Abstract
Stress urinary incontinence (SUI) is the most common form of urinary incontinence in women and is associated with high financial, social, and emotional costs. The history and physical examination can identify most patients with a significant stress incontinence component without the need for urodynamic testing. A variety of pharmacologic agents have been used off-label, but an evidence-based pharmacologic treatment has not been readily available. The development of a selective serotonin and norepinephrine reuptake inhibitor will add a potentially useful drug to the primary care physician's practice for treating female patients with SUI. In August 2004, a selective serotonin and norepinephrine reuptake inhibitor, duloxetine, became the first medication approved for the treatment of women with moderate to severe SUI throughout the European Union. As of November 2005, however, duloxetine has not been approved for the treatment of SUI in the United States.
Background
Stress urinary incontinence (SUI) is defined as involuntary leakage on exertion or on sneezing or coughing.[1] SUI affects approximately 13 million people in the United States alone and is much more prevalent in women than in men.[2] Overall, 30% of women will develop SUI within 5 years after their first vaginal delivery.[3] SUI is associated with significant social and financial costs. The social costs include personal embarrassment and curtailment of daily activities that may cause urine leakage. SUI is associated with depression, particularly in the elderly and in patients with an urge component.[4–6] The annual financial cost associated with urinary incontinence in the United States was estimated to be $16.3 billion in 1995.[7] The cost of incontinence pads and undergarments are borne directly by patients as they are usually not covered by health insurance plans.
Diagnosis
Table 1 lists the definitions of various forms of urinary incontinence.[1,2] SUI is the most common form of urinary incontinence, occurring in pure or mixed forms in nearly 80% of women with incontinence, according to 2 European studies.[8,9] Urge incontinence (UUI), or “overactive bladder,” is the second most common type of urinary incontinence. UUI is characterized by the unexpected loss of urine while suddenly feeling the need to urinate. Mixed urinary incontinence (MUI) is a term that applies to a combination of symptoms (SUI and UUI) and to a combination of urodynamic conditions (urodynamic stress incontinence and detrusor overactivity). Typically, women with MUI symptoms have more severe and bothersome incontinence than women with only SUI or UUI.[8,10] It has recently been proposed that these mixed symptoms are the result of, rather than the cause of, more severe SUI.[11,12] With urodynamic testing, MUI may be subclassified into more specific diagnoses.
Table 1.
| Stress | Involuntary leakage on effort or exertion, or on sneezing or coughing |
| Urge | Involuntary leakage accompanied by or immediately preceded by urgency |
| Mixed | Involuntary leakage associated with urgency and also with exertion, effort, sneezing, or coughing |
| Functional | Untimely urination because of physical disability, external obstacles, or problems in thinking or communicating that prevent a person from reaching a toilet |
| Overflow | Unexpected leakage of small amounts of urine because of an overfilled bladder |
| Transient | Leakage that occurs temporarily because of a condition or situation that will pass (eg, infection, medication) |
| Deformity | Fistula or developmental abnormality |
The 2005 International Consultation on Incontinence (ICI) developed a series of guidelines, including a clinical algorithm for the initial management of women with UI.[1] The ICI algorithm recommends that the assessment include a targeted medical history and assessment of quality of life, a general assessment, and a focused physical examination before arriving at a presumed diagnosis and initiating treatment. The need to simplify this algorithm has been addressed.[13]
A patient history should include consideration of the underlying risk factors listed in Table 2, as well as potentially reversible causes described in Table 3.[14] In practical experience, in the primary care setting, a history based on eliciting underlying risk factors, reversible causes, and the symptoms listed in Table 1 will help identify patients with SUI or UUI. In the case of patients with mixed symptoms, it may be necessary to clarify the source of the symptoms. Asking the patient to keep a bladder record such as the one available for download from the National Library of Medicine at http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat6.table.32903 can help clarify symptoms.[15]
Table 2.
Risk Factors for Urinary Incontinence[8]
| Estrogen depletion | |||||||||||
| Diabetes | |||||||||||
| Childhood nocturnal enuresis | |||||||||||
| Morbid obesity | |||||||||||
| Race | |||||||||||
| Smoking | |||||||||||
| Fecal impaction | |||||||||||
| Delirium | |||||||||||
| Low fluid intake | |||||||||||
| High-impact physical activities | |||||||||||
| Environmental barriers | |||||||||||
| Stroke or impaired cognition | |||||||||||
| Immobility/chronic degenerative disease | |||||||||||
| Pelvic muscle weakness | |||||||||||
| Pregnancy/vaginal delivery/episiotomy | |||||||||||
| Medications: | Diuretics | Caffeine | Alcohol | Beta-adrenergic agonists | Alpha-adrenergic agonists | Alpha-adrenergic blockers | Narcotic analgesics | Anticholinergic agents | Calcium channel blockers | Psychotropics | Angiotensin converting enzyme inhibitors |
Table 3.
Management of Reversible Conditions That Cause or Contribute to Urinary Incontinence[7]
| Condition | Management |
|---|---|
| Urinary tract infection | Antimicrobial therapy |
| Atrophic vaginitis/urethritis | Oral or topical estrogen |
| Pregnancy/vaginal delivery | Behavioral intervention (Avoid surgical therapy postpartum, as condition may be self-limiting.) |
| Stool impaction | Disimpaction – stool softeners, bulk-forming agents, and laxatives, if necessary; high fiber intake, adequate mobility and fluid intake |
| Medications (see Table 2) | Discontinue or change therapy, reduce dosages; modify diuretic schedule. |
| Metabolic disorder (hyperglycemia, hypercalcemia) | Better control of diabetes mellitus (Therapy for hypercalcemia depends on underlying cause.) |
| Excess fluid intake | Reduction in intake of diuretic fluids (eg, caffeinated beverages) |
| Venous insufficiency with edema | Support stocking, leg elevation, sodium restriction, diuretic therapy |
| Congestive heart failure | Medical therapy |
| Delirium | Diagnosis and treatment of underlying cause(s) of acute confusional state |
| Illness, injury, or restraint that interferes with mobility | Regular toileting, environmental alterations (eg, bedside commode, urinal) |
| Psychological | Removal of restraints if possible; appropriate pharmacological and/or nonpharmacologic treatment |
A focused physical examination is described in Table 4. A urinalysis should be performed on all patients with incontinence to rule out pyuria (infection), hematuria (infection, stones, or cancer), proteinuria (renal disease), and glycosuria (diabetes).
Table 4.
Focused Physical Examination in the Patient With Urinary Incontinence
|
A stress pad test – either a short-term test conducted in the office or a long-term test conducted at home – is also useful as an optional investigative tool. The test measures the amount of leakage that occurs when the patient performs a series of activities that might trigger urine leakage (eg, jumping, climbing stairs, coughing vigorously, performing deep knee bends, or washing hands). A pad weight gain ≥ 1 g is considered positive for the 1-hour test, whereas a weight gain ≥ 4 g is considered positive for the 24-hour test.[16] Controversy exists about the reproducibility and validity of these tests, and the 1-hour test is not very accurate unless a fixed bladder volume is confirmed via catheterization or ultrasound.[16]
The results of the history, physical examination for stress-induced leakage, and bladder catheterization for postvoid residual urine volume will identify the majority of patients with SUI or MUI and distinguish them from those with primarily overactive bladder. Those who can be assumed to have SUI or MUI will have a history of leaking with coughing or straining, will demonstrate leakage when asked to cough or “bear down” during the physical examination, will have a postvoid residual urine volume of < 50 to 100 mL, and will have a normal urinalysis. Bladder catheterization is no longer recommended as an obligatory assessment for all women. However, it should be considered in women with neurologic disease, severe pelvic organ prolapse, or a history of prior incontinence surgery or radical pelvic surgery. Although specialized urodynamic testing can be performed to more precisely differentiate between SUI and UUI, the results of such testing have indicated that a high percentage of those with MUI symptoms are classified in the stress category rather than the urge category.[17] It is therefore reasonable to consider initiating treatment for SUI in any patient with significant symptoms of SUI without performing urodynamic testing.
Treatment
If the history and physical exam identify an underlying cause such as urinary tract infection or fecal impaction, the patient should be treated accordingly and followed up to determine whether symptoms have resolved. If medications result in intolerable side effects, substitutions can be made or dosages reduced, if possible. A trial of topical estrogen may be of benefit for younger postpartum women or for peri- and postmenopausal women who may be estrogen deficient.
After underlying causes are ruled out or treated, most women with incontinence will have symptoms suggesting the stress or the mixed type. Management falls into these general categories:
Behavioral
Mechanical
Pharmacologic
Surgical
Behavioral therapy includes bladder retraining and biofeedback, particularly for those with overactive bladder. Pelvic floor muscle exercises (Kegel exercises) are used to rehabilitate and strengthen the pelvic floor muscles and promote urine storage. Compliance is often poor, but results have been favorable for motivated patients who receive proper clinical training and assessment and who repeat contractions several times a day for at least 3 months.[18,19] Patients must be properly instructed in Kegel exercises. Some patients incorrectly perform a “bearing down” effort, which will actually make their SUI worse. Perhaps the most effective way to instruct a woman in the proper performance of pelvic floor exercise is during the physical examination. The examiner's fingers are placed within the vagina and the patient is asked to squeeze the pelvic muscles around them as if trying to hold back urine or stool. This squeeze should be held for about 10 seconds, then released for 10 seconds. The woman should be asked to perform the same type of squeeze at home 10 times in a row, 3 to 4 times per day. Patient instructions for performing Kegel exercises are available for download from the American Academy of Family Physicians (AAFP) at http://familydoctor.org/handouts/642.html.[20]
Nonsurgical mechanical treatments include pessaries to elevate the vesico-urethral angle, urethral occlusive devices, and use of weighted vaginal cones to provide sensory feedback during pelvic floor muscle exercise. Although these devices have demonstrated efficacy and tolerability in clinical studies, patient acceptance has not been sufficient for commercial success. The lack of acceptance has been associated with difficulties in inserting and removing these devices, physical discomfort, and cost.[19]
Anticholinergics and alpha-adrenergics have been suggested for off-label treatment of SUI (Table 5). An anticholinergic effect on the smooth muscle of the urethra has not been documented, however. In addition, alpha-adrenergic agents such as pseudoephedrine and tricyclic agents such as imipramine do not constitute effective treatment for most SUI patients.[21]
Table 5.
Pharmacologic Therapy for Urinary Incontinence in Women
| Class of Agent | Specific Agent | Condition |
|---|---|---|
| Topical or vaginal estrogen | Conjugated estrogen | Vaginal atrophy |
| Anticholinergic agents | Tolterodine | Urge incontinence (overactive bladder) |
| Oxybutynin | ||
| Propantheline | ||
| Darifenacin | ||
| Solifenacin | ||
| Tricyclic antidepressants | Imipramine* | Mixed and stress urinary incontinence |
| Alpha-adrenergic agonists | Pseudoephedrine* | Stress urinary incontinence |
| Selective serotonin and norepinephrine reuptake inhibitor | Duloxetine† | Stress urinary incontinence |
Off-label usage
Approved for treating SUI in the European Union but not in the United States
An understanding of the physiology of bladder filling, emptying, and control under stress suggests that unlike anticholinergics, selective inhibition of serotonin and norepinephrine reuptake can help control SUI.[22] This physiology is illustrated in Figures 1 and 2.
Figure 1.

The physiology of bladder filling and of the guarding reflex.
Figure 2.
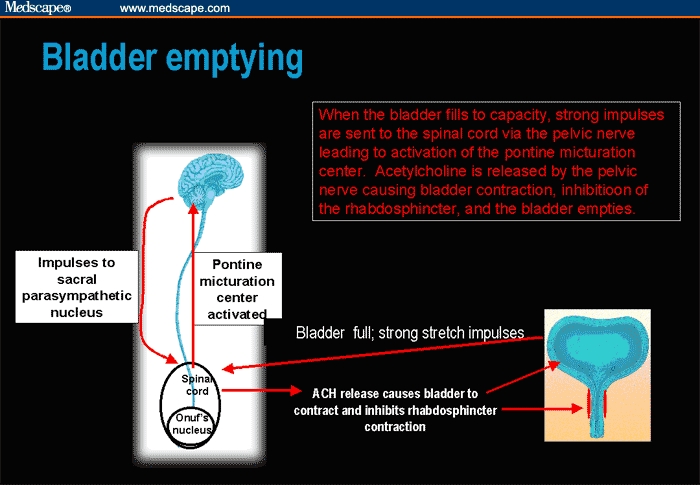
The physiology of bladder emptying.
Recently, a new selective serotonin and norepinephrine reuptake inhibitor, duloxetine, has demonstrated efficacy in phase 2 and phase 3 trials[23–26] and has been approved throughout the European Union for the treatment of SUI. As of November 2005, duloxetine has not been approved for use in the treatment of SUI in the United States. The mechanism of action of this new agent is presumed to be via Onuf's nucleus in the sacral spinal cord.[24] Pudendal motor neurons located in Onuf's nucleus regulate the urethral striated muscle sphincter, and Onuf's nucleus has a high density of norepinephrine and serotonin receptors. Norephinephrine and serotonin stimulate these neurons, causing an increase in the strength of urethral sphincter contractions. Duloxetine blocks the reuptake of norepinephrine and serotonin, increasing pudendal nerve activity and sphincter muscle tone.[27]
In an integrated analysis of 4 randomized, controlled, clinical trials including 1913 women with SUI, duloxetine significantly decreased the median incontinence episode frequency by 51.5%, compared with a 33.3% reduction in the placebo group.[28] Among the patients taking duloxetine, those with more severe symptoms experienced greater benefit. The main adverse event, which led to a discontinuation rate of 5% among 958 patients taking the 40- to 80-mg dose, was nausea; the placebo discontinuation rate among 955 patients was 0.3%.[29]
If behavioral and pharmacologic treatments fail, surgical therapy is possible.[30] Some of the most common surgical options are listed in Table 6.
Table 6.
Surgical Options for Treatment of Urinary Incontinence
| Retropubic urethropexies (Burch and Marshall-Marchetti-Krantz procedures) |
| Suburethral sling (“tension-free vaginal tape”) |
| Periurethral injection of bovine collagen or carbon-coated beads |
Despite its frequency and potential significant impact on quality of life, patients often under-report SUI. They may be embarrassed, they may consider incontinence a normal part of aging, they may fear surgery, or they may not know about medical management options.[31] For these reasons, it is important for physicians to inquire about incontinence. A downloadable patient information resource is available from AAFP at http://familydoctor.org/healthfacts/189/.[32]
Summary
SUI is the most common type of urinary incontinence in women. In most cases, the history and physical examination can identify patients with a significant stress component without the need for urodynamic testing. Currently, treatment for SUI in the United States is limited to various types of behavioral interventions, mechanical devices, and surgery; however, pharmacologic treatment options are being investigated and becoming more widely available throughout the European Union and several other countries.
Acknowledgments
Assistance for this manuscript was provided by Eli Lilly and Company. The author would like to thank Meghan Wulster-Radcliffe of Eli Lilly and Company for her writing, editing, and formatting support for this manuscript.
Contributor Information
Mark Deutchman, Department of Family Medicine, University of Colorado Health Sciences Center at Fitzsimons, Aurora. Email: mark.deutchman@uchsc.edu.
Meghan Wulster-Radcliffe, Eli Lilly and Company, Indianopolis, Indiana.
References
- 1.Abrams P, Andersson K, Brubaker LT, Cardozo L, Cottenden A, Denis L. Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and faecal incontinence. In: Abrams P, Cardozo L, Khoury S, Wein A, editors. 3rd International Consultation on Incontinence. Plymouth, UK: Health Publication Ltd; 2005. –1589.pp. 1630 [Google Scholar]
- 2.Urinary Incontinence in Women. Bethesda, Md: National Kidney and Urologic Diseases Clearinghouse; NIH Publication No. 02-4132, May 2002. Available from: http://kidney.niddk.nih.gov/kudiseases/pubs/uiwomen/index.htm. Accessed November 9, 2005. [Google Scholar]
- 3.Viktrup L, Lose G. The risk of stress incontinence 5 years after first delivery. Am J Obstet Gynecol. 2001;185:82–87. doi: 10.1067/mob.2001.114501. [DOI] [PubMed] [Google Scholar]
- 4.Dugan E, Cohen S, Bland DR, et al. The association of depressive symptoms and urinary incontinence among older adults. J Am Geriatr Soc. 2000;48:413–416. doi: 10.1111/j.1532-5415.2000.tb04699.x. [DOI] [PubMed] [Google Scholar]
- 5.Melville JL, Walker E, Katon W, Lentz G, Miller J, Fenner D. Prevalence of comorbid psychiatric illness and its impact on symptom perception, quality of life, and functional status in women with urinary incontinence. Am J Obstet Gynecol. 2002;187:80–87. doi: 10.1067/mob.2002.124839. [DOI] [PubMed] [Google Scholar]
- 6.Viktrup L, Koke S, Burgio KL, Ouslander JG. Stress urinary incontinence in active elderly women. South Med J. 2005;98:79–89. doi: 10.1097/01.SMJ.0000146587.06656.98. [DOI] [PubMed] [Google Scholar]
- 7.Wilson L, Brown JS, Shin GP, Luc KO, Subak LL. Annual direct cost of urinary incontinence. Obstet Gynecol. 2001;98:398–406. doi: 10.1016/s0029-7844(01)01464-8. [DOI] [PubMed] [Google Scholar]
- 8.Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: The Norwegian EPINCONT study. J Clin Epidemiol. 2000;53:1150–1157. doi: 10.1016/s0895-4356(00)00232-8. [DOI] [PubMed] [Google Scholar]
- 9.Hunskaar S, Lose G, Sykes D, Voss S. The prevalence of urinary incontinence in women in four European countries. BJU Int. 2004;93:324–330. doi: 10.1111/j.1464-410x.2003.04609.x. [DOI] [PubMed] [Google Scholar]
- 10.Sandvik H, Hunskaar S, Vanvik A, Bratt H, Seim A, Hermstad R. Diagnostic classification of female urinary incontinence: an epidemiological survey corrected for validity. J Clin Epidemiol. 1995;48:339–343. doi: 10.1016/0895-4356(94)00147-i. [DOI] [PubMed] [Google Scholar]
- 11.Bump RC, Norton PA, Zinner NR, Yalcin I. Mixed urinary incontinence in women with predominant stress urinary incontinence symptoms: urodynamic findings, incontinence severity measures, and duloxetine treatment response. Obstet Gynecol. 2003;102:76–83. doi: 10.1016/s0029-7844(03)00376-4. [DOI] [PubMed] [Google Scholar]
- 12.Bump R, Norton P, Dmochowski R, Zinner N, Wulster-Radcliffe M, Yalcin I. Pure stress urinary incontinence symptoms and stress-predominant mixed urinary symptoms: comparing symptom severity and response to treatment with duloxetine. BJU Intl. Accepted for publication. [Google Scholar]
- 13.Viktrup L. Addressing the need for a simpler algorithm for the management of women with urinary incontinence. Medscape General Medicine. 2005;7:3. Available at: http://www.medscape.com/viewarticle/506898. Accessed November 9, 2005. [PMC free article] [PubMed] [Google Scholar]
- 14.National Library of Medicine. Urinary Incontinence in Adults: Acute and Chronic Management. Clinical Practice Guideline Number 2 (1996 Update) AHCPR Publication No. 96-0682: March 1996. Available at: http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat6.chapter.9995. Accessed November 9, 2005.
- 15.National Library of Medicine. Sample bladder record. Available at: http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat6.table.32903. Accessed November 9, 2005.
- 16.Artibani W, Andersen JT, Gajewski JB, et al. Abrams P, Cardozo L, Khoury S, Wein A. Incontinence. 2nd ed. Plymouth, UK: Health Publication Ltd.; 2002. Imaging and other investigations; pp. 425–477. [Google Scholar]
- 17.Weidner AC, Myers ER, Visco AG, Cubdiff GW, Bump RC. Which women with stress incontinence require urodynamic evaluation? Am J Obstet Gynecol. 2001;184:20–27. doi: 10.1067/mob.2001.108171. [DOI] [PubMed] [Google Scholar]
- 18.Diokno AC, Burgio K, Fultz NH, Kinchen KS, Obenchain R, Bump RC. Medical and self-care practices reported by women with urinary incontinence. Am J Manag Care. 2004;10(2 Pt 1):69–78. [PubMed] [Google Scholar]
- 19.Wilson PD, Bø K, Hay-Smith J, et al. Abrams P, Cardozo L, Khoury S, Wein A. Incontinence. 2nd ed. Plymouth, UK: Health Publication Ltd; 2002. Conservative treatment in women; pp. 571–624. [Google Scholar]
- 20.American Academy of Family Physicians. Urinary Incontinence: Kegel Exercises for your Pelvic Muscles. Information from your Family Doctor. Available at: http://familydoctor.org/handouts/642.html. Accessed November 9, 2005. [Google Scholar]
- 21.Kershen RT, Hsieh M. Preview of new drugs for overactive bladder and incontinence: darifenacin, solifenacin, trospium, and duloxetine. Curr Urol Rep. 2004;5:359–367. doi: 10.1007/s11934-004-0083-x. [DOI] [PubMed] [Google Scholar]
- 22.Morrison J, Steers WD, Brading A, et al. Neurophysiology and neuropharmacology. In: Abrams P, Khoury S, Wein A, editors. Incontinence. 2nd ed. Plymouth, UK: Health Publication Ltd; 2002. pp. 83–163. [Google Scholar]
- 23.Norton PA, Zinner NR, Yalcin I, Bump RC. Duloxetine versus placebo in the treatment of stress urinary incontinence. Am J Obstet Gynecol. 2002;187:40–48. doi: 10.1067/mob.2002.124840. [DOI] [PubMed] [Google Scholar]
- 24.Dmochowski RR, Miklos JR, Norton PA, Zinner NR, Yalcin I, Bump RC. Duloxetine versus placebo for the treatment of North American women with stress urinary incontinence. J Urol. 2003;170:1259–1263. doi: 10.1097/01.ju.0000080708.87092.cc. [DOI] [PubMed] [Google Scholar]
- 25.van Kerrebroeck P, Abrams P, Lange R, et al. Duloxetine versus placebo in the treatment of European and Canadian women with stress urinary incontinence. BJOG. 2004;111:249–257. doi: 10.1111/j.1471-0528.2004.00067.x. [DOI] [PubMed] [Google Scholar]
- 26.Millard RJ, Moore K, Rencken R, Yalcin I, Bump RC. Duloxetine vs placebo in the treatment of stress urinary incontinence: a four-continent randomized clinical trial. BJU Int. 2004;93:311–318. doi: 10.1111/j.1464-410x.2004.04607.x. [DOI] [PubMed] [Google Scholar]
- 27.Thor KB. Exploring new horizons in neurourology. Contemp Urol. 2002;(Suppl):9–13. Sept. [Google Scholar]
- 28.Bump RC, Wulster-Radcliffe MC, Hooper C, Yalcin I. Duloxetine versus placebo for the treatment of women with stress urinary incontinence: an integrated efficacy analysis of four randomized controlled trials. BJOG. 2005 Accepted for publication. [Google Scholar]
- 29.Hurley D, Turner CL, Yalcin I, Viktrup L, Baygani SK. Duloxetine for the treatment of stress urinary incontinence in women: an integrated analysis of safety. Eur J Obstet Gynecol Reprod Biol. 2005 doi: 10.1016/j.ejogrb.2005.08.006. (epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 30.Hilton P. Trials of surgery for stress incontinence – thoughts on the ‘Humpty Dumpty principle’. BJOG. 2002;109:1081–1088. doi: 10.1111/j.1471-0528.2002.02011.x. [DOI] [PubMed] [Google Scholar]
- 31.Dugan E, Roberts CP, Cohen SJ, et al. Why older community-dwelling adults do not discuss urinary incontinence with their primary care physicians. J Am Geriatr Soc. 2001;49:462–465. doi: 10.1046/j.1532-5415.2001.49094.x. [DOI] [PubMed] [Google Scholar]
- 32.American Academy of Family Physicians. Family Health Facts. Urinary Incontinence: Embarrassing but Treatable. Available at: http://familydoctor.org/healthfacts/189/. Accessed November 9, 2005. [Google Scholar]


