Abstract
Objective
To compare the extent with which child-only and family coverage (child and parent insured) ensure health care access and use for low income children in California and discuss the policy implications of extending the State Children's Health Insurance Program (California's Healthy Families) to uninsured parents of child enrollees.
Data Sources/Setting
We used secondary data from the 2001 California Health Interview Survey (CHIS), a representative telephone survey.
Study Design
We conducted a cross-sectional study of 5,521 public health insurance–eligible children and adolescents and their parents to examine the effects of insurance (family coverage, child-only coverage, and no coverage) on measures of health care access and utilization including emergency room visits and hospitalizations.
Data Collection
We linked the CHIS adult, child, and adolescent datasets, including the adolescent insurance supplement.
Findings
Among the sampled children, 13 percent were uninsured as were 22 percent of their parents. Children without insurance coverage were more likely than children with child-only coverage to lack a usual source of care and to have decreased use of health care. Children with child-only coverage fared worse than those with family coverage on almost every access indicator, but service utilization was comparable.
Conclusions
While extending public benefits to parents of children eligible for Healthy Families may not improve child health care utilization beyond the gains that would be obtained by exclusively insuring the children, family coverage would likely improve access to a regular source of care and private sector providers, and reduce perceived discrimination and breaks in coverage. These advantages should be considered by states that are weighing the benefits of expanding health insurance to parents.
Keywords: SCHIP expansions, healthy families, low-income families, insurance coverage, parents' insurance
In 2001, a peak performance year for California's economy, approximately 36 percent of California's families with children reported incomes near or below poverty (i.e., 200 percent of the federal poverty level [FPL] corresponding to ≤$35,300 for a family of four) (National Center for Children in Poverty 2001). Children in low-income families are at greater risk than nonpoor children of having special health needs related to chronic illness, disability, and social and behavioral problems, yet are less likely to access and utilize health care (Elixhauser et al. 2002; Testa et al. 2003). For instance, compared with nonpoor children, those in working poor families are twice as likely to lack a usual source of care and half as likely to have visited a dentist in a timely manner (Guendelman et al. 2005).
Insurance coverage is considered a key determinant of timely access and utilization of health services. In California, expansions in the State Children's Health Insurance Program (SCHIP, known as Healthy Families), and Medicaid (known as Medi-Cal), have enabled more children to qualify for public coverage. Medi-Cal is available to children under age 1 year in families with incomes under 200 percent of FPL, to children ages 1–5 years with family incomes under 133 percent of FPL, and to children ages 6–18 years with family incomes under 100 percent of FPL. Healthy Families extends public coverage to children under age 19 in families with incomes up to 250 percent of the FPL. Both programs provide comparable coverage. All citizen and legal resident children, regardless of date of arrival, are eligible. But although steps have been taken to minimize barriers to enrollment through outreach, on-line applications, and multilingual staff and forms, it is estimated that up to 30 percent of eligible children have yet to enroll (Brown et al. 2003). Many families cannot afford the Healthy Families monthly premiums (up to $27 per family, per month, depending on FPL) (Holahan, Dubay, and Kenney 2003). Families transitioning from welfare often fail to realize their continued eligibility for public health insurance and do not apply. Furthermore, confusion over eligibility, concerns with the immigration service, and mixed eligibility status among members of binational families act as deterrents to enrollment, particularly among Latinos (Berk et al. 2000; Holahan, Dubay, and Kenney 2003).
One promising avenue to increasing poor children's access to services is by improving their parents' insurance coverage. Evidence shows that among children eligible for Medicaid in 1999, take-up rates were 20 percentage points higher in states that expanded insurance coverage to parents than in states without parental coverage (Dubay and Kenney 2003). Guendelman and Pearl (2004) indicate that by extending health insurance coverage to working poor families, rather than exclusively to children, children experience fewer breaks in coverage and are more likely to be seen regularly at a doctor's office or HMO. Furthermore, Davidoff et al. (2001) and Gifford, Weech-Maldonado, and Short (2003) note that insured children with insured parents are more likely to receive well-child visits compared with children with uninsured parents.
Recent changes in federal policy provide federal matching dollars to states that want to expand coverage to parents under Medicaid and SCHIP. Since 2001, seven states have received federal approval to expand SCHIP enrollment. California passed a legislation in 2002 to extend Healthy Families to parents or guardians of eligible children. Because of a budget shortfall, implementation of this law has been postponed until 2006. Similar to public insurance programs in other states, Healthy Families could experience cut-backs, placing the health care needs of California's poor children at risk (Dubay and Kenney 2004).
In this paper we examine rthe extent to which improvement in access and use of health care among low-income California children could be expected by extending public health insurance coverage to parents, and discuss the implications for other states. We use data from the 2001 California Health Interview Survey (CHIS) to address the following questions:
To what extent does insurance coverage targeted only for individual children and not their parents secure access to care and utilization for California's low-income children?
Would access to and use of health care for children increase if a parent were also covered by health insurance?
STUDY METHODS
Sample and Data Source
CHIS is a representative telephone survey conducted in seven languages; its methodology has been described in several reports (CHIS 2002a;–c). From November 2000 to September 2001, interviewers used random digit dialing to contact 55,428 residential California households. The sample was proportionally distributed by county and aggregates of smaller counties, with supplemental samples of selected Asian and native populations and residents of selected cities. One adult per household was randomly selected for interviewing. In those households with children (under age 12) or adolescents (ages 12–17), one child and one adolescent were randomly selected for a more in-depth interview yielding 18,393 participants.
CHIS provides estimated racial/ethnic and income distributions of California's population that are similar to those provided by the 2000 Census (CHIS 2003b). Moreover, the health characteristics and behaviors of respondents are comparable with those found in other surveys (CHIS 2003b). Compared with other large California telephone surveys, the overall weighted response rate for CHIS was 38 percent (CHIS 2003a).
After dropping 11,422 records at or above 200 percent of the FPL, 182 records not matched to a parent or guardian (hereafter called parent), and an additional 98 records missing parents's immigrant status, our sample consisted of 6,691 children and adolescents in families with annual incomes under 200 percent of the FPL. As the federal law prohibits federal dollars to cover undocumented immigrants, we included only those children and adolescents with legal immigration status (citizen, naturalized citizen, or documented immigrant), who had at least one parent with legal immigrant status, which would make that parent eligible for family coverage (n=5,727). The remaining 964 children and adolescents were from families who were ineligible for public coverage because of child/adolescent undocumented immigrant status (n=103), parents's undocumented immigrant status (n=566), or both (n=295).
Information on the child was collected through the parent who was most knowledgeable about the child at the time of the interview. All adolescent data were collected through direct interviews except for insurance coverage information, which was provided by the parent. Children and adolescents (hereafter collectively called children) were considered insured if their parental respondent reported they were insured at the time of the interview. Parents were considered insured if the responding parent reported being insured or that their spouse was insured by an employer or union at the time of the interview. Individual insurance status (insured/uninsured) and insurance type were obtained by combining several questions on insurance coverage into mutually exclusive categories using the following hierarchy: Medi-Cal, Healthy Families, Medicare, employer-sponsored insurance (ESI), other coverages, and uninsured. That is, individuals receiving Medi-Cal, even if they received other types, were assigned to the Medi-Cal category; those that did not receive Medi-Cal but received Healthy Families were assigned to the Healthy Families category, etc. The same hierarchy was used to resolve parental insurance type in the event that one parent had public and one parent had private coverage. Parental and child insurance statuses were combined to yield the following study groups from the sample of children from eligible families:
Family coverage (n=4,241): Both child and at least one parent are insured.
Child-only coverage (n=721): The child but not the parent(s) has insurance coverage.
No family coverage (n=559): Neither the child nor the parent(s) reports insurance coverage.
The small group of children with parent-only coverage (n=206) was excluded from the analyses because estimates were unreliable and this group does not provide a comparison relevant with the research questions, leaving 5,521 children in the three study groups used for the main analysis.
Conceptual Model
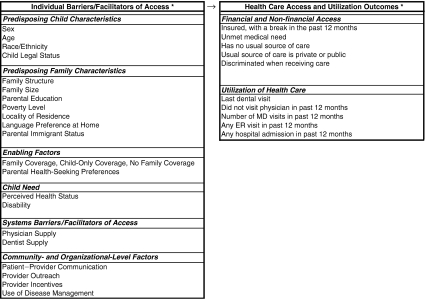
Guided by the Aday, Anderson, Fleming (1980), Andersen et al. (1983) framework, we distinguish two dimensions of health care access: (a) potential entry into care (i.e., financial and nonfinancial access to care) and, (b) actual entry into care or health care utilization. According to this framework, several characteristics of the health care delivery system and of the population-at-risk act as barriers and facilitators of potential access and use. As shown in Figure 1, we used several population measures to reflect each component of the model, including child and family attributes thought to “predispose” a child or parent to seek care for the child, enabling factors that provide the means for service use, and the child's need for care as reflected by the child's health status. Availability of health care resources was measured by the average number of practicing physicians (total patient care, nonfederal, 2001) and dentists (total private practice, 1998) at the county level per 100,000 noninstitutionalized residents. Supply-side data were obtained from the Area Resource File (2001). We lacked more refined organizational measures of dental or medical practices such as outreach, use of disease management, provider incentives, or patient–provider communication, which would help us assess performance, quality of care, or patient satisfaction. Also lacking were measures of parental health-seeking preferences that could influence health care use by the child.
Figure 1.
Conceptual Model
Data Analysis
We first compared children's insurance status and type of coverage (private, public) by parental insurance status and type of coverage for all children from eligible families. We then compared the sociodemographic characteristics, access, and health care utilization measures for the three study groups (family coverage, child-only coverage, no family coverage) among children from eligible families. Chi-square tests, adjusted for complex design effects as explained below, were performed for differences in proportions between study groups, and we indicate statistically significant differences (p≤.05) in the tables.
We used a logistic regression model for each access to care and utilization outcome to determine whether differences between children from eligible families in the three study groups persisted after adjusting for child (age, sex, race/ethnicity, perceived health status), family characteristics (household size, family structure, language preference at home, poverty level, parental education, and parental immigrant status), and supply variables (physicians, dentists). These variables have been shown to influence health care access and use (Wennberg, Freeman, and Culp 1987; Halfon, Inkelas, and Wood 1995; Guendelman, Schauffler, and Pearl 2001; Granados et al. 2001; Ku and Matani 2001; Holahan and Pohl 2002), and many were significant at p≤.05 in the bivariate models.
We used the following equations, reflecting a standard logistic regression approach (Hosmer and Lemeshow 1989), to model the likelihood for each child (indexed by i) of each outcome (indexed by k):
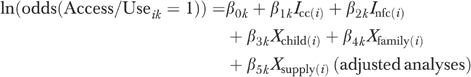
|
where ln(odds(Access/Useik=1))=ln(p/(1−p)) with p=Probability(Access/Useik=1), and Access/Useik=1 if child i was reported as not utilizing health care service or experiencing, health care access barrier k, 0 otherwise; Icc(i)=1 if child i, but not the parent(s), is insured (child-only coverage), 0 otherwise; Ifc(i)=1 if child i and at least one parent are insured (family coverage), 0 otherwise; Xchild(i), Xfamily(i), and Xsupply(i) are vectors of child, family, and supply characteristics for child i; β0k is the log odds of outcome k for children with family coverage (estimated); β1k, β2k the increases in log odds of outcome k if child-only or no family coverage (estimated); β3k, β4k, β5k indicates effects on log odds from child, family, and supply characteristics (estimated). To account for multiple comparisons, for each outcome k we tested the null hypothesis that there were no differences between the three study groups (H0k: β1k=β2k=0), both before and after adjusting for child and family characteristics, using χ2 tests and Wald tests adjusted for complex design effects. We further tested whether the effect of parent/child insurance status on the outcomes differed by type of parental insurance coverage (public versus private) (statistical interaction tests).
Subsequently, we did exploratory analyses to estimate possible changes in the outcomes provided eligibility for public insurance was extended to undocumented families. We examined differences between ineligible and eligible children by adding the previously excluded children with comparable insurance status from ineligible families to the sample, and substituted the eligibility variable for the three study groups as the main predictor of interest in the regression models. We used the following equation:
where Iinelg(i)=1 if the child was from a family ineligible for public coverage, 0 otherwise; β00k is the log odds of outcome k for children eligible for coverage (estimated); β5k the increases in log odds of outcome k if the child is ineligible (estimated); and other variables are interpreted as above. We reran the logistic regression model for each access and utilization outcome to compare eligible and ineligible children.
All estimation procedures used individual weights to compensate for differential sampling probabilities. The weights were constructed to reflect statewide population estimates reported in the 2000 Census, as well as selection probability, response bias, nontelephone coverage, and sampling design. Standard errors, confidence intervals, and bivariate and multivariate tests were further corrected for the complex survey design, which included clustering within households. The analyses were conducted using SAS (SAS Institute 2003) and STATA (STATA Corporation 2002) versions 8.0.
We note that while health insurance reflects coverage at the time of the interview, access, and use are assessed in the past year. Although much of our discussion interprets our findings as reflecting the causal relationship between insurance coverage and the outcomes, we cannot prove this with our data.
RESULTS
Health Insurance Coverage
Among low-income children in our sample, 13 percent were uninsured, 54 percent were covered by public insurance, and one-third were privately insured (Table 1). Insurance coverage was lower among the parents (22 percent uninsured); fewer parents compared with children had public insurance (39 percent) and a higher proportion had private insurance (39 percent). One out of seven insured children had an uninsured parent, reflecting mixed patterns of insurance coverage within families. Nonetheless, there was a strong relationship between parental and child health insurance status (p<.001). While the majority of uninsured children (72 percent) had uninsured parents, 20 percent of uninsured children had privately insured parents, and 8 percent had publicly insured parents. The majority of publicly insured children also had parents with public insurance (66 percent), but 14 percent had parents with private insurance and 20 percent had uninsured parents. And, children who were privately insured were most likely to have privately insured parents (87 percent) with 8 and 5 percent having publicly insured or uninsured parents, respectively.
Table 1.
Children's Insurance Status and Type of Coverage by Parental Insurance Status and Type of Coverage among Poor Families in California, 2001 (N=5,727)*
| Children's Insurance Status | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Combined | Insured Private | Insured Public | Uninsured | |||||||||
| N | %† | SE† | n | %† | SE† | n | %† | SE† | n | %† | SE† | |
| Total | 5,727 | 100.0 | 0 | 2,016 | 32.9 | 1.0 | 2,946 | 53.8 | 1.1 | 765 | 13.3 | 0.7 |
| Parent's insurance status | ||||||||||||
| Insured | ||||||||||||
| Private | 2,329 | 38.9 | 1.1 | 1,711 | 87.2 | 1.1 | 479 | 14.3 | 1.0 | 139 | 19.5 | 2.4 |
| Public | 2,118 | 39.1 | 1.1 | 172 | 7.6 | 0.9 | 1,879 | 65.9 | 1.4 | 67 | 8.3 | 1.8 |
| Uninsured | 1,280 | 22.0 | 0.9 | 133 | 5.2 | 0.7 | 588 | 19.9 | 1.2 | 559 | 72.2 | 2.7 |
Eligible families (N=5,727): below 200% FPL, both child and≥1 parent with legal citizen/immigrant status.
Corrected for complex design effects using weighted and/or clustered analyses.
FPL, federal poverty level.
Sociodemographic Characteristics by Insurance Status
The three groups differed in their sociodemographic characteristics. Children with no family coverage (Table 2, column 3) were more likely than children with child-only coverage (column 2) to be older, white or of “other” race/ethnicity and in fair or poor health. Compared with children with family coverage (column 1), children with no family coverage (column 3) were more likely to be adolescents, Latinos, in fair or poor health, to have parent(s) who had not completed high school, and to live in two-parent households, where no English was spoken at home, and in which at least one parent was an immigrant. A Latino, immigrant background and parental low-educational attainment also distinguished children with child-only coverage (column 2) from children with family coverage (column 1). In addition, among children under age 12, those with child-only coverage were less likely to report a disability. All differences were statistically significant (p≤.05).
Table 2.
Sociodemographic Characteristics by Child/Parent Insurance Status, among Children in Poor Families in California, 2001 (N=5,521)*
| 1 (n=4,241) Family Coverage | 2 (n=721) Child-Only Coverage | 3 (n=559) No Family Coverage | |||||
|---|---|---|---|---|---|---|---|
| %† | SE† | %† | SE† | %† | SE† | p-value≤.05* | |
| Sex | |||||||
| Male | 50.6 | 1.1 | 51.2 | 2.7 | 47.6 | 3.2 | |
| Female | 49.4 | 1.1 | 48.8 | 2.7 | 52.4 | 3.2 | |
| Age (years) | a,b | ||||||
| Under 7 | 40.2 | 1.2 | 44.4 | 2.8 | 30.3 | 2.7 | |
| 7–11 | 29.5 | 1.0 | 28.1 | 2.2 | 31.9 | 2.7 | |
| 12–17 | 30.4 | 1.0 | 27.5 | 2.3 | 37.8 | 2.9 | |
| Race/ethnicity | |||||||
| White | 27.3 | 1.0 | 17.5 | 2.0 | 21.7 | 2.7 | a,b,c |
| Latino | 48.6 | 1.3 | 70.5 | 2.5 | 67.8 | 3.0 | |
| African American | 12.0 | 0.9 | 5.4 | 1.4 | 2.6 | 0.9 | |
| Asian | 8.4 | 0.8 | 4.6 | 1.1 | 3.2 | 1.0 | |
| Other | 3.7 | 0.4 | 2.0 | 0.6 | 4.8 | 1.3 | |
| Perceived health status | a,b | ||||||
| Fair, poor | 12.0 | 0.8 | 9.8 | 1.5 | 17.2 | 2.7 | |
| Excellent, very good, good | 88.0 | 0.8 | 90.2 | 1.5 | 82.8 | 2.7 | |
| Disability (<age 12, only) | c | ||||||
| Disabled | 7.7 | 0.8 | 3.8 | 0.9 | 4.0 | 2.3 | |
| Not disabled | 92.3 | 0.8 | 96.2 | 0.9 | 96.0 | 2.3 | |
| Family structure | b,c | ||||||
| Single-parent household | 36.4 | 1.3 | 27.1 | 2.8 | 24.9 | 2.9 | |
| Two-parent household | 63.6 | 1.3 | 73.0 | 2.8 | 75.1 | 2.9 | |
| Family size | |||||||
| ≤3 | 14.7 | 0.7 | 13.8 | 1.5 | 12.6 | 1.5 | |
| 4–5 | 49.0 | 1.3 | 54.8 | 2.9 | 48.4 | 3.4 | |
| ≥6 | 36.3 | 1.4 | 31.4 | 3.0 | 39.0 | 3.6 | |
| Parental education | b,c | ||||||
| ≤11 years | 36.3 | 1.3 | 51.0 | 2.9 | 50.4 | 3.4 | |
| High school | 33.4 | 1.2 | 29.1 | 2.7 | 24.3 | 2.7 | |
| 13+ years | 30.3 | 1.1 | 19.9 | 2.1 | 25.3 | 2.9 | |
| Poverty level (%) | |||||||
| <100 | 45.0 | 1.3 | 46.6 | 2.9 | 47.9 | 3.4 | |
| 100–199 | 55.0 | 1.3 | 53.5 | 2.9 | 52.1 | 3.4 | |
| Locality of residence | |||||||
| Urban | 84.0 | 0.8 | 81.9 | 2.0 | 83.3 | 2.3 | |
| Rural | 16.0 | 0.8 | 18.1 | 2.0 | 16.7 | 2.3 | |
| Language preference at home | b,c | ||||||
| Some English | 82.7 | 1.0 | 67.1 | 2.7 | 74.0 | 3.0 | |
| No English | 17.3 | 1.0 | 32.9 | 2.7 | 26.1 | 3.0 | |
| Child legal status | c | ||||||
| U.S. born | 94.8 | 0.5 | 91.6 | 1.7 | 92.4 | 1.4 | |
| Naturalized | 2.8 | 0.4 | 2.6 | 0.9 | 2.9 | 0.9 | |
| Legal immigrant with green card | 2.4 | 0.3 | 5.8 | 1.5 | 4.7 | 1.2 | |
| Parental immigrant status | b,c | ||||||
| At least one immigrant parent | 41.4 | 1.3 | 66.9 | 2.6 | 61.1 | 3.3 | |
| Both parents nonimmigrant | 58.6 | 1.3 | 33.1 | 2.6 | 39.0 | 3.3 | |
| Mean number of physicians per county per 100,000 people (patient care, non-federal, 2001) | 197.8 (mean) | 1.4 | 195.6 (mean) | 3.0 | 195.2 (mean) | 3.3 | |
| Mean number of dentists per county per 100,000 people (private practice, 1998) | 47.0 (mean) | 0.3 | 45.8 (mean) | 0.6 | 46.3 (mean) | 0.7 | |
Source: California Health Interview Survey (CHIS 2001).
Eligible families (N=5,521): below 200% FPL, both child and≥1 parent with legal citizen/immigrant status; excludes small group of uninsured children with insured parents (n=206).
corrected for complex design effects using weighted and/or clustered analyses.
p-value for differences in group 3 versus 2.
p-value for differences in group 3 versus 1.
p-value for differences in group 2 versus 1.
FPL, federal poverty level.
Differences in Access and Utilization among Uninsured and Insured Children
Children with no family coverage were significantly more likely to experience access and utilization barriers than children who were insured through child-only or through family coverage, both unadjusted (Table 3, first three columns) and adjusted (final three columns). Compared with children with child-only coverage, children with no family coverage had higher odds of lacking a usual source of care and of not having seen a dentist within the last 2 years or a physician in the last year, after controlling for covariates (column 3 versus 2). Furthermore, among children under age 12, the number of physician visits was lower, and remained lower even after controlling for covariates. Even among children in fair to poor health, those with no family coverage had triple the odds of foregoing a physician visit compared with children with child-only coverage. And, among children in excellent to good health, children with no family coverage had half the odds of those with child-only coverage to seek an emergency room (ER) visit.
Table 3.
Access to and Use of Health Care Services by Child/Parent Insurance Status, among Children in Poor Families in California, 2001 (N=5,521)*
| Unadjusted for Covariates | Adjusted for Covariates | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 (n=4,241) Family Coverage | 2 (n=72) Child-Only Coverage | 3 (n=559) No Family Coverage | |||||||||
| %† | SE† | %† | SE† | %† | SE† | p<.05 | 3 versus 2 No Family versus Child-Only Coverage OR‡ (95% CI) | 3 versus 1 No Family versus Family Coverage OR‡ (95% CI) | 2 versus 1 Child-Only versus Family Coverage Coverage OR‡ (95% CI) | p<.05 | |
| Access indicators | |||||||||||
| Insured, with a break in the past 12 months | 5.7 | 0.6 | 18.1 | 2.1 | NA | NA | c | NA | NA | 3.6 (2.5,5.1) | ∥ |
| Unmet medical need | 7.4 | 0.6 | 8.3 | 1.3 | 8.8 | 1.5 | 0.9 (0.5,1.5) | 1.3 (0.8,1.9) | 1.4 (0.9,2.1) | ||
| Has no usual source of care | 5.2 | 0.5 | 10.4 | 1.7 | 27.2 | 3.0 | a,b,c¶ | 2.9 (1.7,4.9) | 6.5 (4.3,9.9) | 2.2 (1.4,3.5) | ∥ |
| Usual source of care | b,c¶ | 1.1 (0.8,1.7) | 1.7 (1.2,2.4) | 1.5 (1.2,2.0) | ∥ | ||||||
| Private | 59.1 | 1.3 | 42.9 | 2.8 | 40.0 | 3.7 | |||||
| Public | 41.0 | 1.3 | 57.1 | 2.8 | 60.0 | 3.7 | |||||
| Discriminated when receiving care | 2.0 | 0.3 | 3.7 | 0.9 | 3.2 | 0.8 | ¶ | 0.8 (0.4,1.8) | 1.9 (1.0,3.4) | 2.2 (1.2,4.0) | ∥ |
| Traveled to another country for care | 1.1 | 0.3 | 3.2 | 1.1 | 5.7 | 1.7 | b,c¶ | 1.5 (0.6,3.8) | 3.4 (1.6,7.6) | 2.3 (1.0,5.3) | ∥ |
| Use indicators | |||||||||||
| Last dental visit (for those aged >2 years) | a,b¶ | 2.5 (1.6,4.0) | 2.5 (1.8,3.6) | 1.0 (0.7,1.5) | ∥ | ||||||
| 1 month to 2 years | 84.2 | 1.0 | 82.2 | 2.3 | 72.4 | 2.8 | |||||
| >2 years/never | 15.8 | 1.0 | 17.8 | 2.3 | 27.6 | 2.8 | |||||
| Did not visit physician in past 12 months | 12.6 | 0.8 | 13.2 | 1.9 | 28.3 | 2.8 | a,b¶ | 2.3 (1.5,3.6) | 2.5 (1.8,3.6) | 1.1 (0.8,1.6) | ∥ |
| Fair/poor health | 14.3 | 2.6 | 9.0 | 3.5 | 30.0 | 8.0 | a,b¶ | 3.1 (1.1,8.9) | 3.1 (1.3,7.2) | 1.0 (0.4,2.7) | ∥ |
| Excellent/very good/good health | 12.3 | 0.8 | 13.6 | 2.0 | 28.0 | 3.0 | a,b¶ | 2.2 (1.3,3.6) | 2.4 (1.7,3.6) | 1.1 (0.8,1.6) | ∥ |
| Number of MD visits in past 12 months for children <12 years | a,b¶ | 0.5 (0.3,0.8) | 0.4 (0.3,0.6) | 0.8 (0.6,1.1) | ∥ | ||||||
| 0 | 8.3 | 0.8 | 7.5 | 1.7 | 25.2 | 3.3 | § | § | § | ||
| 1 | 24.2 | 1.3 | 21.0 | 2.7 | 26.8 | 3.5 | |||||
| 2–3 | 34.2 | 1.3 | 42.6 | 3.1 | 30.5 | 3.3 | |||||
| 4+ | 33.4 | 1.3 | 28.9 | 2.7 | 17.5 | 2.7 | |||||
| ER visit in past 12 months | 21.5 | 1.0 | 18.2 | 2.0 | 13.0 | 2.1 | ¶ | 0.6 (0.4,1.0) | 0.6 (0.4,0.9) | 1.0 (0.7,1.3) | ∥ |
| Fair/poor health | 33.3 | 3.6 | 23.4 | 6.4 | 22.2 | 7.9 | 0.8 (0.3,2.2) | 0.7 (0.3,1.5) | 0.8 (0.4,1.8) | ||
| Excellent/very good/good health | 19.9 | 1.0 | 17.6 | 2.1 | 11.1 | 1.9 | a,b¶ | 0.5 (0.3,0.9) | 0.6 (0.4,0.8) | 1.0 (0.7,1.4) | ∥ |
| Hospital admission in past 12 months | 5.1 | 0.6 | 5.9 | 1.2 | 4.9 | 1.6 | 0.8 (0.3,1.7) | 1.0 (0.5,2.1) | 1.3 (0.8,2.1) | ||
| Fair/poor health | 11.2 | 2.6 | 10.7 | 3.9 | 12.9 | 7.7 | 1.2 (0.3,4.0) | 1.6 (0.6,4.4) | 1.3 (0.5,3.5) | ||
| Excellent/very good/good health | 4.2 | 0.5 | 5.4 | 1.3 | 3.2 | 1.0 | 0.6 (0.3,1.4) | 0.8 (0.4,1.6) | 1.3 (0.7,2.2) | ||
Source: California Health Interview Survey (CHIS 2001).
Eligible families (N=5,521): below 200% FPL, both child and≥1 parent with legal citizen/immigrant status; excludes small group of uninsured children with insured parents (n=206).
Corrected for complex design effects using weighted and/or clustered analyses.
Adjusted for age, sex, race/ethnicity, parent education, parent immigrant status, poverty level, language, household size, family structure, perceived health status (where appropriate), physicians per county per 100,000 (or dentists per county per 100,000 for last dental visit), and complex design effects.
The reference group for number of MD visits is <4 visits.
p-value for differences in group 3 versus 2 (no family versus child-only coverage).
p-value for differences in group 3 versus 1 (no family versus family coverage).
p-value for differences in group 2 versus 1 (child-only versus family coverage).
p-value≤.05 for the null hypothesis that the three study groups do not differ in analyses unadjusted (¶) or adjusted (∥) for covariates.
FPL, federal poverty level.
Children with no family coverage were at an even greater disadvantage compared with children with family coverage (columns 3 versus 1). Children with no family coverage had over six times the odds of lacking a usual source of care after controlling for other covariates, and if they had a usual source, they were more likely to seek care in the public sector. Furthermore, after controlling for covariates, children without family coverage had elevated odds of feeling discriminated when receiving care and of traveling to another country for care whereas they had a lower probability of seeking dental care or medical care in a timely manner. In addition, the number of physician visits was far lower for children under age 12 with no family coverage, even if in poor to fair health (OR=0.3, 95 percent CI=0.1, 0.7) (data not shown). The disparities in seeking any care from a physician were even greater after controlling for covariates among children in fair or poor health. And, for children with no family coverage, the odds of an ER visit in the past 12 months remained lower.
Differences in Access and Utilization among Insured Children
Compared with children with family coverage, those with child-only coverage had elevated odds of experiencing breaks in insurance coverage in the past year, of lacking a usual source of care, and among those who had a usual source, of seeking care in the public sector; those with child-only coverage also had higher odds of feeling discriminated when receiving care and of traveling abroad for care, after controlling for covariates (columns 2 versus 1). Despite these disparities in access, the two groups did not statistically significantly differ on utilization of health services, either before or after controlling for covariates.
Among children with family coverage, we can distinguish between those whose parent's insurance is either from a public source (Table 1, n=172+1,879=2,051) or a private source (n=1,711+479=2,190). The odds of breaks in insurance coverage (OR=1.7, 95 percent CI=1.1, 2.7), traveling abroad for care (OR=2.7, 95 percent CI=1.2, 6.4), and seeking a usual source of care in the public sector (OR=2.2, 95 percent CI=1.8, 2.8) were higher among children with public family coverage than with private family coverage. Moreover, children with public family coverage had a higher probability of having more than four annual physician visits (OR=1.6, 95 percent CI=1.2, 2.1), ER visits (OR=1.6, 95 percent CI=1.2, 2.0), and, among those in excellent to good health, ER visits (OR=1.5, 95 percent CI=1.2, 2.0) and hospital admissions (OR=1.7, 95 percent CI=1.0, 2.8) compared with children with private family coverage (adjusted analyses, data not shown).
Adjusting for Multiple Group Comparisons
The null hypothesis that there were no differences between the three study groups was rejected at the p≤.05 level for all outcomes that had demonstrated statistically significant differences between two groups (see Table 3, footnotes “§” and “‡”), exceeding the number that would be expected by chance.
Extending Eligibility to Undocumented Families
Among the ineligible families with an undocumented parent and/or child, 46 percent had family coverage, 24 percent had child-only coverage, and 22 percent had no coverage. For an additional 8 percent, only the parent was insured. Compared with children from families eligible for public insurance, children from ineligible families stood higher odds of lacking a usual source of care (OR=1.7, 95 percent CI=1.2, 2.3), of having a public source of usual care (OR=1.8, 95 percent CI=1.3, 2.3), of forgoing or postponing dental care (OR=1.6, 95 percent CI=1.2, 2.2), and of not seeking medical care in the past year if in excellent–good health (OR=1.5, 95 percent CI=1.1, 2.0), and had lower odds of traveling to another country for care (OR=0.3, 95 percent CI=0.1, 0.6) (adjusted analyses, data not shown).
DISCUSSION
California's efforts to insure low-income children through Medi-Cal and Healthy Families have contributed to marked gains in coverage over the past decade (Brown, Alex, and Becerra 2002). Yet our findings indicate that in 2001, 13 percent of children in families below 200 percent FPL eligible for public insurance were uninsured, lagging behind their insured counterparts in access and use of health care services. Children without insurance coverage are more likely to face barriers to access and utilization compared with children who are insured either through child-only coverage or family coverage.
Compared with children with child-only coverage, our findings show that children with no family coverage were more likely to lack a usual source of care, even after controlling for other health and demographic factors. A usual source of care has been shown to increase timely use of preventive health services and contributes to optimum management of chronic illnesses (Elixhauser et al. 2002). Children with no family coverage also showed large disparities when compared with children with child-only coverage in their use of health services. By increasing participation in Healthy Families, we would expect gains for previously uninsured children in access to a usual source of care and a narrowing in disparities in the timely use of dental care, physician care, and in the number of physician visits. As almost one out of five children in families with no coverage reportedly was in fair or poor health, improvements in these outcomes are particularly pressing.
Our findings also show that there are marked disparities in access and use among insured low-income children. Children with child-only coverage fared worse than those with family coverage on every access indicator, except unmet health care needs. By extending health insurance to both children and parents rather than only the child, we would anticipate a marked narrowing of disparities in breaks in insurance coverage, having a usual source of care, and perceived discrimination. Gaps in seeking a usual source of care in the private sector would also likely narrow further. Decreasing these disparities is important as evidence suggests that continuity of coverage and absence of perceived discrimination enables more consistent and trusting relationships with health care providers allowing for better preventive care and management of chronic conditions. While public sector providers often provide adequate care, public services tend to have increased wait times and overtaxed resources. Furthermore, parents covered by the same insurance as their children might be more effective advocates for care because they are familiar with the specific health insurance system (Hansen 1998; Davidoff et al. 2001). As utilization of services was found to be comparable among insured children regardless of parental insurance status, extending insurance to parents of children who are already insured would probably not impact on utilization of health care among insured low-income children. Nevertheless, families who switch from private family coverage to public family insurance coverage would likely experience increased barriers in access to care.
Compared with children with family coverage, those with child-only coverage or no coverage are more likely to be adolescents, Latino, immigrants, or to speak no English at home. Immigrants, particularly from Latin America, are a growing segment of the U.S. population and comprise over 30 percent of all Californians (U.S. Census Bureau 2002). New immigrants to California tend to be disproportionately represented among the poor and near poor, tend to hold jobs that offer few or no benefits, and have limited English skills. They also have high fertility rates and bear U.S. citizen children into households of mixed citizenship and thus mixed eligibility for services. Hence, these are the currently eligible children that in California may most likely benefit from increasing take-up rates of child-only or family insurance coverage. Were we to eliminate insurance barriers for undocumented families, we might expect narrowing inequalities becuase of an increased use of medical and dental care and access to a usual source of care.
Extending health insurance coverage to families would also benefit parents. Currently, there are no state provisions for insuring low-income adults who do not meet Medi-Cal criteria. Consequently, low-income parents are more likely than their children to be uninsured (Kaiser Commission on Medicaid and the Uninsured 2003; Dubay and Kenney 2004). The burden of paying out-of-pocket for medical care reaches far beyond financial costs. Low-income families may have to place other competing financial demands before parents' medical needs, or plunge further into poverty. Working, low-income parents with unmet health care needs may face decreased productivity at work and a decreased ability to care for their children, which may in turn impact their children's health.
Policy Implications
Our findings underscore the importance of instituting expansions to the Healthy Families program that were approved in 2002 and are pending implementation. An alternative strategy that has been considered, instating caps to Healthy Families enrollment, would result in approximately 300,000 eligible low-income children, who are not currently insured, being placed on the Healthy Families waiting list if they attempt to enroll (Testa et al. 2003). As expansions can only be deployed if all children applying for Healthy Families are enrolled, establishing a waiting list may void the federal government's approval to expand services to parents. Given that health insurance is one of the most important determinants of health care access and utilization (Newacheck et al. 1998), it is imperative that California continue efforts to enroll all eligible children and implement access expansions to their parents.
These findings have implications for other states that are facing budget shortfalls and are considering rolling back some of their health insurance expansions. The primary aim of SCHIP expansions to parents has been to increase enrollment by eligible children. Increased enrollment has been evidenced in states with parental expansions of public insurance (Dubay and Kenney 2003). Roll-backs could result in decreased coverage among low-income children, who are most likely to benefit from public health insurance.
Our findings must be interpreted cautiously. As noted earlier, CHIS is a cross-sectional survey with a single period, self-reported assessment of income, insurance status, and health access and utilization; a causal relationship cannot be established. As insurance may help children obtain health care while some may seek out or retain insurance because they need care, this may produce endogeneity problems. Overall, the result would be to overestimate the effect of health insurance on access and utilization. By limiting our sample to low-income children, we excluded children who most likely qualified for public insurance because of a disability or extraordinary health care needs. By adjusting for several covariates and stratifying for health status we attempted to equalize other factors that could influence the outcomes. But this may not accurately model the conditions that would occur were uninsured children to obtain insurance. In addition, the method we developed for classifying low-income children as belonging to families with child-only or family coverage may have been inexact and relied on self-reporting; thus, it may have been subject to error. Retrospective assessments are subject to recall error and misclassification (Infante-Revard and Jacques 2000).
Other measures of group membership such as being below 200 percent of FPL for 3 years rather than one, would possibly show even larger effects across the study groups than what we observed in so far as such measures might more fully reflect the adverse life effects of sustained poverty. And, although comparable with other large California telephone surveys, the overall response rate for CHIS was low (CHIS 2003a). Nonetheless, the completion rates among children and adolescents selected for the surveys in households with a responding adult were higher at 87.6 percent and 63.5 percent, respectively. The low response rate could be because of the growing use of answering machine-only telephone numbers, never answered numbers, and cellular phones as replacements for working household numbers. Under- sampling of households that lack telephones was taken into account by poststratification weights in CHIS. However, these weights may not adjust for all noncoverage effects. Household reliance on answering machines or cell phones could have yielded lower response rates, especially among the highly mobile, the undocumented, and full-time working parents. In addition, individuals with low education have been found to disproportionately refuse telephone interviews (Groves and Lyberg 1988). Furthermore, child and adolescent interviews required that a sampled adult in the household be interviewed first. If the adult interviewed was the most knowledgeable person about the child, then that adult was requested to complete the child interview, substantially adding to the interview burden. Adolescents could not be interviewed unless the parent verbally consented to the interview. These constraints could have increased refusal rates among overburdened parents or those unwilling to let teens participate in the study. Furthermore, our study lacked measures of parental health-seeking preferences, community and organizational-level variables. The organizational context in which physicians and dentists practice may be an important determinant of health care access (Grumbach, Vranizan, and Bindman 1997). Our findings show that children with no family coverage or child-only coverage had a higher likelihood of receiving care from a public source rather than a private physician office or HMO compared with children with family coverage. The extent to which this acts as an access barrier requires further investigation.
Acknowledging these caveats, our findings suggest that improving public health insurance take-up rates among eligible, uninsured low-income children in California will substantially increase their access and use of services and make them less likely to delay or miss preventive care opportunities. Benefits would most likely accrue to adolescents, Latinos, immigrants, and those in families with limited English, as these children are the most likely to face barriers to insurance coverage. While extending public benefits to parents of children eligible for Healthy Families may not improve health care utilization by children beyond the gains that would be obtained by exclusively insuring the children, family coverage would likely improve access to a regular source of care and private sector providers, and reduce perceived discrimination and breaks in coverage. These advantages should be considered by states that are weighing the benefits of expanding health insurance to parents.
Acknowledgments
This study was funded by the Agency for Healthcare Quality Research and supplemented by the Health Research Center and Latino Policy Research Center at the University of California at Berkeley.
References
- Aday LA, Andersen R, Fleming GV. Health Care in the U.S.: Equitable for Whom? Beverly Hills, CA: Sage; 1980. [Google Scholar]
- Andersen R, McCutcheon A, Aday LA, Chiu G, Bell R. “Exploring Dimensions of Access to Medical Care.”. Health Services Research. 1983;18(1):49–74. [PMC free article] [PubMed] [Google Scholar]
- Area Resource File. Health Resources and Services Administration, Bureau of Health Professions. Rockville, MD: U.S. Department of Health and Human Services; 2001. [Google Scholar]
- Berk ML, Schur CL, Chavez LR, Frankel M. “Health Care Use among Undocumented Latino Immigrants.”. Health Affairs. 2000;19(4):51–64. doi: 10.1377/hlthaff.19.4.51. [DOI] [PubMed] [Google Scholar]
- Brown ER, Alex S, Becerra L. Number of Uninsured Californians Declines to 6.2 Million–2 Million are Eligible for Medi-Cal or Healthy Families. Los Angeles: UCLA Center for Health Policy Research; 2002. [Google Scholar]
- Brown ER, Ponce N, Rice T, Lavarreda SA. The State of Health Insurance in California: Long-Term and Intermittent Lack of Health Insurance Coverage. Los Angeles, CA: UCLA Center for Health Policy Research; 2003. [Google Scholar]
- California Health Interview Survey (CHIS) CHIS 2001 Methodology Series: Report 1—Sample Design. Los Angeles: UCLA Center for Health Policy Research; 2002a. [Google Scholar]
- California Health Interview Survey (CHIS) CHIS 2001 Methodology Series: Report 2—Data Collection Methods. Los Angeles: UCLA Center for Health Policy Research; 2002b. [Google Scholar]
- California Health Interview Survey (CHIS) CHIS 2001 Methodology Series: Report 3—Response Rates. Los Angeles: UCLA Center for Health Policy Research; 2002c. [Google Scholar]
- California Health Interview Survey (CHIS) Los Angeles: UCLA Center for Health Policy Research; 2003a. Technical Paper No. 1. December. [Google Scholar]
- California Health Interview Survey (CHIS) The CHIS 2001 Sample: Response Rate and Representativeness. Los Angeles: UCLA Center for Health Policy Research; 2003b. [Google Scholar]
- Davidoff A, Kenney G, Dubay I, Yemane A. “Patterns of Child–Parent Insurance Coverage: Implications for Coverage Expansions.”. 2001. The Urban Institute, Series B, No. B-39.
- Dubay L, Kenney G. “Expanding Public Health Insurance to Parents: Effects on Children's Coverage under Medicaid.”. Health Services Research. 2003;38(5):1283–301. doi: 10.1111/1475-6773.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubay L, Kenney G. “Addressing Coverage Gaps for Low-Income Parents.”. Health Affairs. 2004;23(2):225–34. doi: 10.1377/hlthaff.23.2.225. [DOI] [PubMed] [Google Scholar]
- Elixhauser A, Machlin M, Chevarley F, Patel N, McCormick M, Simpson L. “Health Care for Children and Youth in the United States: 2001 Annual Report on Access, Utilization, Quality and Expenditures.”. Ambulatory Pediatrics. 2002;2:419–37. doi: 10.1367/1539-4409(2002)002<0419:hcfcay>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Gifford E, Weech-Maldonado R, Short PF. “Encouraging Preventive Services for Low-Income Children: Implications of Expanding Medicaid Coverage to Parents.”. 2003. Unpublished manuscript.
- Granados G, Puvvula J, Berman J, Dowling PT. “Health Care for Latino Children: Impact of Child and Parental Birthplace on Insurance Status and Access to Health Services.”. American Journal of Public Health. 2001;91(11):1806–7. doi: 10.2105/ajph.91.11.1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groves R, Lyberg L. “An Overview of Non-response Issues in Telephone Surveys.”. In: Groves RM, editor. Telephone Survey Methodology. New York: Wiley; 1988. pp. 191–212. [Google Scholar]
- Grumbach K, Vranizan K, Bindman A. “Physician Supply and Access to Care in Urban Communities.”. Health Affairs. 1997;16(1):71–86. doi: 10.1377/hlthaff.16.1.71. [DOI] [PubMed] [Google Scholar]
- Guendelman S, Angulo V, Oman D. “Access to Healthcare for Children and Adolescents in Working Poor Families: Recent Findings from California.”. Medical Care. 2005;43:68–78. [PubMed] [Google Scholar]
- Guendelman S, Pearl M. “Children's Ability to Access and Use Health Care.”. Health Affairs. 2004;23(2):235–44. doi: 10.1377/hlthaff.23.2.235. [DOI] [PubMed] [Google Scholar]
- Guendelman S, Schauffler H, Pearl M. “Unfriendly Shores: How Immigrant Children Fare in the U.S. Health System.”. Health Affairs. 2001;20(1):257–66. doi: 10.1377/hlthaff.20.1.257. [DOI] [PubMed] [Google Scholar]
- Halfon N, Inkelas M, Wood D. “Non-Financial Barriers to Care for Children and Youth.”. Annual Review of Public Health. 1995;16:447–72. doi: 10.1146/annurev.pu.16.050195.002311. [DOI] [PubMed] [Google Scholar]
- Hansen K. “Is Insurance for Children Enough? The Link between Parents' and Children's Health Care Use Revisited.”. Inquiry. 1998;35(3):294–302. [PubMed] [Google Scholar]
- Holahan J, Dubay L, Kenney G. The Future of Children Which Children Are Still Uninsured and Why. 1. Vol. 13. Los Altos, CA: The David and Lucille Packard Foundation; 2003. pp. 55–79. [PubMed] [Google Scholar]
- Holahan J, Pohl M. “Changes in Insurance Coverage: 1994–2000 and Beyond.”. Health Affairs. 2002;(web suppl, April 3):W162–W172. doi: 10.1377/hlthaff.w2.162. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied Logistic Regression. New York: Wiley; 1989. [Google Scholar]
- Infante-Revard C, Jacques L. “Empirical Study of Parental Recall Bias.”. American Journal of Epidemiology. 2000;152(5):480–6. doi: 10.1093/aje/152.5.480. [DOI] [PubMed] [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured. The Health Insurance Status of Low-Income Children and Their Parents: Recent Trends in Coverage and State-Level Data. Menlo Park, CA: Kaiser Family Foundation; 2003. [Google Scholar]
- Ku L, Matani S. “Left Out: Immigrants' Access to Health Care and Insurance.”. Health Affairs. 2001;20(1):247–56. doi: 10.1377/hlthaff.20.1.247. [DOI] [PubMed] [Google Scholar]
- National Center for Children in Poverty. “NCCP California Demographics”. [on 07 April 2004];2001 Available at http://www.nccp.org/state_detail_demographic_CA.html.
- Newacheck P, Stoddard J, Hughes D, Pearl M. “Health Insurance and Access to Primary Care for Children.”. The New England Journal of Medicine. 1998;338(8):512–9. doi: 10.1056/NEJM199802193380806. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS software. Cary; 2003. NC version 8/:SAS/ [Google Scholar]
- STATA Corporation. STATA Software. College Station: 2002. TX version 8/:STATA. [Google Scholar]
- Testa K, Mohamadi, Horner D, Lazarus W. Children Falling through the Health Insurance Cracks. Oakland, CA: 100% Campaign; 2003. [Google Scholar]
- U.S. Census Bureau. “American Community Survey Profile”. [on 03 May 2004];2002 Available at http://www.census.gov/acs/www/Products/Profiles/Single/2002/ACS/Tabular/040/04000US061.htm.
- Wennberg J, Freeman J, Culp W. “Are Hospital Services Rationed in New Havern or Over-Utilized in Boston?”. The Lancet. 1987;23:1185–8. doi: 10.1016/s0140-6736(87)92152-0. [DOI] [PubMed] [Google Scholar]