Abstract
Obesity is no longer just a “Western” problem, as evidenced by an increase in prevalence of up to 75% in parts of the developing world. It is important to transfer experience from the developed world to developing countries in an attempt to prepare for the inevitable health and economic problems. This case report highlights an unusual intraoperative complication that has medical and medico-legal implications. A simple apparatus designed to retract the panniculus of an obese patient might reduce complications when performing abdominal surgery in such cases.
Synopsis
Surgery in the morbidly obese is associated with risk. Correct handling of an abdominal panniculus is an important issue.
Introduction
The World Health Organization suggests that a prevalence of 15% or greater for a disease represents an epidemic.[1] Worldwide, the prevalence of obesity has now exceeded this mark[2,3] and warrants urgent attention and intervention if we are to avoid the significant impact that obesity has on physical, mental, and social ill health and its economic burdens.[4]
Although it is important to initiate politically driven public health measures to curb this epidemic in the long term, for the present, we shall have to devise procedural technologies that will minimize any iatrogenic injury that may affect obese patients.
The increase in obesity in younger women is of particular concern to obstetricians because of the increased incidence of associated medical and surgical risks during pregnancy, labor, and delivery. This case report describes an unusual complication of cesarean section in a morbidly obese woman that stimulated the development of a simple apparatus to minimize such complications. One of the authors (OACV) encountered the case described below while in practice at the Hamilton Base Hospital in the Western District of Victoria, Australia.
Case Report
MB, a 34-year-old G3 P2 booked for confinement under the care of a local GP obstetrician. She was a heavy smoker and morbidly obese. She weighed 148 kg and was 1.65 m tall (body mass index = 54). Serial antenatal ultrasound examinations (palpation was unhelpful) revealed normal fetal position and presentation and adequate intrauterine growth. She remained normotensive throughout her pregnancy.
Despite reliable menstrual data, an early ultrasound examination was necessary to determine gestational age as bimanual examination of the pelvis was unhelpful at estimating uterine size in the first trimester. Labor was induced by amniotomy and intravenous oxytocin when she was 9 days post-date. Cervical dilation was recorded as 2 cm with a modified Bishop score of 6. Intravenous oxytocin was administered as per labor ward protocol. The patient was in established labor 6 hours after induction by midday and had only achieved a cervical dilation of 5 cm 12 hours after amniotomy. Thick meconium-stained liquor was noted at midnight, and a repeat vaginal examination at this time revealed an arrest of labor at 5 cm. An urgent referral for consultant (OACV) opinion was sought. Vaginal exam by the consultant obstetrician was difficult. Morbid obesity made access to the perineum difficult, and a digital exam was only possible after much effort. Thick meconium staining of the liquor was confirmed and cord prolapse excluded. The presenting fetal head was high, suggesting a brow presentation. A decision was made to perform an emergency cesarean section. Although regional anesthesia would have been preferred, general anesthesia was administered for 2 reasons. First, poor fetal condition necessitated urgent delivery and, second, morbid obesity obscuring the intervertebral spaces made the administration of a spinal block more difficult.
The main intraoperative problem encountered was a large panniculus of anterior abdominal wall fat that extended to approximately 20 cm below the mons veneris. A medical student was recruited to retract this panniculus as the GP obstetrician was to attend to the newborn. Delivery of the infant was achieved via a low Pffannensteil skin incision and was reasonably uncomplicated apart from limited exposure. Brow presentation was confirmed, and there were no cord or placental complications to account for the intrapartum fetal distress. A male infant weighing 3.915 kg was delivered with birth Apgar scores of 7 and 9 at 1 and 5 minutes, respectively. Duration of surgery was 1 hour, and the estimated blood loss was 500 mL.
Postoperative thromboprophylaxis was continued, and the patient was discharged with her newborn baby to the hospital in the home system 48 hours after delivery. Skin sutures were removed on the 8th postoperative day and wound union was excellent. However, on the 11th postoperative day, it became clear that the patient had developed decubitus ulcers caused by pressure of the thumbs and digits of the medical student during retraction of the panniculus (Figure 1). Full thickness sloughing ensued at these points, requiring intensive wound care for10 weeks before complete healing. The patient was informed of the iatrogenic nature of the “injury” but accepted this outcome given the adverse circumstances surrounding the delivery.
Figure 1.
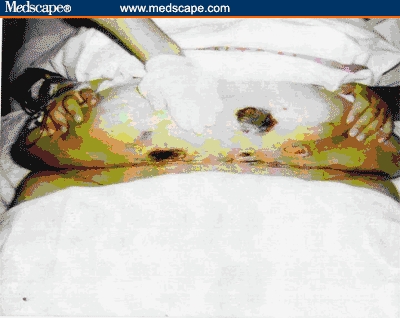
Day 11 post operation. Necrosis from forefinger pressure on inferior surface of panniculus. Thumb pressure points of necrosis were visible on the superior aspect. The scar itself is well healed.
Discussion
This case report highlights an unusual surgical complication that has not only medical considerations but also the potential for litigation. Obesity, its associated health problems, their economic implications, and the urgent need to tackle the problem effectively are all well recognized but will need time for change. Withdrawal of medical help in such cases, as advocated by Longmore in Australia,[5] is unhelpful. Instead, we should seek ways of trying to minimize possible complications. Reporting such problems is essential to create awareness within the specialty.
Cephalad retraction of the panniculus in morbidly obese patients during cesarean section carries the risk of hypotension and fetal compromise as well as respiratory difficulties, especially in the patient with a regional block. Therefore, this retraction must be done with great care and concern.
Figure 2 shows a simple device devised by the surgical staff at Hamilton Base Hospital to assist in cephalad retraction of the panniculus. It consists of:
Hooks to attach chain to railing across the operating table
Chain to provide adjustable length
Large Doyen's retractor to contain the edge of the panniculus
Figure 2.
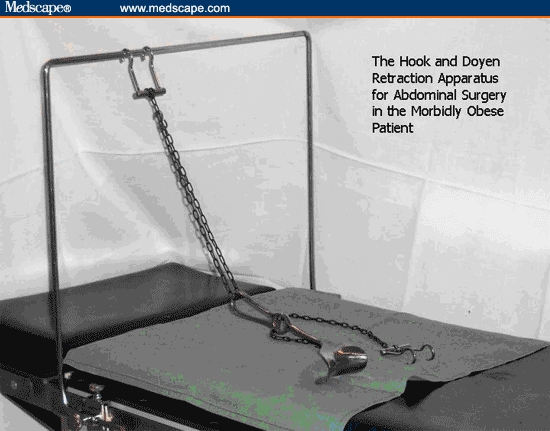
Simple apparatus incorporating a Doyen's retractor and hooks to be applied to the inferior border of the panniculus. Shortening the chain applies the necessary amount of traction for appropriate retraction of the panniculus.
We have found this method of retracting the panniculus simple, effective, and more convenient than the alternatives. The use of broad zinc oxide sticky tape to “hitch up” the panniculus, for example, carries a small risk of allergy and may itself cause skin trauma on removal. The use of Kocher's forceps to retract the superior edge of the incision requires the assistance of the anesthetist, who may have a host of other concerns during the procedure. This apparatus can be sterilized and allows for adjustment by the surgeon during the procedure. The edge of the panniculus is contained in the large Doyen retractor, which in turn is connected to a chain whose length can be adjusted as necessary. To date, we have not experienced any ischemic damage using this gadget to retract the panniculus and so suggest that those involved in surgery of the morbidly obese individual consider its use as a simple low-cost device.
Contributor Information
Claire Maria Viegas, Department of Family Medicine, School of Medicine, Universiti Malaysia Sabah, Malaysia. Email: profviegas@yahoo.com.au.
Osborn A C Viegas, Department of Reproductive Health, School of Medicine, Universiti Malaysia Sabah, Malaysia.
References
- 1.World Health Organization, Food and Agriculture Organization. Report of the joint WHO/FAO expert consultation on diet, nutrition and the prevention of chronic diseases. Geneva, Switzerland: WHO Tech Report 916, 2003. [PubMed]
- 2.White C. Obesity rates treble in England. BMJ. 2001;322:450. [Google Scholar]
- 3.Vlad I. Obesity costs UK economy 2bn pounds sterling a year. BMJ. 2003;327:1308. doi: 10.1136/bmj.327.7427.1308-d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ganapati M. Asia grapples with obesity epidemics. BMJ. 2003;326:515. doi: 10.1136/bmj.326.7388.515/a. Vlad I. Obesity costs UK economy 2bn pounds sterling a year. BMJ. 2003;327:1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Australian Associated Press. Pregnant woman ‘too fat’ for hospital. June 13, 2005.


