LP, Kalichman S. Predictors of HIV antibody testing among gay, lesbian, and bisexual youth. J Adolesc Health. 2000;26:252–257. doi: 10.1016/s1054-139x(99)00078-6. [DOI] [PubMed] [Google Scholar]
- 25.Ajzen I, Fishbein M. Englewood Cliffs, NJ: Prentice Hall, Inc.; 1980. Understanding Attitudes and Predicting Social Behavior. [Google Scholar]
- 26.Bandura A. Englewood Cliffs, NJ: Prentice Hall, Inc.; 1986. Social Foundations of Thought and Action: A Social Cognitive Theory. [Google Scholar]
- 27.Dilorio C, Soet J. Atlanta, Ga: Emory University; 1996. Sex in the Nineties: The Atlanta Multi-University Prevention Survey. [Google Scholar]
- 28.Prince A, Bernard A. Edwardsville, Ill: Southern Illinois University; 1995. Southern Illinois University HIV/AIDS Study. [Google Scholar]
- 29.CDC. Atlanta, Ga: CDC Behavioral Intervention Research Branch; 1992. Hemophilia Behavioral Intervention Evaluation Project. [Google Scholar]
- 30.Ministry of Health. National Knowledge, Attitudes and Practices Survey. Kingston, Jamaica: Epidemiology Unit; 2000. [Google Scholar]
- 31.University of the West Indies. The Registry – 2001/2002. Kingston, Jamaica: Campus Records Office, University Archives and Records Management Programme; 2002. [Google Scholar]
- 32.WHO. Definitions of indicators and targets for STI, HIV and AIDS surveillance. HIV/AIDS Surveill Rep. 2000;16:9–11. [Google Scholar]
- 33.Cohen J, Cohen P. Hillsdale, NJ: Lawrence Erlbaum; 1983. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. [Google Scholar]
- 34.Jamaica Ministry of Health. National Knowledge, Attitudes and Practices Survey. Kingston, Jamaica: Epidemiology Unit, Ministry of Health; 2000. [Google Scholar]
- 35.UNAIDS. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2003. Illustrative Menu of Partnership Options in Jamaica. [Google Scholar]
- 36.Carr R. Stigma, coping and gender: a study of HIV Jamaicans. Race Gender Class. 2002;9:122–144. [Google Scholar]
- 37.Worthington C, Myers T. Desired elements of HIV testing services: test recipient perspectives. AIDS Patient Care. 2002;16:537–548. doi: 10.1089/108729102761041092. [DOI] [PubMed] [Google Scholar]
- 38. US Embassy. Ambassador's Fund for HIV/AIDS Helps Communities Fight Stigma. Kingston, Jamaica. Media Release. July 2003.
- 39.Bernard A, Prince A. HIV testing practices and attitudes of college students. Am J Health Stud. 1998;14:84–94. [Google Scholar]
- 40.Jackson LA, Millson P, Calzavara L, et al. HIV-positive women living in the metropolitan Toronto area: their experiences and perceptions related to HIV testing. The HIV Women's Study Group. Can J Public Health. 1997;88:18–22. doi: 10.1007/BF03403852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Misovich S, Fisher J, Fisher W. Close relationships and elevated HIV risk behavior: evidence and possible underlying psychological processes. Gen Psychology Rev. 1997;1:72–107. [Google Scholar]
- 42.Tierney KJ. Toward a critical sociology of risk. Sociol Forum. 1999;14:215–242. [Google Scholar]
- 43.Kellerman SE, Lehman JS, Lansky AM, et al. HIV testing within at-risk populations in the United States and the reasons for seeking or avoiding HIV testing. J AIDS. 2002;31:202–210. doi: 10.1097/00126334-200210010-00011. [DOI] [PubMed] [Google Scholar]
- 44.National AIDS Committee. Kingston, Jamaica: 2001. Dec, HIV/AIDS Legal, Ethical and Human Rights Issues. [Google Scholar]
- 45.Stein JA, Nyamathi A. Gender differences in behavioral and psychosocial predictors of HIV testing and return for test results in a high-risk population. AIDS Care. 2000;12:343–356. doi: 10.1080/09540120050043007. [DOI] [PubMed] [Google Scholar]
- 46.Samet JH, Winter MR, Grant L, Hingson R. Factors associated with HVI testing among sexually active adolescents: a Massachusetts survey. Pediatrics. 1997;100((3 Pt 1)):371–377. doi: 10.1542/peds.100.3.371. [DOI] [PubMed] [Google Scholar]
- 47.Gerbert B, Sumser J, Maguire BT. The impact of who you know and where you live on opinions about AIDS and health care. Soc Sci Med. 1991;32:677–681. doi: 10.1016/0277-9536(91)90146-4. [DOI] [PubMed] [Google Scholar]
- 48.Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counseling and testing in a black township in Cape Town, South Africa. Sex Transm Infect. 2003;79:442–447. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Patient DR, Orr NM. Stigma: beliefs determine behavior. Disabil World. 2003;20:1–20. Available at: http://www.disabilityworld.org/09-10_03/news/stigma.shtml Accessed February 14, 2005. [Google Scholar]
- 50.Wenger NS, Greenberg JM, Hilborne LH, Kusseling F, Mangotich M, Shapiro MF. Effects of HIV antibody testing and AIDS education on communication about HIV risk and sexual behavior: a randomized controlled trial of college students. Ann Intern Med. 1992;117:905–911. doi: 10.7326/0003-4819-117-11-905. [DOI] [PubMed] [Google Scholar]
- 51.Catania J, Gibson D, Chitwood D, Coates T. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior. Psychol Bull. 1990;108:339–362. doi: 10.1037/0033-2909.108.3.339. [DOI] [PubMed] [Google Scholar]


