Abstract
Purpose: To assess feasibility, results and complications in image-guided biopsies using a single needle design in various organs. Materials and methods: 100 consecutive percutaneous biopsies were performed in 54 females and 46 males aged 24–87 years (mean age/standard deviation: 64.5 +/− 12 years) using a full-core end-cut tri-axial full-automatic biopsy needle (18 gauge BioPince ™, InterV-MDTech, Gainesville, Florida) under CT (n=45) or ultrasound (n=55) guidance. In 63 biopsies a coaxial technique was used. Results: Biopsies were obtained of liver (n=32), lymph nodes (n=17), thyroid (n=11), lung (n=9), adrenal (n=9), pelvis (n=6), chest wall/pleura (n=6), mediastinum (n=4), lytic bone lesions (n=2), retroperitoneum (n=1), muscle (n=1), pancreas (n=1), peritoneum (n=1). Between 1 and 6 (mean/SD 2.83 +/− 0.92) needle passes were performed. In 77 cases a malignant (40 metastases, 37 primary tumours) and in 23 a benign lesion was diagnosed. Of the 23 benign lesions a specific diagnosis was possible in 22. In one case necrosis and haemorrhage was diagnosed. In this patient surgery and autopsy both revealed a mediastinal haematoma of unknown origin. Eight minor complications (mild pain/local haematoma requiring no therapy) and three major complications (three pneumothoraces in nine lung biopsies requiring two aspirations and one drainage) were observed. There was no mortality. Conclusion: Percutaneous image-guided biopsy using the described full-core end-cut needle resulted in a specific diagnosis in 99/100 consecutive biopsies in various organs with a low complication rate. We use this needle type for all CT- or US-guided biopsies in all organs except for solid bone.
Keywords: Biopsy, CT-fluoroscopy, ultrasonography, core biopsy
Introduction
For percutaneous biopsy different needle types are available. Simple bevel shapes are used for fine needle aspiration (FNA) providing material for cytological analysis. Cutting or core biopsy needles provide specimens that preserve the tissue architecture enabling histological analysis. Design of these needles is complex with considerable differences between needle types resulting in different advantages and disadvantages. Two needle designs are most commonly used:
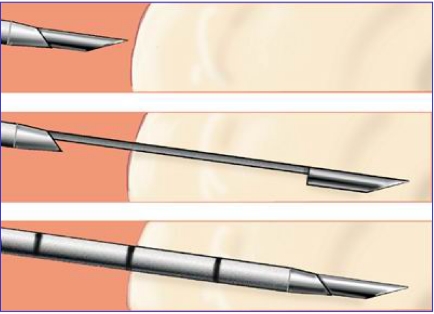
The first type consists of an inner stylet with a side notch and an outer cutting needle. It is introduced with the stylet slightly protruding from the cutting needle. After positioning of the needle tip at the margin of the lesion the stylet is further advanced into the lesion followed by subsequent advancement of the cutting needle over the stylet. Tissue protruding into the side notch is cut off by advancement of the cutting needle and entrapped. Thus, it cannot be lost during withdrawal of the needle (Fig. 1). However, this technique, obviously results in relatively little tissue being obtained as only the lumen of the notch is used to retrieve tissue. Furthermore, compression of tissue by advancement of the stylet may result in crush artifacts compromising histological assessment, again requiring more tissue for a correct diagnosis. The side-notch needle type is also called the ‘tru-cut’ type after the first model commercially used (Tru-Cut ™, Allegiance, USA). Side-notch core needles can be advanced manually or spring driven, the latter having either plastic handles for single use or metal handles which can be re-sterilized and loaded with single-use needles. Automatic spring driven needles provide more tissue than manually advanced needles of the same type [1]. Automatic tru-cut type needles are marketed under various names by different manufacturers.
Figure 1.
Designs of side-notch needle (‘tru-cut’-type).
The second needle type most commonly used is composed of a sharp inner stylet and an outer cutting needle. It is introduced in a similar fashion to the type described above. At the margin of the lesion the stylet is removed and a vacuum applied during advancement of the cutting needle. Thus, a core specimen is cut from the target tissue using the entire lumen of the cutting needle. However, as the needle tip remains open the specimen may be lost when the needle is removed. This needle type is mostly advanced manually. Its results have been shown to be inferior to those of automatic tru-cut type needles [2].
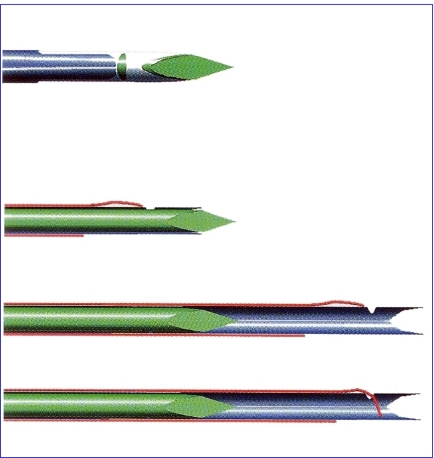
The novel design of the core needle used in this study (BioPince ™ needle) is based on three separate parts (tri-axial design): a sharp inner stylet, an outer cutting needle and an outermost pincer needle. For biopsy the needle is advanced with the stylet slightly protruding from both the cutting and the pincer needle. At the margin of the lesion the cutting needle is advanced over the stylet, cutting through tissue without compressing it, followed by the pincer needle which slides over the cutting needle and cuts off the core of tissue at the needle tip (end-cut design); it also seals the tip of the cutting needle. Thus the specimen cannot be lost at withdrawal of the needle (Fig. 2).
Figure 2.
Designs of tri-axial, end-cut needle (BioPince ™ needle).
The stroke length is set after loading the spring prior to introduction of the needle by manually setting a plastic stopper to the desired depth of 13, 23 or 33 mm as indicated on the handle.
In side-notch needles the actual length of the side notch (i.e. specimen) is shorter than the advancement of the stylet and cutting needle. Also, only part of the needle lumen—the volume of the notch—is used to store tissue.
In the tri-axial end-cut needle, in contrast, the entire lumen and almost the whole length of advancement of the needle within the lesion is used to enclose the specimen. Therefore, this needle can provide longer cores resulting in up to 30% more tissue as compared to side-notch needles when using the same diameter of needle and depth of introduction [3].
In preliminary applications we found the visibility of the tri-axial needle to be excellent at both ultrasound and CT.
Because of its specific design, its good visibility at both of the imaging modalities commonly used for biopsy guidance and the fact that the same model of tri-axial needle allows stroke lengths of 13, 23, and 33 mm we felt that this needle would be appropriate as the only needle type used for soft tissue biopsy in all types of organs in both ultrasound- and CT-guided biopsies. Thus we hoped to avoid the use of different needle types in different situations and therefore facilitate needle handling during biopsies and storage.
At the time of initiation of this study the BioPince ™ needle was only available with a diameter of 18 gauge and with total lengths of 10, 15, and 20 cm. For each length an appropriate guiding needle (16 gauge) is available for coaxial biopsies with lengths of 6.8 cm, 11.8 cm, and 16.8 cm, respectively (Fig. 3).
Figure 3.
18 gauge BioPince ™ needle with 16 gauge guiding needle for coaxial biopsies.
The aim of our study was to assess the feasibility, diagnostic accuracy and complication rate of biopsies of different organs guided by different imaging modalities using exclusively the tri-axial end-cut needle.
Patients and methods
We analysed 100 consecutive biopsies referred to our department for percutaneous biopsies of organs other than solid bone from September 2002 through February 2004. Patient age ranged from 24 to 87 years with a median age of 64.5 +/− 12 years (standard deviation). In 54 biopsies the patients were females and in 46 males. Ninety-three procedures were performed in in-patients and seven in out-patients.
Patients were referred for biopsy for different reasons (Table 1). Most commonly, biopsy was performed to confirm or exclude malignancy of newly detected focal lesions or to determine whether focal lesions represented metastases in a patient with known malignancy.
Table 1.
Indications for percutaneous biopsy
| Focal lesion, no known malignancy | 60 | |
| Known malignancy | 40 | |
| One known primary: confirm/exclude metastasis | 30 | |
| Two known primaries: classify presumable metastasis | 8 | |
| Three known primaries: classify presumable metastasis | 1 | |
| Four known primaries: classify presumable metastasis | 1 | |
| Total | 100 | |
Biopsies were obtained in 13 different organs, most commonly the liver (n=32) (Table 2).
Table 2.
Organ, imaging technique for guidance and biopsy technique
| Organ | Total | CT guidance | US guidance |
|---|---|---|---|
| (coaxial/direct) | (coaxial/direct) | (coaxial/direct) | |
| Liver | 32 (21/11) | 4 (3/1) | 28 (18/10) |
| Lymph nodes | 17 (12/5) | 12 (10/2) | 5 (2/3) |
| Thyroid | 11 (0/11) | 0 | 11 (0/11) |
| Lung | 9 (5/4) | 9 (5/4) | 0 |
| Adrenal | 9 (9/0) | 7 (7/0) | 2 (2/0) |
| Pelvic mass | 6 (6/0) | 4 (4/0) | 2 (2/0) |
| Chest wall/pleura | 6 (3/3) | 2 (2/0) | 4 (1/3) |
| Mediastinum | 4 (4/0) | 3 (3/0) | 1 (1/0) |
| Lytic bone | 2 (1/1) | 2 (1/1) | 0 |
| Muscle | 1 (1/0) | 1 (1/0) | 0 |
| Retroperitoneum | 1 (1/0) | 1 (1/0) | 0 |
| Peritoneum | 1 (0/1) | 0 | 1 (0/1) |
| Pancreas | 1 (0/1) | 0 | 1 (0/1) |
| Total | 100 (63/37) | 45 (37/8) | 55 (26/29) |
All biopsies were performed by one of two radiologists who had several years of experience with percutaneous image guided biopsy.
The patients’ written informed consent was obtained at least 24 h before the biopsy after the nature of the procedure had been fully explained. In in-patients this was done by the radiologist, usually on the day before the procedure. In out-patients informed consent was obtained either by the radiologist when the patient was in the hospital in an out-patient clinic on the day the biopsy was scheduled or informed consent was obtained by the transferring clinician in patients that were transferred to our department only for the biopsy.
The biopsy was performed under ultrasound guidance whenever possible to avoid radiation exposure to the patient and radiologist, using a Sonoline Elegra ™ (Siemens, Erlangen, Germany) with 3.5 or 7.5 MHz transducers. In superficial biopsies (thyroid, superficial lymph nodes) a free-hand technique was used, otherwise a sterile needle guide was mounted on the transducer and the needle tract was projected on the screen using the biopsy mode of the ultrasound machine. Ultrasound settings were adjusted to optimally demonstrate the lesion and anticipated needle tract, mostly using the tissue harmonic imaging mode.
If the lesion or a safe needle tract could not be adequately visualized at ultrasound (e.g. lung, retroperitoneum or bone) CT guidance was used. The CT-fluoroscopy mode was used of a single-detector spiral CT (Somatom Plus 4 Power, Siemens, Erlangen, Germany) and a 16-slice multidetector CT (Lightspeed 16, General Electrics, Milwaukee, USA). With the single-detector scanner continuous CT fluoroscopy was possible but fluoroscopy time was limited to the minimum to reduce radiation exposure. The multi-detector scanner does not allow continuous CT fluoroscopy but only single ‘shots’ up to a maximum of two per second.
In 12 of 100 biopsies conscious sedation with 2–10 mg (mean +/− standard deviation: 4.54 +/− 2.21 mg) Midazolam (Ratiopharm, Ulm, Germany) was performed; in all other cases only local anaesthetic was required.
After sterile draping of the entry site, local anaesthetic (5–10 ml Scandicain ™, Astra Zeneca, Wedel, Germany) was applied to the prospective biopsy tract with particular emphasis on skin, peritoneum, parietal pleura, liver capsule, etc. Depending on lesion location biopsy was performed with coaxial technique or direct puncture. Direct puncture was used in lesions close to the surface of an organ when a guiding needle could not be safely placed within the organ adjacent to the lesion. Coaxial technique was preferred with long and difficult needle tracts if it was expected that many specimens would be required or in patients with coagulation disorders to minimize trauma to the needle tract or organ capsule. Table 2 describes the biopsy technique (guiding technique, coaxial or direct puncture) by organ.
The stroke length of the biopsy was adjusted according to the lesion size and location with regard to proximity to blood vessels or other vulnerable structures and 33 mm stroke length was chosen whenever possible.
After every needle pass the specimen obtained was delivered to a slide, inspected and transferred to a formalin container. A smear was prepared from liquid and tissue fragments remaining on the slide and air-fixed for cytological analysis; the tissue cylinder was fixed in formalin and underwent histological analysis.
The number of needle passes was decided by the radiologist during the procedure depending on the visual impression of whether the needle location within the lesion and the specimens retrieved were adequate. The number of needle passes ranged from 1 to 6 with a mean number of 2.83 +/− 0.92 (mean +/− standard deviation). The number of needle passes was significantly higher with the coaxial technique (mean 3.09 +/− 0.89) than with direct puncture (mean 2.36 +/− 0.80). This was due to the fact that the coaxial technique was used when it was anticipated that multiple needle passes would be required (e.g. in suspected malignant lymphoma). Also, the coaxial technique was used in long and difficult trajectories. Thus, once the guiding needle had been safely placed we tended to obtain more biopsies to avoid a repeat procedure.
We did not specifically record the stroke length of individual needle passes. However, we only used a stroke length of 13 mm in lesions <1 cm and of 23 mm in lesions <2 cm. We specifically aimed at including normal host tissue in the specimen to facilitate a more specific pathologic diagnosis unless the needle pass was likely to touch a vessel, in which case a shorter stroke was selected. Therefore, we believe that >90% of biopsies were obtained using a stroke length of 33 mm.
Cytological and histological diagnosis was made in consensus by two pathologists trained in both cytopathology and histopathology. Usually, the specimen was analysed with haematoxylin and eosin stain and other stains as required. Slides were sent to centres of reference in doubtful cases (particularly malignant lymphoma). It was specifically recorded whether the biopsy material was deemed adequate by the pathologists and whether crush artifacts were reported.
For assessment of the diagnostic accuracy of the biopsy the cytologic–histologic result was compared to the final clinical diagnosis based on all available information.
For assessment of complications the biopsy report as well as the patient’s records were retrospectively reviewed for evidence of new symptoms, imaging findings of complications, procedures initiated because of possible complications and the patient’s final outcome.
Results
Feasibility
In all cases both operators felt that the biopsy was easily possible with the tri-axial, end-cut needle. Loading, placing, firing and removing the needle was easily performed with no failures. In all cases the specimen was easily removed.
Visibility of the needle was excellent at CT and good to excellent at ultrasound depending on the angle of the needle and depth of the lesion. If visibility of the needle was suboptimal in deep locations or steep angles slight movement of the needle helped to identify the needle tip. In no case had a biopsy to be abandoned because of insufficient visibility of the needle.
Accuracy
In all cases adequate material was retrieved as judged by the pathologist and a cytopathological and/or histopathological diagnosis was possible. No biopsy had to be repeated because of insufficient material.
In 77 cases a malignant (40 metastases, 37 primary tumours) and in 23 a benign lesion was diagnosed. Of the 23 benign lesions a specific diagnosis was possible in 22. In one case necrosis and haemorrhage was diagnosed. In this patient surgery and autopsy both only revealed a mediastinal haematoma of unknown origin. Table 3 lists the pathological diagnosis by organs.
Table 3.
Results of cytopathologic/histopathologic analysis by organ
| Organ | Total | Benign | Malignant |
|---|---|---|---|
| Liver | 32 | Toxic damage: 1 Fibrosis: 2 | Hepatocellular carcinoma: 5 Cholangiocellular carcinoma: 1 B-cell-lymphoma: 2 Metastases: 21 - prostate cancer: 2 - lung cancer: 3 - pancreatic cancer: 6 - breast cancer: 4 - cholangiocellular carcinoma: 2 - colorectal carcinoma: 1 - gastric carcinoma: 1 - thyroid carcinoma: 1 - renal cell carcinoma: 1 |
| Lymph nodes | 16 | Lymphadenitis: 1 | Malignant lymphoma: 10 - B-cell lymphoma: 9 - T-cell lymphoma: 1 Metastases: 5 - lung cancer: 1 - malignant melanoma: 1 - neuroendocrine carcinoma: 1 - endometrial carcinoma: 1 - colorectal carcinoma: 1 |
| Thyroid | 11 | Adenoma: 8 Oncocytoma: 1 | Anaplastic carcinoma: 1 Oncocytic carcinoma: 1 |
| Lung | 9 | Lung cancer: 6 - squamous cell carcinoma: 3 - adenocarcinoma: 3 - metastases (renal cell carcinoma): 2 - malignant mesothelioma: 1 | |
| Adrenal | 9 | Adenoma: 2 | Metastases: 7 - lung cancer: 3 - pancreatic carcinoma: 1 - colorectal carcinoma: 1 - renal cell carcinoma: 1 - prostate cancer: 1 |
| Pelvic mass | 6 | Abscess: 1 Retention cyst: 1 | Ovarian carcinoma: 1 Endometrial carcinoma (recurrence): 1 Rectal carcinoma (recurrence): 1 Metastasis (prostate cancer): 1 |
| Chest wall/pleura | 6 | Fibrosis: 1 Chronic inflammation: 1 | Lung cancer 4 - squamous cell carcinoma: 3 - small cell lung cancer: 1 |
| Mediastinum | 4 | Haematoma: 1 | Thymic carcinoma: 1 Biphasic malignant tumour of the mediastinum: 1 Onkocytic carcinoma of thyroid: 1 |
| Lytic bone | 2 | 0 | Metastases: 2 - hepatocellular carcinoma: 1 - pancreatic cancer: 1 |
| Retroperitoneum | 2 | Retroperitoneal fibrosis (Ormond’s disease): 2 | |
| Peritoneum | 1 | 0 | Metastasis (neuroendocrine carcinoma: 1 |
| Pancreas | 1 | 0 | Pancreatic carcinoma: 1 |
| Muscle | 1 | 0 | Metastasis (breast cancer): 1 |
| Total | 100 | 23 | 77 |
The pathology report explicitly included the presence of any tissue alteration and artifacts. There was significant degradation of cytological slides in three biopsies rendering the slides insufficient for cytological assessment. In all three cases the histological specimen provided a specific diagnosis. We believed that the artifacts resulted from exposure of the slides to formalin vapour, probably due to the fact that both the formalin container with the histological specimen and the cytological slides had been sent to the pathology department in one plastic envelope. From then on, we sent both specimens in separate envelopes and did not encounter that problem again.
In one case crush artifacts were reported but it was uncertain whether these were due to the biopsy or improper handling of the specimen at preparation for histology. Otherwise no crush artifacts were reported.
Complications
In 90 of 100 biopsies (90%) no complications were observed. In 10 biopsies 11 complications were noted of which eight were considered minor, requiring no treatment, and three required therapy and were, therefore, considered major complications.
Seven small haemorrhages not requiring any therapy were observed at the end of the procedure by ultrasound or CT. These included minor pleural effusion after lung biopsy in two, and small local haematomas after biopsies of the mediastinum (two) and of liver, bone and thyroid (one each).
After a retroperitoneal biopsy one patient experienced pain for less than 24 h not requiring systemic analgesics. In one patient a small asymtomatic pneumothorax was noted at the end of a lung biopsy not requiring aspiration or drainage.
In three lung biopsies pneumothoraces were noted after the procedure which were deemed large enough to require therapy because of a volume of 30% of the volume of the respective hemithorax. Two patients were asymptomatic. In two cases the pneumothorax was aspirated on the CT table and did not recur; in the other case a small bore chest drain was inserted for 5 days. In all three cases the needle pass had crossed aerated lung between the chest wall and the lesion.
There was no mortality.
Discussion
Image-guided percutaneous biopsy is the ultimate means of establishing the nature of a lesion demonstrated at imaging short of surgical biopsy and is often required in clinical practice.
The ideal percutaneous biopsy should always provide sufficient tissue for a histological diagnosis with no discomfort to the patient, no complications, and as little use of resources as possible with respect to training of the operator, time required for the procedure, use of imaging modalities for guidance and disposable items.
These ideal circumstances are impossible to reach as conditions for these are conflicting:
Sufficient tissue for diagnosis is more likely with larger specimens. These can be obtained through large needles; however, discomfort to the patient and the risk of complications increase with needle calibre. Also, choosing the ideal access route may require extensive use of imaging modalities for guidance.
Thus, every biopsy is a compromise, with the likely benefit—a definitive histological diagnosis—balanced against likelihood of discomfort and risk to the patient and the use of resources. This particularly applies to the type of biopsy needle used: Thin or ultra thin (21–25 gauge) needles reduce trauma to the patient and the risk of complications but are usually only applicable for fine-needle aspiration (FNA) which is mostly sufficient for diagnosis of malignancy but often does not allow a specific diagnosis, particularly in benign lesions [4]. Core biopsy needles can retrieve histological specimens but are more invasive, more expensive and require more training. Furthermore, it is usually easier to decide whether material is adequate for pathological diagnosis with core biopsy than with FNA unless a cytopathologist can immediately assess the aspirate in the biopsy room. Quality of the specimen does not only depend on the amount of tissue obtained but also on the presence or absence of artifacts. Risk increases with needle calibre, lesion depth and duration of the procedure [5].
This was the background of our evaluation of a needle that promises more tissue with no crush artifacts compared to other core needles of the same calibre and reduced risk of losing the specimen. Furthermore, the use of a single needle design for biopsies of different organs with different guiding modalities suggested facilitation of handling.
Our results show that the 18 G needle was adequate to provide sufficient tissue in a variety of conditions including classification of malignant lymphoma and analysis of hormone receptors. In no case had a biopsy to be repeated because of insufficient material. Obviously we performed more than one needle pass in most biopsies but this was mainly done to sample different areas of the lesion rather than because of insufficient tissue at the first biopsy.
The plastic handle of the needle used is relatively heavy (71 g) compared to many other disposable core biopsy needles. This facilitates retrieval of adequate specimens by avoiding recoil during the biopsy which may occur in light-weight systems. On the other hand, the weight of the needle is a disadvantage in superficial or lung biopsies with CT guidance as the needle has to be held with a clamp during CT fluoroscopy to avoid displacement.
The large amount of tissue retrieved by this needle type is confirmed by other studies and was higher with longer stroke lengths and compared to side-notch needles [3, 6].
The fact that some publications on prostate biopsies using the same needle type [3, 6, 7] have reported a significant number of zero biopsies is not easily explained, particularly as the zero rate was higher in one series [6] and lower in another [7] with a longer stroke length. The only ‘zero’ biopsy in our study was obtained in a mediastinal haematoma which is natural. It may be possible that the tissue characteristics of lesions in our series compared to those of prostate tissue are different in that prostate tissue is more elastic and can be pushed away by the needle.
In our study no crush artifacts were attributed to the needle design and artifacts from formaldehyde vapour in cytological slides were no longer encountered with proper handling of the specimens.
Complication rate was low and comparable with other needle designs. The only major complications were three pneumothoraces in nine lung biopsies (33%) that required aspiration or drainage. Pneumothorax is common in lung biopsies, particularly when passage of aerated lung is required to reach a lesion which was the case in all three cases in our series that required therapy of pneumothoraces. In biopsies performed under CT guidance pneumothorax may be demonstrated in as many as 69% of procedures [8]. However, most pneumothoraces are small and asymptomatic, requiring no therapy. In large or symptomatic pneumothoraces therapy is indicated using simple aspiration or continuous drainage through a small bore catheter [5].
In our study one symptomatic pneumothorax required therapy and two asymptomatic pneumothoraces were treated because they were deemed larger than 30% of the volume of the hemithorax. The proportion of pneumothoraces requiring therapy varies significantly in the literature ranging from 1% [9] to 38% [8]. The differences are probably due to lesion size, depth and location, presence or absence of aerated lung and particularly emphysema in the needle path, patient cooperation etc. [5].
Minor complications included one case of mild pain and seven small haematomas demonstrated at imaging not requiring therapy.
Visibility of the needle was excellent at CT-guided biopsies and depended on the surrounding tissue and angle of insertion at ultrasound-guided procedures, as with other needles. In no case had a biopsy to be abandoned because of insufficient visibility.
Handling of the needle was easy due to the fact that only the appropriate needle length had to be chosen, stroke length adjusted and a decision be made whether to use a guiding needle for coaxial technique.
Conclusion
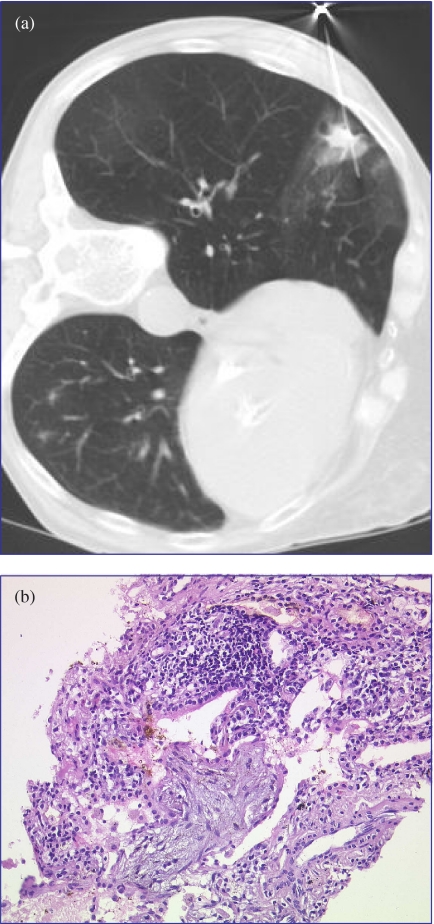
Our results show that the tri-axial, end-cut 18 gauge biopsy needle was easy to handle at both ultrasound- and CT-guided percutaneous biopsies of various organs (Figs. 4 and 5).
Figure 4.
Ultrasound-guided biopsy of a hypoechoic liver lesion: The BioPince ™ needle is shown as a hyperechoic line (arrows). Dotted lines represent predicted needle tract in the ultrasound biopsy mode. Diagnosis: non Hodgkin lymphoma.
Figure 5.
CT-guided biopsy of a lung nodule in a patient with a history of breast cancer. (a) image obtained after passage of the lesion with the 18 G BioPince needle. (b) Histologic specimen demonstrating no crush artifacts. Diagnosis: cryptogenic organizing pneumonia, no evidence of malignancy.
Accuracy of biopsies was high and certainly not inferior, if not superior, to biopsies obtained with other needle types. In particular, no crush artifacts were observed at histology, probably due to the novel end-cut design. Complication rate was low and also comparable to other 18 gauge needles.
We therefore use this needle type for all CT- and US-guided biopsies in all organs except solid bone.
Limitations
Obviously, there are limitations of our study. Only 100 biopsies of different organs were analysed; thus, the number of biopsies of an individual organ is rather small. Rare complications therefore may not have been encountered. The rate of pneumothoraces requiring therapy needs to be evaluated by larger series and we are currently analysing a larger number of lung biopsies with this needle.
In our series all biopsies were performed by only two radiologists with several years of experience with image-guided percutaneous biopsy. Our results may not be reproducible when biopsies are performed by less experienced operators.
Obviously, accuracy of biopsies does not only depend on the needle used and the experience of the interventional radiologist to correctly place the needle but also on the experience of the cyto-/histopathologist. In our study a consensus analysis of both cytological and histological findings was made which is certainly not possible in all institutions.
Future perspectives
Until recently, the biopsy needle investigated was only available with a diameter of 18 gauge.
For specific clinical problems which require large tissue samples for analysis (e.g. classification of malignant lymphoma) larger specimens may be preferred. In spring 2004 a 16 gauge model was launched together with an appropriate 15 gauge guiding needle. Further studies are required to assess feasibility, diagnostic accuracy and complication rate of this needle calibre.
References
- 1.Hopper KD, Abendroth CS, Sturtz KW, Matthews YL, Shirk SJ, Stevens LA. Blinded comparison of biopsy needles and automated devices in vitro: 1 Biopsy of diffuse hepatic disease. Am J Roentgenol. 1993;161:1293–7. doi: 10.2214/ajr.161.6.8249745. [DOI] [PubMed] [Google Scholar]
- 2.Hopper KD, Grenko RT, TenHave TR, Hartzel J, Sturtz KW, Savage CA. Percutaneous biopsy of the liver and kidney by using coaxial technique: adequacy of the specimen obtained with three different needles in vitro. Am J Roentgeneol. 1995;164:221–4. doi: 10.2214/ajr.164.1.7998543. [DOI] [PubMed] [Google Scholar]
- 3.Ubhayakar GN, Li WY, Corbishley CM, Patel U. Improving glandular coverage during prostate biopsy using a core needle: technical performance of an end-cut needle. BJU. 2002;89:40. doi: 10.1046/j.1464-4096.2001.001177.x. [DOI] [PubMed] [Google Scholar]
- 4.Oikonomou A, Matzinger FR, Seely JM, Dennie JC, Macleod PJ. Ultrathin needle (25 G) aspiration lung biopsy: diagnostic accuracy and complication rates. Eur Radiol. 2004;14:375–82. doi: 10.1007/s00330-003-2076-4. [DOI] [PubMed] [Google Scholar]
- 5.Moore EH. Technical aspects of needle aspiration lung biopsy: a personal perspective. Radiology. 1998;208:303–18. doi: 10.1148/radiology.208.2.9680552. [DOI] [PubMed] [Google Scholar]
- 6.Dogan HS, Eskicorapci SY, Ertoy-Baydar D, Akdogan B, Gunay LM, Ozen H. Can we obtain better specimens with an end-cutting prostatic biopsy device. Eur Urol. 2005;47:297–301. doi: 10.1016/j.eururo.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Ozden E, Gogus C, Tulunay O, Baltaci S. The long core needle with an end-cut technique for prostate biopsy: does it really have advantages when compared with standard needles. Eur Urol. 2004;45:287–91. doi: 10.1016/j.eururo.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Gupta S, Krishnamurthy S, Broemeling LD, Morello FA Jr, Wallace MJ, Ahrar K, et al. Small (≤2 cm) subpleural pulmonary lesions: short- versus long-needle-path CT guided biopsy—comparison of diagnostic yields and complications. Radiology. 2005;234:631–7. doi: 10.1148/radiol.2342031423. [DOI] [PubMed] [Google Scholar]
- 9.Yeow KM, Su IH, Pan KT, Tsay PK, Lui KW, Cheung YC, et al. Risk factors of pneumothorax and bleeding: multivariate analysis of 660 CT-guided coaxial cutting needle lung biopsies. Chest. 2004;126:748–54. doi: 10.1378/chest.126.3.748. [DOI] [PubMed] [Google Scholar]