Abstract
Granulocytic sarcomas (chloromas) are rare extramedullary tumors consisting of primitive granulocytic cells. They arise de novo, or are associated with other hematologic disorders such as acute myeloid leukemia, myelodysplastic syndrome, or myeloproliferative disorders. We report here on a case of a 62-year-old woman who presented with a large swelling in her right groin and leg. The mass was confirmed by biopsy to be a granulocytic sarcoma. Bone marrow examination showed mild hypercellularity but no evidence of increase in blast count. However, cytogenetic examination of the marrow showed t(9;22), indicating an unexpected diagnosis of chronic myeloid leukemia.
Case Report
A 62-year-old female patient presented with a history of stiffness in both legs for 1 year, plus pain in the right groin for 3 months. On examination, a large mass was palpable in the right groin, and the right leg was swollen throughout. Blood count results were: Hb 10.1, WBC 10.4, plat 331, neut 8.2. A computed tomography (CT) scan of the pelvis showed a large soft tissue mass involving the anterior aspect of the acetabulum and hip joint on the right. It extended into the inguinal region and into the thigh with invasion of the right abdominal muscles. There was also invasion into the perineum, plus symphysis pubis and rectus sheath. The largest diameter is 12.5 × 10.3 cm.
The diagnosis at this stage was thought to be a non-hematologic malignancy, most likely an ovarian tumor, sarcoma, or a metastatic lesion.
Further investigations were performed to establish the diagnosis. These included:
A) CT Guided Biopsy
A biopsy was performed under CT guidance. The histology showed a tumor with nests and sheet of regular large cells (Figure 2). Immunohistochemistry was positive for CD 33, 34, 43, 45, and 68. Ki67 was 80%. This was consistent with a myeloid malignancy - an extramedullary myeloid tumor.
Figure 2.

Tru-cut biopsy histology of the tumor.
B) Bone Marrow Investigations
Bone marrow aspirate was performed to look for any evidence of an increased myeloblast population. Results showed only mild myeloid and eosinophilic hyperplasia (Figure 3). There was no evidence of acute myeloid leukemia. (BM immunophenotyping - CD34 blasts < 1%).
Figure 3.

Bone marrow aspirate morphology.
However, bone marrow cytogenetics subsequently demonstrated an unsuspected abnormality, t(9;22) (q34;q11) in 18/20 cells (Figure 4). This is the Philadelphia chromosome translocation associated with chronic myeloid leukemia (CML).
Figure 4.

Cytogenetics karyotype.
Fluorescent in-situ hybridization (FISH) investigation was performed on the marrow sample (Figure 5). This involves utilizing specific fluorescently labeled DNA probes, and adding them to the denatured DNA from the patient"s sample. The probe hybridizes with the sample DNA and the probe signal can be seen through a fluorescent microscope. The marrow sample test used the Bcr-Abl dual color probe and confirmed the Bcr-Abl translocation fusion product in 92% of cells.
Figure 5.

Fluorescent in-situ hybridization.
The final diagnosis was confirmed as bone marrow CML, with the presenting feature of the disease as unifocal extramedullary granulocytic sarcoma transformation. The blood and marrow met the criteria for chronic phase CML (ie, blasts < 10%, peripheral blood basophils < 20%, normal platelet count, no evidence of cytogenetic clonal evolution). However, the extramedullary myeloblast proliferation classifies the CML as blastic phase.
Discussion
Granulocytic sarcomas are rare, destructive, extramedullary tumor masses that consist of immature granulocytic cells. The term “chloroma” is derived from the Greek word chloros (for green). It describes the tumor's frequently greenish color, which is due to the presence and oxidation of the enzyme myeloperoxidase in the tumor. These tumors can arise de novo or can be associated with other myeloid disorders – acute myeloid leukemia (AML) or CML, myeloproliferative, or myelodysplastic conditions. Presentation can occur prior to, in association with the underlying myeloid disorder, or upon relapse. The location of the tumor varies – eg, subperiosteal bone – skull, pelvis, ribs, sternum; lymph node; skin; gums. In this case, the granulocytic sarcoma was a large destructive pelvic tumor that caused symptoms due to local destruction.
The WHO[1] has classified granulocytic sarcomas into 3 main types, depending upon the degree of maturation:
Blastic – composed mainly of myeloblasts
Immature – myeloblasts and promyelocytes
Differentiated – promyelocytes and more mature myeloid cells
Rarer types can consist of a monoblastic sarcoma, associated with monoblastic leukemia.
The diagnosis of granulocytic sarcoma can be difficult. As in this case, the disease is often not suspected on clinical grounds and a high index of suspicion is needed. Clinically and histologically, the diagnosis needs to be distinguished from the main differentials – ie, Hodgkin lymphoma, Burkitt's lymphoma, large cell lymphomas, and small round blue cell tumors, such as neuroectodermal tumors.
In this patient's case, the location and invasive nature of the tumor made an ovarian or metastatic tumor the most probable clinical diagnosis. Full investigations into the morphology, immunohistochemistry, immunophenotyping, and cytogenetics are essential as the diagnosis may be inconclusive on the basis of morphology alone. The morphology of the cells can be variable. If well differentiated, a diffuse infiltrate of granulocytic cells can be seen (often containing all stages of myeloid cell maturation). If poorly differentiated, the majority of the cells are a large and monotonous population. The nucleoli may or may not be prominent. Cytoplasm is often scanty. A high mitotic index can be seen [2] Dissection of collagen by strings of neoplastic cells is also a common feature. In lymph nodes, granulocytic sarcoma may show paracortical or sinus infiltration, or efface the architecture with a diffuse infiltrate. Bone marrow investigations need to be performed to look for any underlying myeloid conditions, as in this case. Tissue both from the tumor and the marrow needs to be examined as the cellularity and phenotype can differ between them.
Certain risk factors for developing granulocytic sarcomas associated with any underlying myeloid disorder have been recognized:
FAB types M2, M4, and M5 of the underlying leukemia
Expression of the surface markers CD 2, 7, and 56
Cytogenetic abnormalities t(8;21) and inv (16)[3]
Optimal therapy for these patients has not been well defined: standard AML chemotherapy is moderately effective and should be considered for all suitable cases. The addition of radiotherapy can provide a survival benefit, especially in CNS-related tumors. Chromosome abnormalities are associated with a worse prognosis. Intensive therapy should be considered early, especially for patients with chromosome 8 abnormalities.[4] Median survival is approximately 22 months, with worse outcomes more common in elderly patients.[5]
CML can be associated with granulocytic sarcomas in a variety of ways. Most frequently, the tumor presents later in the natural history of the CML as the disease progresses. Patients in relapse after chemotherapy or stem cell transplant can also present with a granulocytic sarcoma.[6] Of note, a granulocytic sarcoma that develops with chronic phase CML confers a worse prognosis – ie, a higher risk of rapid blastic marrow transformation.[7] Any underlying CML associated with the granulocytic sarcoma will require appropriate treatment, such as with imatinib mesylate. This targeted therapy inhibits the abnormal Bcr-Abl tyrosine kinase created by the Philadelphia chromosome abnormality. Imatinib inhibits cell growth and induces apoptosis in the affected cells, and should be used in combination with the standard AML therapy.
Readers are encouraged to respond to George Lundberg, MD, Editor of MedGenMed, for the editor's eye only or for possible publication via email: glundberg@medscape.net.
Figure 1a.




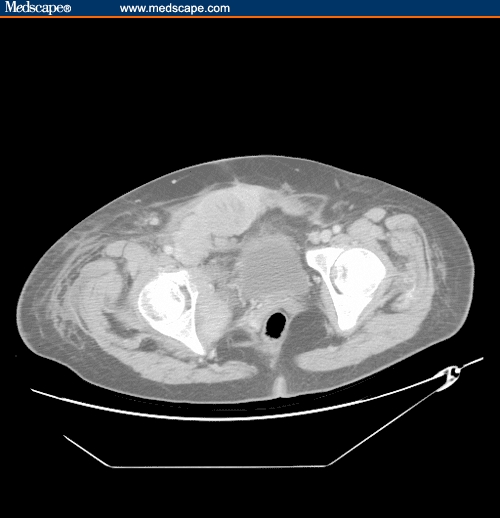
Anterior abdominal mass at the level of the bladder.
Figure 1b.





Mass at the level of the femoral heads.
Figure 1c.




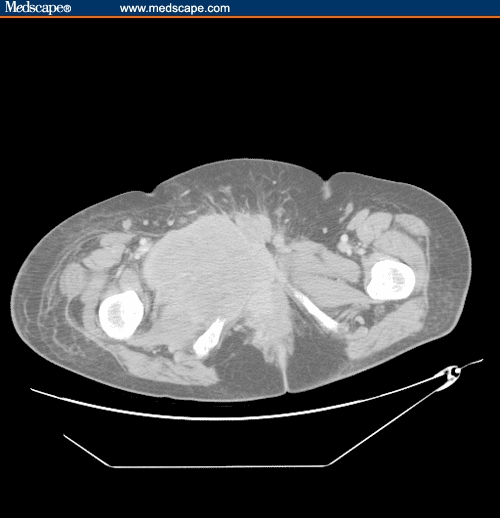
Central/right pelvic mass, crossing the midline, with involvement of the pelvic bones.
Figure 1d.





Upper right thigh.
Figure 1e.





Mass extending further down the thigh.
Figure 1f.





Mid right thigh region.
Contributor Information
Christopher I. Jenkins, Department of Haematology, University Hospital of Wales, Cardiff, United Kingdom.
Youssef Sorour, Department of Haematology, University Hospital of Wales, Cardiff, United Kingdom.
References
- 1.Jaffe ES, Harris NL, Stein H, Vardimann JW, editors. World Health Organisation Classification of Tumours – Tumours of Haematopoietic and Lymphoid Tissues. 2001. p. 105. [Google Scholar]
- 2.Bishop P. An immunohistochemical vade mecum. Available at www.e-immunohistochemistry.info. Accessed October 3, 2005.
- 3.Suzner T, Colakoglu N, Cirak B, Keskin A, Coskun E, Tahta K. Intracerebellar granulocytic sarcoma complicating acute myelogenous leukaemia: a case report and review of the literature. J Clin Neurosci. 2004;11:914–917. doi: 10.1016/j.jocn.2003.12.018. [DOI] [PubMed] [Google Scholar]
- 4.Tsimberidou A, Kantarjian H, Estey E, et al. Outcome in patients with nonleukaemic granulocytic sarcoma treated with chemotherapy with or without radiotherapy. Leukaemia. 2003;17:2011–2013. doi: 10.1038/sj.leu.2402958. [DOI] [PubMed] [Google Scholar]
- 5.Imrie K, Kovacs M, Selby D, et al. Isolated chloroma – the effects of early antileukaemic therapy. Ann Intern Med. 1995;123:351–353. doi: 10.7326/0003-4819-123-5-199509010-00005. [DOI] [PubMed] [Google Scholar]
- 6.Martel L, Reddy K, Greco M, Tuscano M, Richman M, Wun T. Isolated cavernous sinus extramedullary relapse of chronic myelogenous leukemia following allogeneic stem cell transplant. Ann Hematol. 2002;81:108–110. doi: 10.1007/s00277-001-0411-x. [DOI] [PubMed] [Google Scholar]
- 7.Mahendra P, Ager S, Bedlow AJ, Bloxham DM, Green AR, Marcus RE. Two unusual neurological presentations of granulocytic sarcoma in Philadelphia positive chronic myeloid leukaemia. Leuk Lymphoma. 1994;15:351–355. doi: 10.3109/10428199409049735. [DOI] [PubMed] [Google Scholar]


