Abstract
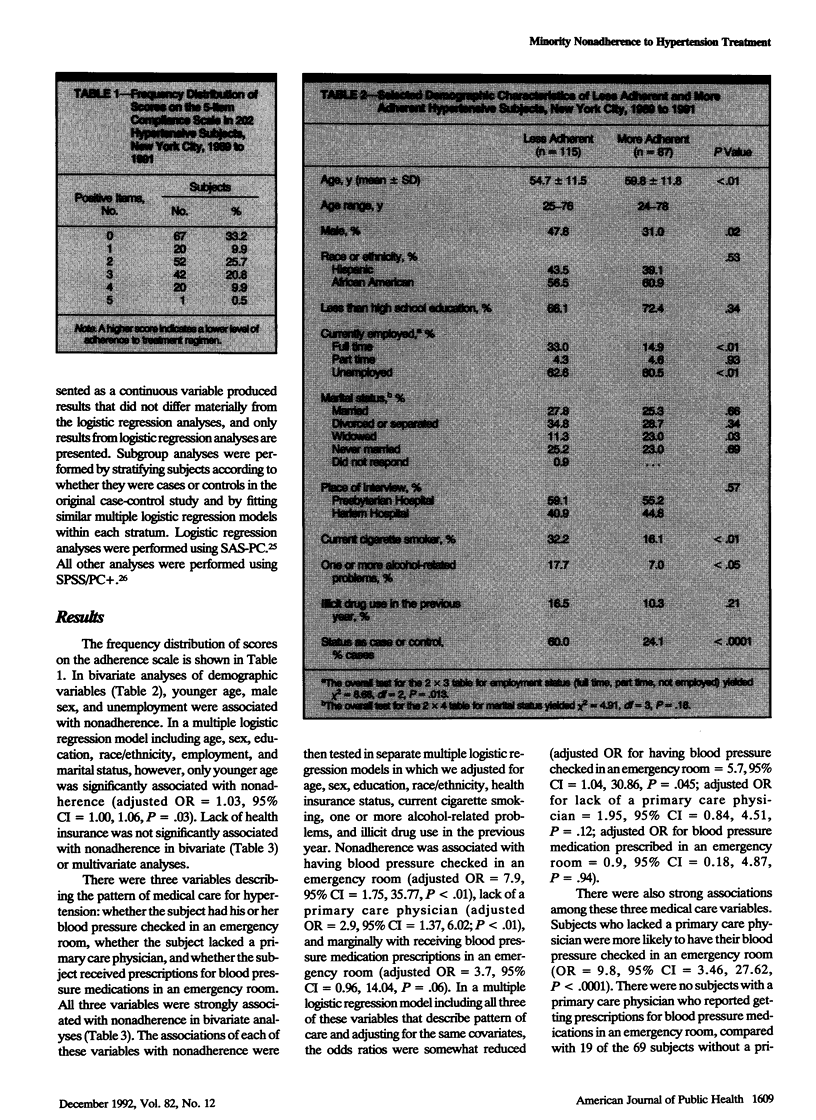
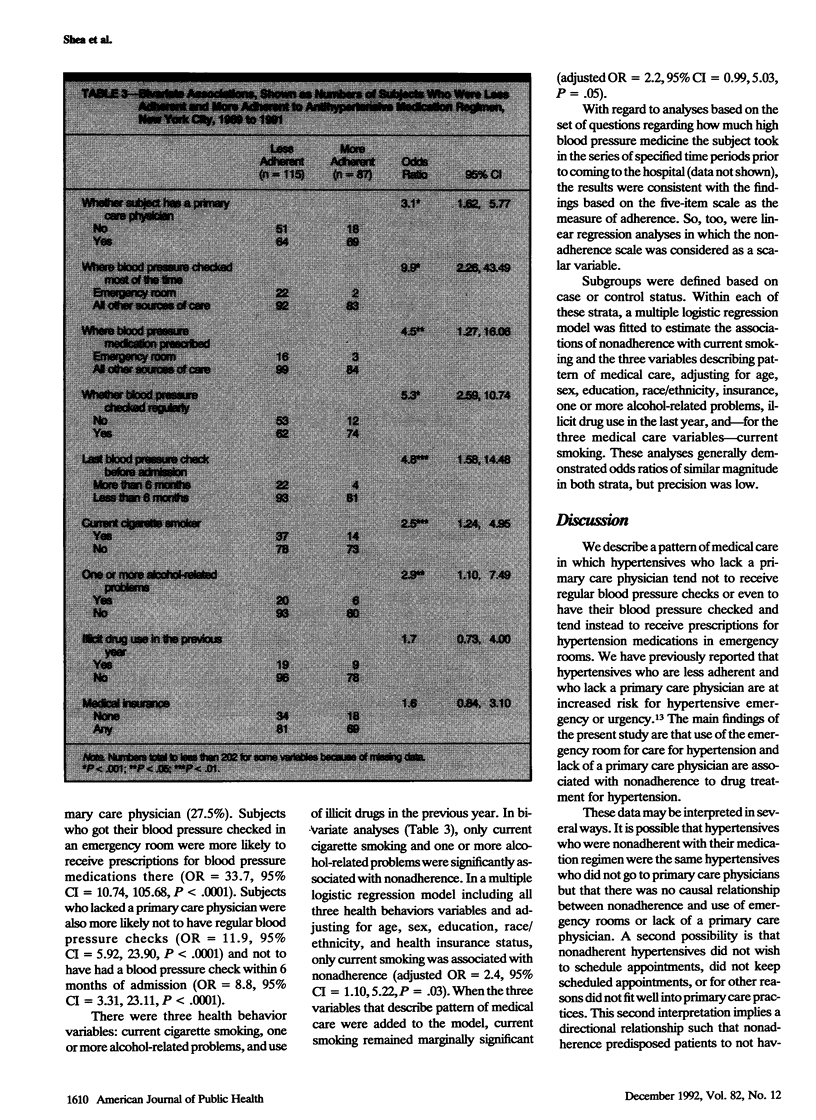
OBJECTIVE. Adherence to treatment is a key factor in achieving blood pressure control among hypertensives. We examined correlates of nonadherence to hypertension treatment in an inner-city minority population. METHODS. Subjects (n = 202) were interviewed as part of a case-control study of severe, uncontrolled hypertension conducted in two New York City hospitals in 1989-91. All subjects were African American or Hispanic. Self-reported nonadherence to drug treatment for hypertension was measured using a five-item scale, and the sample was dichotomized as more (n = 87) or less (n = 115) adherent. Multiple logistic regression analysis was used to adjust for demographic and other covariates. RESULTS. Nonadherence was associated with having blood pressure checked in an emergency room (adjusted odds ratio [OR] = 7.9; 95% confidence interval [CI] = 1.75, 35.77; P < .01), lack of a primary care physician (adjusted OR = 2.9; 95% CI = 1.37, 6.02; P < .01), current smoking (adjusted OR = 2.4; 95% CI = 1.10, 5.22; P = .03), and younger age (adjusted OR = 1.03, 95% CI = 1.00, 1.06; P = .03). CONCLUSIONS. Changing the locus of care for hypertension from emergency rooms to primary care physicians may improve adherence to hypertension treatment in minority populations.
Full text
PDF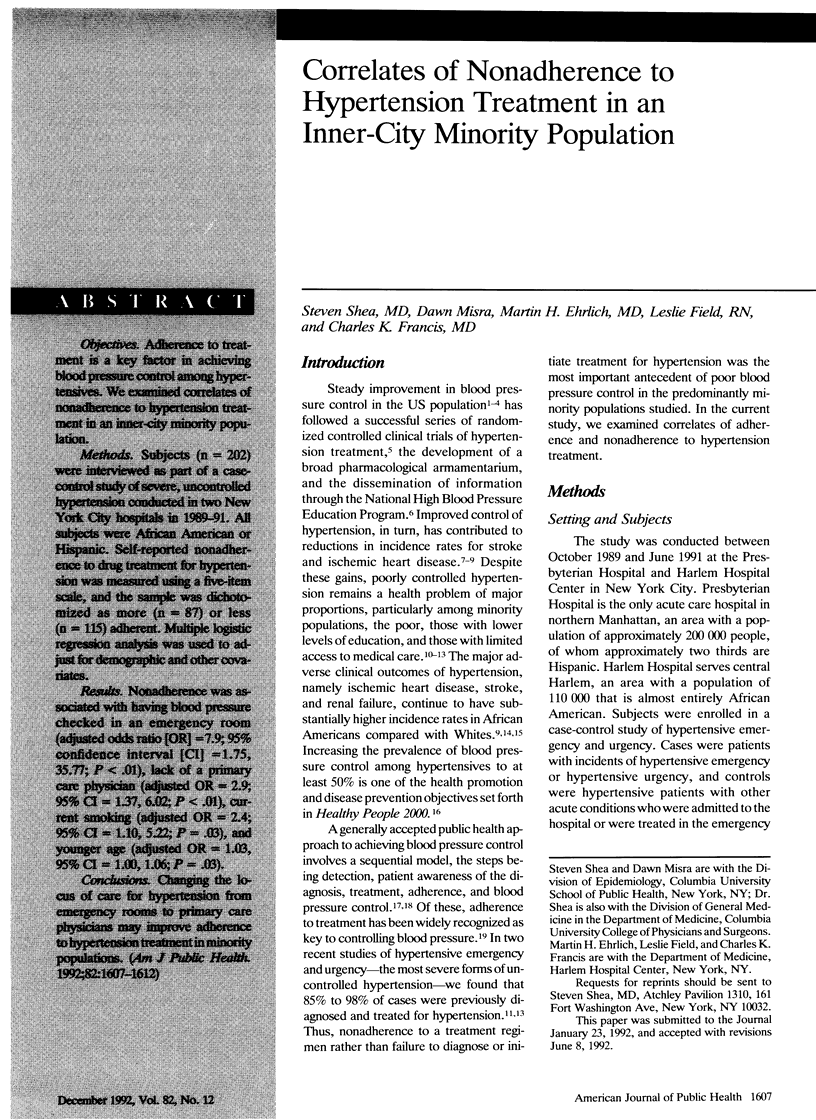

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bennett N. M., Shea S. Hypertensive emergency: case criteria, sociodemographic profile, and previous care of 100 cases. Am J Public Health. 1988 Jun;78(6):636–640. doi: 10.2105/ajph.78.6.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkson D. M., Brown M. C., Stanton H., Masterson J., Shireman L., Ausbrook D. K., Mikes D., Whipple I. T., Muriel H. H. Changing trends in hypertension detection and control: the Chicago experience. Am J Public Health. 1980 Apr;70(4):389–393. doi: 10.2105/ajph.70.4.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand F. N., Smith R. T., Brand P. A. Effect of economic barriers to medical care on patients' noncompliance. Public Health Rep. 1977 Jan-Feb;92(1):72–78. [PMC free article] [PubMed] [Google Scholar]
- Clark L. T. Improving compliance and increasing control of hypertension: needs of special hypertensive populations. Am Heart J. 1991 Feb;121(2 Pt 2):664–669. doi: 10.1016/0002-8703(91)90443-l. [DOI] [PubMed] [Google Scholar]
- Collins R., Peto R., MacMahon S., Hebert P., Fiebach N. H., Eberlein K. A., Godwin J., Qizilbash N., Taylor J. O., Hennekens C. H. Blood pressure, stroke, and coronary heart disease. Part 2, Short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet. 1990 Apr 7;335(8693):827–838. doi: 10.1016/0140-6736(90)90944-z. [DOI] [PubMed] [Google Scholar]
- Folsom A. R., Luepker R. V., Gillum R. F., Jacobs D. R., Prineas R. J., Taylor H. L., Blackburn H. Improvement in hypertension detection and control from 1973-1974 to 1980-1981. The Minnesota Heart Survey experience. JAMA. 1983 Aug 19;250(7):916–921. [PubMed] [Google Scholar]
- Francis C. K. Hypertension, cardiac disease, and compliance in minority patients. Am J Med. 1991 Jul 18;91(1A):29S–36S. doi: 10.1016/0002-9343(91)90060-b. [DOI] [PubMed] [Google Scholar]
- Goldman L., Cook E. F. The decline in ischemic heart disease mortality rates. An analysis of the comparative effects of medical interventions and changes in lifestyle. Ann Intern Med. 1984 Dec;101(6):825–836. doi: 10.7326/0003-4819-101-6-825. [DOI] [PubMed] [Google Scholar]
- Keeler E. B., Brook R. H., Goldberg G. A., Kamberg C. J., Newhouse J. P. How free care reduced hypertension in the health insurance experiment. JAMA. 1985 Oct 11;254(14):1926–1931. [PubMed] [Google Scholar]
- Kittner S. J., White L. R., Losonczy K. G., Wolf P. A., Hebel J. R. Black-white differences in stroke incidence in a national sample. The contribution of hypertension and diabetes mellitus. JAMA. 1990 Sep 12;264(10):1267–1270. [PubMed] [Google Scholar]
- Manson A. Language concordance as a determinant of patient compliance and emergency room use in patients with asthma. Med Care. 1988 Dec;26(12):1119–1128. doi: 10.1097/00005650-198812000-00003. [DOI] [PubMed] [Google Scholar]
- McNagny S. E., Parker R. M. High prevalence of recent cocaine use and the unreliability of patient self-report in an inner-city walk-in clinic. JAMA. 1992 Feb 26;267(8):1106–1108. [PubMed] [Google Scholar]
- Morisky D. E., Green L. W., Levine D. M. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986 Jan;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- Ostfeld A. M., Wilk E. Epidemiology of stroke, 1980-1990: a progress report. Epidemiol Rev. 1990;12:253–256. doi: 10.1093/oxfordjournals.epirev.a036059. [DOI] [PubMed] [Google Scholar]
- Pappas G., Gergen P. J., Carroll M. Hypertension prevalence and the status of awareness, treatment, and control in the Hispanic Health and Nutrition Examination Survey (HHANES), 1982-84. Am J Public Health. 1990 Dec;80(12):1431–1436. doi: 10.2105/ajph.80.12.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roccella E. J., Horan M. J. The National High Blood Pressure Education Program: measuring progress and assessing its impact. Health Psychol. 1988;7 (Suppl):297–303. [PubMed] [Google Scholar]
- Rostand S. G., Kirk K. A., Rutsky E. A., Pate B. A. Racial differences in the incidence of treatment for end-stage renal disease. N Engl J Med. 1982 May 27;306(21):1276–1279. doi: 10.1056/NEJM198205273062106. [DOI] [PubMed] [Google Scholar]
- Shea S., Misra D., Ehrlich M. H., Field L., Francis C. K. Predisposing factors for severe, uncontrolled hypertension in an inner-city minority population. N Engl J Med. 1992 Sep 10;327(11):776–781. doi: 10.1056/NEJM199209103271107. [DOI] [PubMed] [Google Scholar]
- Shea S., Stein A. D., Basch C. E., Lantigua R., Maylahn C., Strogatz D. S., Novick L. Independent associations of educational attainment and ethnicity with behavioral risk factors for cardiovascular disease. Am J Epidemiol. 1991 Sep 15;134(6):567–582. doi: 10.1093/oxfordjournals.aje.a116130. [DOI] [PubMed] [Google Scholar]
- Shea S., Stein A. D., Lantigua R., Basch C. E. Reliability of the behavioral risk factor survey in a triethnic population. Am J Epidemiol. 1991 Mar 1;133(5):489–500. doi: 10.1093/oxfordjournals.aje.a115916. [DOI] [PubMed] [Google Scholar]
- Shulman N. B., Martinez B., Brogan D., Carr A. A., Miles C. G. Financial cost as an obstacle to hypertension therapy. Am J Public Health. 1986 Sep;76(9):1105–1108. doi: 10.2105/ajph.76.9.1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton A. L. Determinants of adherence to medical regimens by hypertensive patients. J Behav Med. 1987 Aug;10(4):377–394. doi: 10.1007/BF00846477. [DOI] [PubMed] [Google Scholar]



