Abstract
Objective
To determine whether the probability of undergoing coronary bypass surgery within a certain time was related to the number of patients on the wait list at registration for the operation in a publicly funded health system.
Methods
A prospective cohort study comparing waiting times among patients registered on wait lists at the hospitals delivering adult cardiac surgery. For each calendar week, the list size, the number of new registrations, and the number of direct admissions immediately after angiography characterized the demand for surgery.
Results
The length of delay in undergoing treatment was associated with list size at registration, with shorter times for shorter lists (log-rank test 1,198.3, p<.0001). When the list size at registration required clearance time over 1 week patients had 42 percent lower odds of undergoing surgery compared with lists with clearance time less than 1 week (odds ratio [OR] 0.58 percent, 95 percent, confidence interval [CI] 0.53–0.63), after adjustment for age, sex, comorbidity, period, and hospital. The weekly number of new registrations exceeding weekly service capacity had an independent effect toward longer service delays when the list size at registration required clearance time less than 1 week (OR 0.56 percent, 95 percent CI 0.45–0.71), but not for longer lists. Every time the operation was performed for a patient requiring surgery without registration on wait lists, the odds of surgery for listed patients were reduced by 6 percent (OR 0.94, CI 0.93–0.95).
Conclusion
For wait-listed patients, time to surgery depends on the list size at registration, the number of new registrations, as well as on the weekly number of patients who move immediately from angiography to coronary bypass surgery without being registered on a wait list. Hospital managers may use these findings to improve resource planning and to reduce uncertainty when providing advice on expected treatment delays.
Keywords: Access to health care, surgical procedures, elective surgery, waiting lists, delay in treatment, patient admission, registries, cohort studies
In the Canadian province of British Columbia (BC), priority wait lists (Noseworthy, McGurran, and Hadorn 2003) are commonly used to manage access to elective procedures according to urgency of treatment. In particular, patients with coronary artery disease (CAD) are prioritized according to angina symptoms, coronary anatomy, and left ventricular function impairment to facilitate access to surgical revascularization within a clinically appropriate time (Levy et al. 2005).
When wait lists are used to ration access to medical services, the length of time that patients may be required to wait is usually uncertain (Sobolev, Brown, and Zelt 2000). This is a natural product of random variations in demand, in service time, and in the percentage of urgent cases. Previous studies described time to surgery according to procedure, urgency, socioeconomic status, emergency referrals, management practice, surgical cancellations, and period (Clover et al. 1998; DeCoster et al. 1999; Sykora et al. 1999; Pell et al. 2000; Mayo et al. 2001; Sobolev et al. 2001; Sobolev, Brown, and Zelt 2001; Noseworthy, McGurran, and Hadorn 2003).
Describing waiting times for coronary artery bypass graft (CABG) in BC, Katz, Mizgala, and Welch (1991) suggested that variation in the size of wait list among individual surgeons may be an important factor as well. Indeed, if there are patients on the list, then for a patient who just arrived to be admitted within a certain time, all patients ahead must have been served. Surprisingly, little is known on how the list size at registration affects waiting time for elective surgical procedures. Without this, it is difficult to obtain accurate estimates of how much service capacity is required to maintain short wait lists for surgery (Thomas et al. 2001).
In this paper we determine whether the probability of undergoing surgery within a certain time is related to the number of patients on the wait list at registration. To examine the relationship between the size of a surgical wait list and the length of delay before undergoing treatment, we study actual waiting times from a population-based database of patients registered for CABG surgery between 1991 and 2000 in BC.
First, we compare the number of weeks required for specified proportions of patients to undergo the operation by list-size categories. Then, we estimate the effect of list size on waiting time using discrete-time survival models. The next sections describe the patient journey for care, data sources, study variables, and our findings on the impact of the list size.
The Clinical Research Ethics Board of the University of British Columbia approved the study protocol.
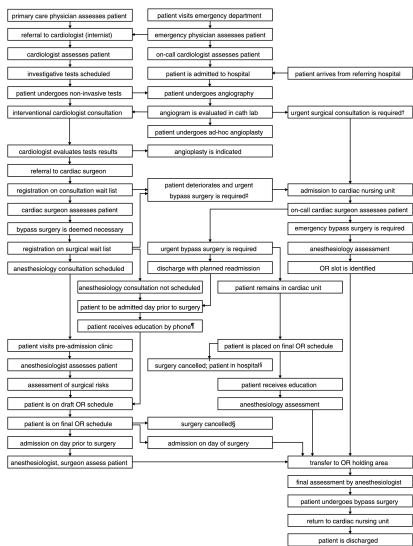
PATHWAY TO SURGICAL REVASCULARIZATION
Patients presenting with symptoms of CAD are referred to the cardiologist to assess the need for revascularization. If symptoms indicate the onset of an acute coronary syndrome, patients are advised to seek urgent medical help.
The cardiologist evaluates the results of coronary angiography and decides on treatment (Grech 2003). If coronary angioplasty is not indicated, patients are referred to a cardiac surgeon, who assesses their need and suitability for CABG. Cardiologists refer patients to several surgeons.
When urgent assessment is deemed necessary, patients are admitted to a hospital cardiac ward directly from the catheterization laboratory. If deemed suitable for surgery, such patients remain in the hospital until the operation.
Alternatively, patients are scheduled for an outpatient consultation with the cardiac surgeon at a later date. Following the consultation in which surgery is deemed necessary, surgeons register on their wait lists patients who require CABG and decide to undergo the operation in one of four hospitals where surgeons have admitting rights. A priority category is assigned to each patient by urgency of treatment.
In each hospital, patient access to surgery is managed through scheduling operating room time. Patients are selected for scheduling both from hospital cardiac wards and from the surgical wait lists based on allocated operating room timeslots and priority.
Patients with a higher priority are selected for surgery ahead of those with a lower priority, regardless of the date of registration. Patients in the same priority category are selected in the order of their registration. The availability of other hospital resources is another factor considered when selecting patients for scheduling the operation (Hamilton and Breslawski 1994).
Before being added to the operating room schedule, each patient is assessed by an anesthesiologist as to suitability for surgery. The operation is postponed if the patient is deemed unfit, or when the anesthesiologist requests additional preoperative investigation. Emergency patients have preferential access to hospital resources, which may cancel scheduled operations. On the other hand, already scheduled patients may undergo surgery ahead of their scheduled dates if an operating room timeslot becomes available.
Patients are removed from the wait lists after undergoing the operation or if they die, reconsider the decision to undergo surgery, accept surgery from another surgeon, move out of the province, or if their conditions deteriorate to the point that the operation is no longer possible.
A diagram showing the patient path after presenting with symptoms of CAD until CABG can be found in Figure 1.
Figure 1.
The Flow of Patients from Presenting with Symptoms to Coronary Bypass Surgery
Regional Cardiac Care Coordinators †facilitate physician-to-physician communication to expedite surgical assessment, ‡monitor patients at home until their procedures, §oversee scheduling of patients whose surgeries were cancelled, and ¶help to provide educational materials to patients and their families. The diagram was produced with the support from SIMCARE.
OR, operating room.
DATA
Data Sources
The BC Cardiac Registries (BCCR) prospectively capture the time of registration for surgery, the time of surgery, or removal from wait lists without surgery, for all patients accepted for surgery in the four tertiary hospitals delivering adult cardiac care to four million residents of BC (Levy et al. 2005). Each hospital has a catheterization laboratory. Offices of all cardiac surgeons provide information weekly to the BCCR on registrations for surgery, operations performed, wait-list reconciliation (removals), and discharge summaries.
Patients
There were 9,366 records of registration for isolated CABG added to BCCR between January 1991 and December 2000. We excluded 135 records of patients who were emergency cases (30), were removed on the registration date (101), or who had missing operating room reports (4). The remaining 9,231 records had either the surgery date or the date and reason of removal from the list without surgery.
The study period ended in December 2001 because of data availability, allowing only 52 weeks of follow-up after the last patients were added to the list. Therefore, we restricted the analysis to the first 52 weeks after registration so that observations of 475 (5 percent) patients remaining on the lists that long were censored. Of those, 167 eventually underwent surgery, 7 died, 78 received medical treatment, 104 declined surgery, 17 were transferred to another surgeon or hospital, and 102 were removed for other reasons.
As patients who moved from angiography to surgery on an expedited basis were not added to the wait lists, they were not included in analyses of wait-list times. These patients contributed to demand figures only.
Priority Categories
All cardiac surgeons in BC use a common guideline for prioritizing patients and assigning a target time for surgery based on angina symptoms, affected coronary anatomy, and left ventricular function impairment described in our previous report (Levy et al. 2005). The suggested time to surgery is 3 days for patients with left main coronary artery stenosis greater than 70 percent (Priority 1), 6 weeks for patients with persistent unstable angina, impaired left ventricular function, and significant obstruction defined as left-main stenosis, triple-vessel disease or double-vessel disease with significant proximal left anterior descending stenosis (Priority 2), and 12 weeks for patients with intractable chronic angina, normal left ventricular function, and single-vessel disease or double-vessel disease with no lesion in the proximal left anterior descending artery (Priority 3).
Demand for Surgery
For each calendar week during the study period, the demand for surgery was characterized by (1) the existing list size, (2) the batch size of new arrivals, and (3) the number of direct admissions immediately after angiography.
For each patient, the list size was a census of patients with higher or equal priority present at registration on the list in a hospital. Patients contributed one count to the list size for each week they remained on the list, except for the week of arrival. As operations are scheduled a week in advance, patients who underwent surgery are considered removed from the wait list in the week previous to their admission dates. Patients, who remained on wait lists at 52 weeks, contribute to the list size for 52 weeks following registration. For each patient, the batch size was a count of patients with higher or equal priority registered on the list in the same week. The number of direct admissions was a count of surgeries performed without wait-list registration during the week of arrival.
Comorbidity
Data on coexisting medical conditions were retrieved from the BC Linked Health Database Hospital Separations File using diagnoses reported in discharge abstracts within 1 year prior to registration for CABG.1 Each patient was classified as (1) presenting with no coexisting conditions, (2) presenting with congestive heart failure, diabetes, chronic obstructive pulmonary disease, cancer, or rheumatoid arthritis, or (3) presenting with other coexisting chronic conditions including peripheral vascular disease, cerebrovascular disease, dementia, peptic ulcer disease, hemiplegia, renal disease, or liver disease (Romano, Roos, and Jollis 1993).
STATISTICAL ANALYSIS
Waiting Time
Surgical wait lists are used to hold patient names until the operating room time can be scheduled. As scheduling is done weekly, waiting time is computed as the number of calendar weeks between registration and surgery or removal for other reasons. The date at which a surgeon's office submits the operating room booking request for surgery serves as the date of registration on the list.
Cumulative and Conditional Probability of Surgery
Waiting times were analyzed as prospective observations that have been followed up from registration, wait-list week 0, to removal, last week on the list. We interpreted time to removal without surgery as a censored observation, assuming that the actual wait would be larger otherwise. The cumulative probability of undergoing surgery within a certain time was estimated using the product-limit method (Bland and Altman 1998). By using the log-rank test, access to surgery was compared among patient groups (Bland and Altman 2004).
Study Variables
The list size was categorized in relation to clearance time, that is, a hypothetical time within which the list will be cleared at a maximum weekly service capacity if there are no new arrivals. We divided the list size into four categories: (1) lists requiring less than a week of clearance time, (2) half a month, (3) a month, (4) over 1 month. In three hospitals with the service capacity of 15 operations a week, the following numbers of patients on the list—0–14, 15–29, 30–59, and over 60—correspond to clearance time of a week, half a month, a month, over 1 month. In a hospital with the service capacity of 25 operations weeks, the same clearance times correspond to 0–24, 25–49, 50–99, and over 100 patients on the list.
Batch size of arrivals was categorized as whether or not it exceeded the weekly number of operating room slots allocated to patients on the wait lists. Therefore, we divide the batch size into two batch-size categories: (1) the arrival of one to six patients at the three hospitals, or one to 12 patients at the other hospital; and (2) the arrival of seven and more patients at the three hospitals, or 13 and more patients at the other hospital.
The weekly number of direct admissions was treated as a continuous variable.
Regression Models
The effect sizes of study variables were estimated by the odds ratio (ORs) using discrete-time survival regression models (Allison 1982). For the direct admissions, we interpret the OR as a change in the weekly odds of elective surgery associated with one additional surgery performed immediately after angiography.
In multivariate analysis we adjusted for age, sex, comorbidity, period, and hospital. Although hospital-related factors were used to create variables describing the demand for surgery, we entered an indicator variable for each hospital in the models in order to obtain regression estimates for the study variables adjusted for possible variations in access management. Hospital 1 was coded as referent.
RESULTS
Table 1 outlines the distribution of wait-listed patients by age, sex, period of registration, hospital, priority, comorbidity, list size at registration, and size of batch arrival. In the group of patients who underwent surgery without registration on wait lists, the distribution by age was similar to the listed patients, with the majority (69 percent) undergoing surgery between 60 and 79 years. Compared with the listed patients, the proportion of women (22 percent) was slightly higher, Table 1.
Table 1.
Characteristics of 9,231 Registrations for Coronary Artery Bypass Surgery and 10,467 Direct Admission Surgeries
| Characteristics | Wait-Listed Patients (%) | Direct Admission Surgeries (%) |
|---|---|---|
| Age group (years) | ||
| <50 | 732 (7.9) | 808 (7.7) |
| 50–59 | 2,005 (21.7) | 2,082 (19.9) |
| 60–69 | 3,530 (38.2) | 3,689 (35.2) |
| 70–79 | 2,770 (30.0) | 3,509 (33.5) |
| ≥80 | 194 (2.1) | 3,79 (3.6) |
| Sex | ||
| Women | 1,634 (17.7) | 2,313 (22.1) |
| Men | 7,597 (82.3) | 8,154 (77.9) |
| Period of registration/surgery | ||
| 1991–1992 | 1,724 (18.7) | 1,770 (16.9) |
| 1993–1994 | 1,889 (20.5) | 1,526 (14.6) |
| 1995–1996 | 2,010 (21.8) | 1,686 (16.1) |
| 1997–1998 | 1,888 (20.5) | 1,997 (19.1) |
| 1999–2000 | 1,720 (18.6) | 2,454 (23.4) |
| 2001 | 1,034 (9.9) | |
| Hospital at registration/surgery | ||
| 1 | 1,902 (20.6) | 1,590 (15.2) |
| 2 | 3,137 (34.0) | 2,522 (24.1) |
| 3 | 2,123 (23.0) | 4,362 (41.7) |
| 4 | 2,069 (22.4) | 1,993 (19.0) |
| Urgency at registration/surgery | ||
| Priority 1 | 664 (7.2) | 5,353 (51.1) |
| Priority 2 | 6,553 (71.0) | 4,536 (43.3) |
| Priority 3 | 2,014 (21.8) | 523 (5.0) |
| Unknown | 55 (0.5) | |
| Comorbidity at registration/surgery | ||
| None | 4,775 (51.7) | 1,159 (11.1) |
| CHF, COPD, RA, diabetes, cancer | 2,012 (21.8) | 4,040 (38.6) |
| Other conditions | 2,444 (26.5) | 5,268 (50.3) |
| Wait-list size category | ||
| 1 | 1,514 (16.4) | |
| 2 | 1,275 (13.8) | |
| 3 | 3,955 (42.8) | |
| 4 | 2,487 (26.9) | |
| Batch size category | ||
| 1 | 6,640 (71.9) | |
| 2 | 2,591 (28.1) | |
CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; RA, rheumatoid arthritis.
Differences between these two groups in the distribution by priority categories and coexisting medical conditions indicate that sicker patients were more likely to undergo the operation without delay. For example, less than 10 percent of wait-listed patients were assigned to priority category 1 compared with over half of the patients who were admitted for surgery directly after angiography. Similarly, over half of the wait-listed patients had no identifiable comorbid conditions, compared with only 11 percent in the other group.
There was a variation between hospitals in the number of patients who stayed on the list longer than 52 weeks, from almost 0 in hospital 1 and 2 to 118 (3.8 percent) in hospital 4 to 332 (15.6 percent) in hospital 3. One-third of such patients in hospital 3 were registered in 1993–1994.
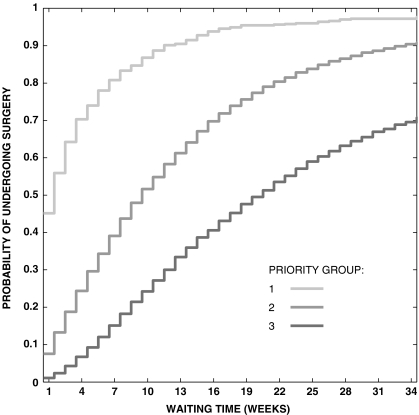
Access to Surgery by Priority
As expected, priority had a major influence on waiting times, with shorter times in higher priority groups (log-rank test 1,639.2, p<.0001). For instance, waiting times in priority-group 3 were such that 10 percent of the patients underwent surgery within 6 weeks, 25 percent within 11 weeks, 50 percent within 21 weeks, and 75 percent within 41 weeks, whereas half of priority-group 1 patients underwent surgery within 2 weeks, and 75 percent did so within 6 weeks (Figure 2). There was a corresponding gradient in average surgery rate across priority groups, from 20.2/100 patients/week in group 1 to 6.7 in group 2 to 3.2 in group 3.
Figure 2.
Estimated Probabilities of Undergoing Surgery by Priority Group
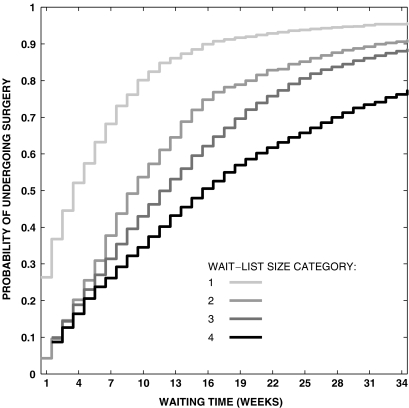
Access to Surgery by the List Size at Registration
There was a strong association between list size at registration and waiting time, with shorter waits experienced by patients registered on shorter lists (log-rank test 1,198.3, p<.0001). When the list at registration had clearance time exceeding 1 month (category 4), waiting times were such that 10 percent of the patients underwent surgery within 3 weeks, 25 percent within 7 weeks, 50 percent within 16 weeks, and 75 percent within 33 weeks, whereas 50 percent of patients registered on lists with clearance time less than 1 week (category 1) underwent surgery within 4 weeks, and 75 percent did so within 9 weeks (Figure 3).
Figure 3.
Estimated Probabilities of Undergoing Surgery by Wait-List Size Categories
Access to Surgery by List and Batch Size Combined
Batch size of arrivals in the week of registration was also a factor in the variation of waiting times when wait lists had clearance time less than 1 week, with shorter times when the batch size was smaller (log-rank test 6.6, p=.01). Waiting times for patients who, when registered, had less than 1-week clearance time worth of patients ahead of them (list-size category 1) and who arrived in a batch bigger than the weekly capacity (batch-size category 2) were such that 10 percent of the patients underwent surgery within 1 week, 25 percent within 3 weeks, 50 percent within 6 weeks, and 75 percent within 11 weeks. In contrast, 50 percent of patients with list-size category 1 who arrived in batches smaller than the weekly capacity (batch-size category 1) underwent surgery within 4 weeks, and 75 percent did so within 9 weeks. The difference in waiting times according to batch size was also significant in list-size category 2 (log-rank test 20.9, p<.0001), category 3 (log-rank test 88.1, p<.0001), and category 4 (log-rank test 119.1, p<.0001).
Regression Analysis
Table 2 shows the association between list size and the probability of surgery as measured by OR derived from three regression models after adjustment for age, sex, comorbidity, calendar period, and hospital.
Table 2.
Association between the Conditional Probability of Surgery and Wait-List Size as Measured by Odds Ratios* Derived from Discrete-Time Survival Regression Models
| OR (95% CI) | |||
|---|---|---|---|
| Surgery Demand | Model I† | Model II‡ | Model III‡ |
| List-size category 1 | 1.0 | — | — |
| List-size category 1, batch-size category 1 | — | 1.0 | 1.0 |
| List-size category 1, batch-size category 2 | — | 0.55 (0.44, 0.69) | 0.56 (0.45, 0.71) |
| List-size category 2 | 0.58 (0.53, 0.63) | 0.55 (0.50, 0.60) | 0.56 (0.51, 0.61) |
| List-size category 3 | 0.43 (0.40, 0.46) | 0.41 (0.38, 0.44) | 0.40 (0.37, 0.43) |
| List-size category 4 | 0.33 (0.31, 0.36) | 0.32 (0.29, 0.35) | 0.31 (0.28, 0.33) |
| Direct admissions | — | — | 0.94 (0.93, 0.95)§ |
Adjusted for age, sex, comorbidity, calendar period, hospital, and week on the list.
Reference is clearance time less than 1 week.
Reference is clearance time less than 1 week, batch size less than weekly capacity (list-size category 1, batch-size category 1).
Associated with one additional surgery performed without wait-list registration.
In Model I, variables for list-size categories were coded so that category 1 (clearance time less than 1 week) was the referent. The odds of surgery were 42 percent lower in list-size category 2, OR (95 percent confidence interval [CI])=0.58 (0.53, 0.63), 57 percent lower in category 3, OR=0.43 (0.40, 0.46), and 67 percent lower in category 4, OR=0.33 (0.31, 0.36), compared with category 1.
For Model II, 2, Table 2 shows an additional comparison group corresponding to list-size category 1 and batch-size category 2 combined, with the referent group consisting of list-size category 1 in combination with batch-size category 1. After adjustment for covariates, there was no difference between the ORs for these two groups as measured by the Wald test (χ2=0.01, p=.92).
Derived from Model II, the OR was 0.55 (0.44, 0.69) for combined list-size category 1 and batch-size category 2, suggesting that the odds of surgery were 45 percent lower compared with those in the referent group. The odds of surgery were 45 percent lower in list-size category 2, OR=0.55 (0.50, 0.60), 59 percent lower in category 3, OR=0.41 (0.38, 0.44), and 68 percent lower in category 4, OR=0.32 (0.29, 0.35), compared with the referent group.
Model III shows the effect of the number of weekly surgeries without registration on waiting times of listed patients. Every time an additional patient was operated without being registered on wait lists, for patients registered in that week, the odds of surgery were reduced by 6 percent, OR=0.94 (0.93–0.95). This effect was independent of the size of batch arrivals and list size at registration.
DISCUSSION
In this paper we examined the relationship between the length of time before treatment and the length of the wait list at registration for CABG surgery in a publicly funded health system.
Our results provide evidence that list size had an effect on the length of delay in undergoing treatment, with shorter times for shorter lists. Patients who were registered when the list size required clearance time exceeding 1 month had 69 percent lower odds of undergoing surgery at any week on the list than those registered on a list with clearance time less than 1 week, after adjustment for other factors.
The weekly number of new registrations exceeding weekly service capacity had an independent effect toward longer service delays when list size required clearance time of less than 1 week, but not for longer lists. We also found an independent effect of the number of surgeries delivered through direct admissions.
The quality of information on dates of registration and removal is a concern in this analysis. Although we used the date at which the surgeon's office sends operating room booking request as the date of registration on the list, no audit has been conducted to verify the accuracy of coding dates in BCCR records.3
Some evidence that procedure dates are recorded accurately comes from further investigation in which we found that for 8,159 BCCR records with surgery dates, 8,030 (98.4 percent) were found to have the operation date recorded between admission and discharge dates in the Hospital Separations File. An additional 76 records (0.9 percent) had their procedure dates either a few days before the admission date or after the discharge date. Fifty-three records (0.7 percent) could not be linked.
Retrieved from the registry, the priority category is a composite variable based on clinical information. The observation that higher priority patients were more likely to undergo CABG through direct admission indicates that the degree of misclassification of priority was likely small.
Several studies have shown that, when compared with medical charts, comorbid medical conditions are underreported in hospital discharge databases among persons discharged with cardiovascular diagnoses or procedures (Levy et al. 1999; Humphries et al. 2000; Austin, Daly, and Tu 2002; Quan, Parsons, and Ghali 2002). However, this unlikely affected our results, as the effect of study variables was similar before and after adjustment for comorbidity.
Our findings have implications for policies on access to elective cardiac surgery in a network of hospitals. If queue length varies significantly from hospital to hospital, policy makers may consider redistribution of cases across hospitals with the aim of reducing treatment delays. From the patients' perspective, as argued elsewhere, such a policy could infringe on the cardiologist's choice of a surgeon when referring a patient (Naylor 1991). Our results suggest that in order to make an informed decision on choosing a surgeon, cardiologists and patients should use information about the likely extent of treatment delay and associated risks. When projecting the expected time to treatment for patients who will be placed on the wait list, hospital managers should take into account the current list size as well as the weekly number of patients who require CABG immediately after undergoing coronary angiography.
More research is needed to evaluate whether waiting times for elective surgery vary because of chance alone after adjustment for clinical factors and variation in demand. One important issue is preferential allocation of hospital resources (Alter, Basinski, and Naylor 1998). It remains unclear whether directly admitting patients of low priority is done in order to circumvent long wait lists, or to substitute for cancellations on the operating room schedule. Other remaining questions include whether referral patterns across hospitals depend on wait-list size.
Acknowledgments
This research was supported by the Canada Research Chair Program (B.S.), the Michael Smith Foundation for Health Research Scholar Program (A.L.), and Canadian Foundation for Innovation (B.S., A.L.). The following cardiac surgeons are members of the BCCR Surgical Research Committee: Drs. James Abel, Richard Brownlee, Larry Burr, Anson Cheung, James Dutton, Guy Fradet, Virginia Gudas, Robert Hayden, Eric Jamieson, Michael Janusz, Shahzad Karim, Tim Latham, Jacques LeBlanc, Sam Lichtenstein, Hilton Ling, John Ofiesh, Michael Perchinsky, Peter Skarsgard, and Frank Tyers. We are grateful to anonymous external referees for thoughtful and detailed reviews. We would also like to thank the HSR editors for helpful comments.
Notes
Levy et al. (1999) found no evidence of differential coding in discharge abstracts between teaching and community hospitals in Canada.
Before using Model II, we found that although the effect of larger batch size was significant for list-size category 1, the ORs showed no significant differences between batch sizes for list-size categories 2–4 (data not shown). The Wald test of equality of the ORs associated with batch size categories had a χ2 value of 1.2 (p=.27, 1 df) for list-size category 2, 0.3 (p=.57, 1 df) for category 3, and 2.0 (p=.16, 1 df) for category 4. Therefore, we estimated regression coefficients for batch-size categories in list-size category 1 only.
Information is routinely verified only for patient ID.
References
- Allison PD. “Discrete-Time Methods for the Analysis of Event Histories.”. In: Leinhardt S, editor. Sociological Methodology. San Francisco: Jossey-Bass; 1982. pp. 61–98. [Google Scholar]
- Alter DA, Basinski AS, Naylor CD. “A Survey of Provider Experiences and Perceptions of Preferential Access to Cardiovascular Care in Ontario, Canada.”. Annals of Internal Medicine. 1998;129(7):567–72. doi: 10.7326/0003-4819-129-7-199810010-00011. [DOI] [PubMed] [Google Scholar]
- Austin PC, Daly PA, Tu JV. “A Multicenter Study of the Coding Accuracy of Hospital Discharge Administrative Data for Patients Admitted to Cardiac Care Units in Ontario.”. American Heart Journal. 2002;144(2):290–6. doi: 10.1067/mhj.2002.123839. [DOI] [PubMed] [Google Scholar]
- Bland JM, Altman DG. “Survival Probabilities (the Kaplan–Meier Method).”. British Medical Journal. 1998;317(7172):1572. doi: 10.1136/bmj.317.7172.1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland JM, Altman DG. “The Logrank Test.”. British Medical Journal. 2004;328(7447):1073. doi: 10.1136/bmj.328.7447.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clover KA, Dobbins TA, Smyth TJ, Sanson-Fisher RW. “Factors Associated with Waiting Time for Surgery.”. The Medical Journal of Australia. 1998;169(9):464–8. doi: 10.5694/j.1326-5377.1999.tb127867.x. [DOI] [PubMed] [Google Scholar]
- DeCoster C, Carriere KC, Peterson S, Walld R, MacWilliam L. “Waiting Times for Surgical Procedures.”. Medical Care. 1999;37(6 suppl):JS187–205. doi: 10.1097/00005650-199906001-00016. [DOI] [PubMed] [Google Scholar]
- Grech ED. “Pathophysiology and Investigation of Coronary Artery Disease.”. British Medical Journal. 2003;326(7397):1027–30. doi: 10.1136/bmj.326.7397.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton DM, Breslawski S. “Operating Room Scheduling. Factors to Consider.”. AORN Journal. 1994;59(3):665–80. doi: 10.1016/s0001-2092(07)69983-9. [DOI] [PubMed] [Google Scholar]
- Humphries KH, Rankin JM, Carere RG, Buller CE, Kiely FM, Spinelli JJ. “Co-Morbidity Data in Outcomes Research: Are Clinical Data Derived from Administrative Databases a Reliable Alternative to Chart Review?”. Journal of Clinical Epidemiology. 2000;53(4):343–9. doi: 10.1016/s0895-4356(99)00188-2. [DOI] [PubMed] [Google Scholar]
- Katz SJ, Mizgala HF, Welch HG. “British Columbia Sends Patients to Seattle for Coronary Artery Surgery. Bypassing the Queue in Canada.”. Journal of the American Medical Association. 1991;266(8):1108–11. [PubMed] [Google Scholar]
- Levy A, Sobolev B, Hayden R, Kiely M, FitzGerald M, Schechter M. “Time on Wait Lists for Coronary Bypass Surgery in British Columbia, Canada, 1991–2000.”. BMC Health Services Research. 2005;5:22. doi: 10.1186/1472-6963-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy AR, Tamblyn RM, Fitchett D, McLeod PJ, Hanley JA. “Coding Accuracy of Hospital Discharge Data for Elderly Survivors of Myocardial Infarction.”. Canadian Journal of Cardiology. 1999;15(11):1277–82. [PubMed] [Google Scholar]
- Mayo NE, Scott SC, Shen N, Hanley J, Goldberg MS, MacDonald N. “Waiting Time for Breast Cancer Surgery in Quebec.”. Canadian Medical Association Journal. 2001;164(8):1133–8. [PMC free article] [PubMed] [Google Scholar]
- Naylor CD. “A Different View of Queues in Ontario.”. Health Affairs. 1991;10(3):110–28. doi: 10.1377/hlthaff.10.3.110. [DOI] [PubMed] [Google Scholar]
- Noseworthy TW, McGurran JJ, Hadorn DC. “Waiting for Scheduled Services in Canada: Development of Priority-Setting Scoring Systems.”. Journal of Evaluation in Clinical Practice. 2003;9(1):23–31. doi: 10.1046/j.1365-2753.2003.00377.x. [DOI] [PubMed] [Google Scholar]
- Pell JP, Pell AC, Norrie J, Ford I, Cobbe SM. “Effect of Socioeconomic Deprivation on Waiting Time for Cardiac Surgery: Retrospective Cohort Study.”. British Medical Journal. 2000;320(7226):15–8. doi: 10.1136/bmj.320.7226.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quan H, Parsons GA, Ghali WA. “Validity of Information on Comorbidity Derived Rom ICD-9-CCM Administrative Data.”. Medical Care. 2002;40(8):675–85. doi: 10.1097/00005650-200208000-00007. [DOI] [PubMed] [Google Scholar]
- Romano PS, Roos LL, Jollis JG. “Adapting a Clinical Comorbidity Index for Use with ICD-9-CM Administrative Data: Differing Perspectives.”. Journal of Clinical Epidemiology. 1993;46(10):1075–9. doi: 10.1016/0895-4356(93)90103-8. [DOI] [PubMed] [Google Scholar]
- Sobolev B, Brown P, Zelt D. “Variation in Time Spent on the Waiting List for Elective Vascular Surgery: A Case Study.”. Clinical and Investigative Medicine. 2000;23(4):227–38. [PubMed] [Google Scholar]
- Sobolev B, Brown P, Zelt D. “Modeling and Analysis of Multistate Access to Elective Surgery.”. Health Care Management Science. 2001;4(2):125–32. doi: 10.1023/a:1011457627757. [DOI] [PubMed] [Google Scholar]
- Sobolev B, Brown P, Zelt D, Shortt S. “Access to Elective Vascular Surgery within the Recommended Time According to Emergency Referrals.”. Clinical and Investigative Medicine. 2001;24(5):236–41. [PubMed] [Google Scholar]
- Sykora K, Slaughter PM, Young W, Garlin D, Naylor CD. “Waiting Lists for Cardiac Surgery.”. In: Naylor CD, Slaughter PM, editors. Cardiovascular Health and Services in Ontario: An ICES Atlas. Toronto: Institute for Clinical Evaluative Sciences; 1999. pp. 239–54. [Google Scholar]
- Thomas SJ, Williams MV, Burnet NG, Baker CR. “How Much Surplus Capacity Is Required to Maintain Low Waiting Times? ”. Clinical Oncology (Royal College of Radiologists [Great Britain]) 2001;13(1):24–8. doi: 10.1053/clon.2001.9210. [DOI] [PubMed] [Google Scholar]