Abstract
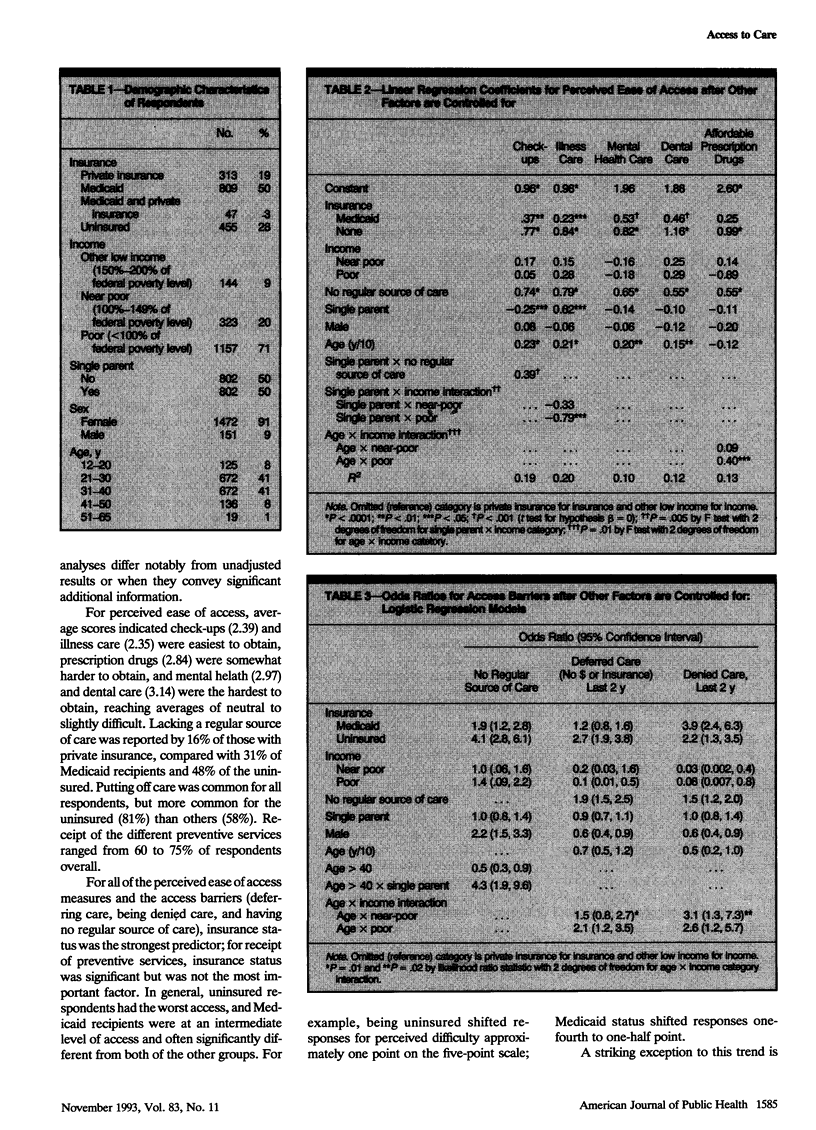
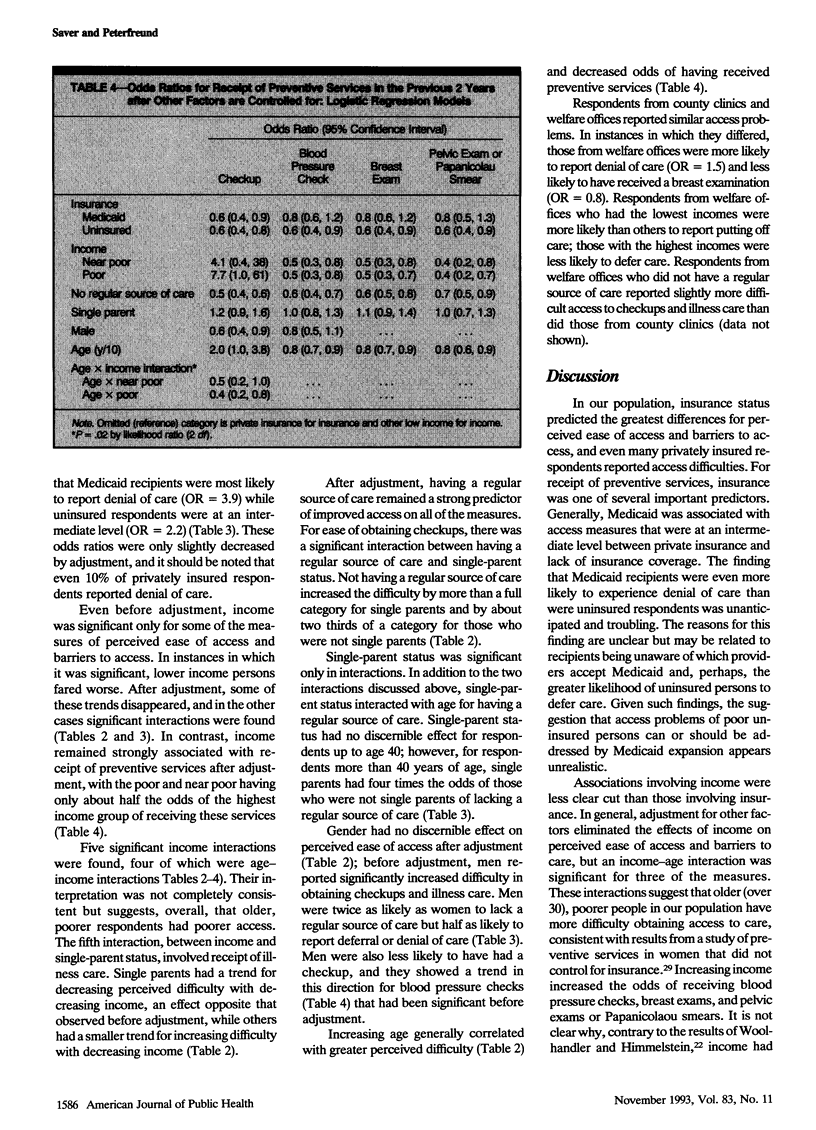
OBJECTIVES. We studied simultaneous effects of income and insurance on access measures in an indigent population, focusing on Medicaid and the marginal effects of increasing income. METHODS. Surveys were distributed in waiting rooms of county clinics and welfare offices. Models examined insurance (private, Medicaid, or none), income (to twice the poverty level), single-parent status, age, gender, and presence of a regular source of care; first-order interactions were evaluated. RESULTS. In terms of ease of access, postponing care, and having a regular source of care, uninsured respondents fared worst and Medicaid recipients were at an intermediate level. However, relative to those with private insurance, Medicaid recipients had four times the odds, and uninsured respondents twice the odds of being denied care. Income had no consistent effect; however, older, poorer people may have greater problems. For preventive services, income was significant, while differences between Medicaid and private insurance were generally not significant. CONCLUSIONS. Except for denial of care, access for indigent people is improved by Medicaid but remains worse than the access of those with private insurance. Income had variable effects, but support for income criteria used for public insurance eligibility was not found.
Full text
PDF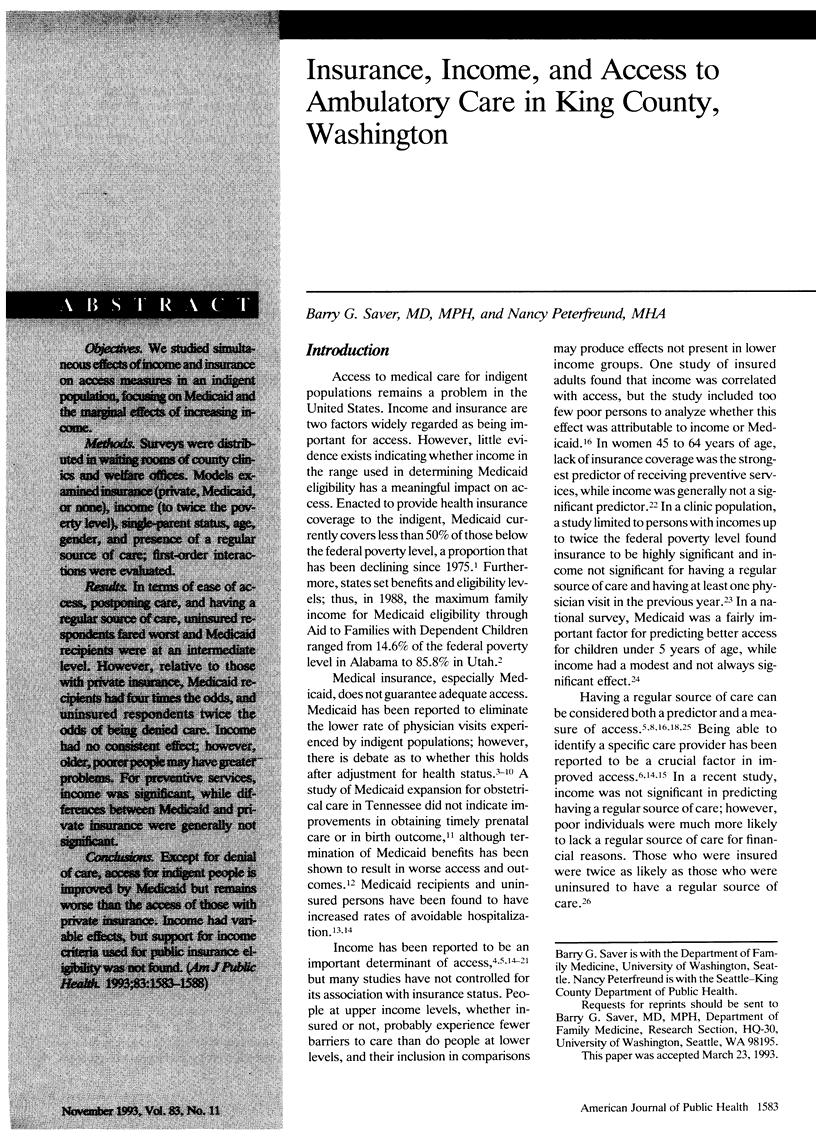



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aday L. A., Andersen R. M. The national profile of access to medical care: where do we stand? Am J Public Health. 1984 Dec;74(12):1331–1339. doi: 10.2105/ajph.74.12.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billings J., Teicholz N. Uninsured patients in District of Columbia hospitals. Health Aff (Millwood) 1990 Winter;9(4):158–165. doi: 10.1377/hlthaff.9.4.158. [DOI] [PubMed] [Google Scholar]
- Blendon R. J., Aiken L. H., Freeman H. E., Kirkman-Liff B. L., Murphy J. W. Uncompensated care by hospitals or public insurance for the poor. Does it make a difference? N Engl J Med. 1986 May 1;314(18):1160–1163. doi: 10.1056/NEJM198605013141806. [DOI] [PubMed] [Google Scholar]
- Davis K., Gold M., Makuc D. Access to health care for the poor: does the gap remain? Annu Rev Public Health. 1981;2:159–182. doi: 10.1146/annurev.pu.02.050181.001111. [DOI] [PubMed] [Google Scholar]
- Gittelsohn A. M., Halpern J., Sanchez R. L. Income, race, and surgery in Maryland. Am J Public Health. 1991 Nov;81(11):1435–1441. doi: 10.2105/ajph.81.11.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward R. A., Bernard A. M., Freeman H. E., Corey C. R. Regular source of ambulatory care and access to health services. Am J Public Health. 1991 Apr;81(4):434–438. doi: 10.2105/ajph.81.4.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward R. A., Shapiro M. F., Freeman H. E., Corey C. R. Inequities in health services among insured Americans. Do working-age adults have less access to medical care than the elderly? N Engl J Med. 1988 Jun 9;318(23):1507–1512. doi: 10.1056/NEJM198806093182305. [DOI] [PubMed] [Google Scholar]
- Hayward R. A., Shapiro M. F., Freeman H. E., Corey C. R. Who gets screened for cervical and breast cancer? Results from a new national survey. Arch Intern Med. 1988 May;148(5):1177–1181. [PubMed] [Google Scholar]
- Howell E. M. Low-income persons' access to health care: NMCUES Medicaid data. Public Health Rep. 1988 Sep-Oct;103(5):507–514. [PMC free article] [PubMed] [Google Scholar]
- Hubbell F. A., Waitzkin H., Mishra S. I., Dombrink J. Evaluating health-care needs of the poor: a community-oriented approach. Am J Med. 1989 Aug;87(2):127–131. doi: 10.1016/s0002-9343(89)80686-2. [DOI] [PubMed] [Google Scholar]
- Kleinman J. C., Gold M., Makuc D. Use of ambulatory medical care by the poor: another look at equity. Med Care. 1981 Oct;19(10):1011–1029. doi: 10.1097/00005650-198110000-00004. [DOI] [PubMed] [Google Scholar]
- Lurie N., Ward N. B., Shapiro M. F., Brook R. H. Termination from Medi-Cal--does it affect health? N Engl J Med. 1984 Aug 16;311(7):480–484. doi: 10.1056/nejm198408163110735. [DOI] [PubMed] [Google Scholar]
- Makuc D. M., Freid V. M., Kleinman J. C. National trends in the use of preventive health care by women. Am J Public Health. 1989 Jan;79(1):21–26. doi: 10.2105/ajph.79.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus A. C., Crane L. A. Telephone surveys in public health research. Med Care. 1986 Feb;24(2):97–112. doi: 10.1097/00005650-198602000-00002. [DOI] [PubMed] [Google Scholar]
- Newacheck P. W. Access to ambulatory care for poor persons. Health Serv Res. 1988 Aug;23(3):401–419. [PMC free article] [PubMed] [Google Scholar]
- Newacheck P. W., Halfon N. Access to ambulatory care services for economically disadvantaged children. Pediatrics. 1986 Nov;78(5):813–819. [PubMed] [Google Scholar]
- Oberg C. N., Polich C. L. Medicaid: entering the third decade. Health Aff (Millwood) 1988 Fall;7(4):83–96. doi: 10.1377/hlthaff.7.4.83. [DOI] [PubMed] [Google Scholar]
- Piper J. M., Ray W. A., Griffin M. R. Effects of Medicaid eligibility expansion on prenatal care and pregnancy outcome in Tennessee. JAMA. 1990 Nov 7;264(17):2219–2223. [PubMed] [Google Scholar]
- Rogers D. E., Blendon R. J., Moloney T. W. Who needs Medicaid? N Engl J Med. 1982 Jul 1;307(1):13–18. doi: 10.1056/NEJM198207013070103. [DOI] [PubMed] [Google Scholar]
- Rosenbach M. L. The impact of Medicaid on physician use by low-income children. Am J Public Health. 1989 Sep;79(9):1220–1226. doi: 10.2105/ajph.79.9.1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short P. F., Lefkowitz D. C. Encouraging preventive services for low-income children. The effect of expanding Medicaid. Med Care. 1992 Sep;30(9):766–780. doi: 10.1097/00005650-199209000-00002. [DOI] [PubMed] [Google Scholar]
- Taube C. A., Rupp A. The effect of Medicaid on access to ambulatory mental health care for the poor and near-poor under 65. Med Care. 1986 Aug;24(8):677–686. doi: 10.1097/00005650-198608000-00003. [DOI] [PubMed] [Google Scholar]
- Weissman J. S., Gatsonis C., Epstein A. M. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. JAMA. 1992 Nov 4;268(17):2388–2394. [PubMed] [Google Scholar]
- Wilensky G., Berk M. L. Health care, the poor, and the role of Medicaid. Health Aff (Millwood) 1982 Fall;1(4):93–100. doi: 10.1377/hlthaff.1.4.93. [DOI] [PubMed] [Google Scholar]
- Woolhandler S., Himmelstein D. U. Reverse targeting of preventive care due to lack of health insurance. JAMA. 1988 May 20;259(19):2872–2874. [PubMed] [Google Scholar]


