Abstract
Tsetse flies (Glossina sp.) are the vectors that transmit African trypanosomes, protozoan parasites that cause human sleeping sickness and veterinary infections in the African continent. These blood-feeding dipteran insects deposit saliva at the feeding site that enables the blood-feeding process. Here we demonstrate that tsetse fly saliva also accelerates the onset of a Trypanosoma brucei infection. This effect was associated with a reduced inflammatory reaction at the site of infection initiation (reflected by a decrease of interleukin-6 [IL-6] and IL-12 mRNA) as well as lower serum concentrations of the trypanocidal cytokine tumor necrosis factor. Variant-specific surface glycoprotein-specific antibody isotypes immunoglobulin M (IgM) and IgG2a, implicated in trypanosome clearance, were not suppressed. We propose that tsetse fly saliva accelerates the onset of trypanosome infection by inhibiting local and systemic inflammatory responses involved in parasite control.
African trypanosomes are extracellular protozoan flagellates that infect a broad range of vertebrate hosts, including humans, and rely for their transmission on tsetse flies (Glossina sp.), which are obligately blood-feeding organisms (62). In the mammalian host, the parasites establish controlled growth to ensure survival and optimal transmission. In order to escape the adaptive immune system, trypanosomes undergo antigenic variation by altering their major surface antigen, the variant-specific surface glycoprotein (VSG) (6). Beside this immune evasion mechanism, trypanosomes have been shown to modulate immune functions of macrophages (8, 43), T lymphocytes (56), and B lymphocytes (2). The main host immune effectors involved in parasite control are considered to be trypanosome-specific antibodies (30) and the cytokine tumor necrosis factor (TNF) (33). Concerning trypanosome-specific antibodies, increased VSG-reactive immunoglobulin M (IgM) and IgG2a antibody isotypes have been associated with improved control of trypanosome infections (34, 55). TNF, as a host cytokine, was released from activated macrophages in response to stimulation by soluble VSG (sVSG) and membrane-bound VSG (11, 35). TNF was demonstrated to have trypanocidal properties for certain trypanosome stocks and to be associated with the occurrence of immune pathology in infected animals (33). As such, direct or indirect modulation of parasite-specific antibody induction and TNF release might influence trypanosome growth and the severity of infection.
Focusing on the early stage of trypanosome infection in the mammalian host, the effect of tsetse fly salivary components on parasitemia onset and on the involved host antiparasite immune effectors has been poorly investigated. Studies with other blood-sucking arthropods, such as ticks and sand flies, have demonstrated that salivary proteins are potent modulators of host innate and adaptive immune responses. Especially for ticks, which are characterized by their extended feeding time, a broad repertoire of immune modulatory activities has been described. These modulatory activities include the predominant induction of a Th2 response with an overall inhibition of proinflammatory and Th1 cytokines (23, 24, 38, 54), suppression of the effector functions of antigen-presenting cells (APCs) (5, 26, 28, 59), and modulation of T-cell (28, 59) and B-cell (17, 18) responses, as well as the inhibition of granulocyte infiltration (39, 53) and NK-mediated cytotoxicity (25). Illustrating the importance of salivary components for pathogen transmission, the tick protein Salp15 was shown to significantly increase the infectivity of Borrelia burgdorferi spirochetes in mice (50). Also, previous studies indicate that salivary extracts from Old and New World sand flies modulate several effector functions of the host immune system, promoting the initial Leishmania infection at the inoculation site (3, 16, 32, 58, 60).
A general immunological effect observed in several studied vector-host interaction models is an anti-inflammatory action of the salivary components and the occurrence of a Th2-associated cytokine response in exposed hosts (23, 24, 37, 38, 54). Consistent with this, we have previously demonstrated that tsetse fly saliva also biases the immune system to a Th2 response (4), possibly reflecting the anti-inflammatory potential of tsetse fly saliva. As a proinflammatory response in an early stage of trypanosome infection has been shown to be crucial for efficient control of parasitemia (21, 33, 44), a putative anti-inflammatory property of tsetse fly saliva might enhance trypanosome progression at the early stage of infection. Moreover, tsetse fly saliva was shown to suppress IgG responses against the heterologous antigen ovalbumin (4). As such, the salivary components might also influence the host antitrypanosome antibody induction responsible for parasite clearance. This paper describes the effect of Glossina morsitans morsitans saliva on the onset of a Trypanosoma brucei brucei infection in mice and the associated immune responses.
MATERIALS AND METHODS
Animals.
Six- to 8-week-old female Toll-like receptor-2/4 (TLR-2/4)-deficient mice (Jackson Laboratory, Bar Harbor, ME) were used for the experimental infections. Six- to 8-week-old female in-house-bred (BALB/c × C57BL/6)F1 mice were used for antisaliva immunization and natural trypanosome infection via tsetse flies. Mouse care and experimental procedures were performed under approval from the Animal Ethical Committee of the Vrije Universiteit Brussel. Tsetse flies (Glossina morsitans morsitans) were available from the insectaria at the Prins Leopold Institute of Tropical Medicine Antwerp (ITMA) and originated from puparia collected in Kariba (Zimbabwe) and Handeni (Tanzania). Flies were fed on rabbits and maintained at 26°C and at a relative humidity of 65%. Animal ethics approval for the tsetse fly feeding on live animals was obtained from the Animal Ethical Committee of the Institute of Tropical Medicine, Antwerp (Belgium).
Parasites.
Pleomorphic AnTat1.1E Trypanosoma brucei brucei parasites were used for the experimental infections done by use of an intradermal injection method. Parasites were grown in mice and purified from their heparinized blood by using DEAE-cellulose (DE52; Whatman) anion-exchange chromatography (27). Parasites were collected in PSG buffer (phosphate-buffered saline [PBS] [pH 7.4] supplemented with 10% glucose), centrifuged at 850 × g, and resuspended in sterile PBS or RPMI 1640 prior to injection.
For natural infection experiments, tsetse flies were infected with the AnTAR1 Trypanosoma brucei brucei parasite strain, which was shown to efficiently develop into a mature salivary gland infection.
sVSG purification.
The soluble form of the glycosylphosphatidylinositol-anchored VSG was purified from isolated AnTat1.1E parasites following a stress-induced activation (50 mM NaH2PO4, pH 5.5) of the endogenous phospholipase (PLC) releasing the VSG from its membrane anchor. sVSG was further purified using a combination of ion-exchange and gel filtration chromatography (7).
Tsetse fly saliva isolates.
Three days after the last blood meal, 10- to 15-day-old noninfected tsetse flies were dissected under a binocular microscope, and salivary glands were isolated using forceps and collected in ice-cold, sterile PBS (pH 7.4). Saliva was allowed to outflow into the buffer solution and was subsequently separated from the salivary glands by centrifugation for 1 min at 12,000 × g. The supernatant (i.e., saliva) was sterilized by filtration through a 0.2-μm-pore-size filter. Protein concentrations were assessed by a bicinchoninic acid protein assay reagent kit (Pierce Biotechnology), and aliquots stored at −20°C. The approximate yield of eluted saliva proteins was approximately 5 μg per salivary gland.
Natural and experimental exposure to tsetse fly saliva.
Natural exposure to tsetse fly saliva was performed by allowing 15 flies per mouse (n = 6) to feed twice a week over a period of 5 weeks. An additional six F1 mice were experimentally immunized by priming with 5 μg saliva in Freund's complete adjuvant and boosting twice at three weekly intervals by administering the same dose in Freund's incomplete adjuvant subcutaneously at the tail base. Control mice were subjected to the same injection schedule with only adjuvant in PBS. From all exposed mice, sera were collected 14 days after the last boost for analysis of the immune response.
Intrapinnal trypanosome infections.
Experimental trypanosome infections were initiated intradermally in the presence and absence of 5 μg saliva (equivalent to the contents of one salivary gland). The inoculation consisted of a single injection of 25 μl buffer containing 2000 AnTat1.1E trypanosomes with or without 5 μg saliva between the ventral and dorsal ear dermis (intrapinnally) by using a gauge 30 insulin microsyringe. Saliva was added to the trypanosome inoculum just prior to injection, and inoculated doses were confirmed retrospectively by parasite counting. Parasitemia was analyzed microscopically using a Bürker hematocytometer in 1/200-diluted blood samples taken from the tail vein.
Tsetse fly-transmitted trypanosome infections.
Freshly emerged tsetse flies were infected by feeding on AnTAR1-infected mice at the peak of parasitemia. In order to obtain a pleomorphic trypanosome population at high titer, these mice were immune suppressed with cyclophosphamide (20 mg/kg of body weight). Twenty-eight days after the infecting blood meal, flies were screened for a mature salivary gland infection by induced probing on prewarmed glass slides followed by a microscopic analysis for the presence of metacyclic trypanosomes in the saliva. Infection of tsetse flies with T. brucei parasites was performed in compliance with the regulations for biosafety and under approval from the environmental administration of the Flemish government.
To initiate a natural infection, one individual tsetse fly with a mature salivary gland infection was allowed to feed per mouse. To avoid interrupted tsetse feeding, mice were anesthetized prior to the tsetse exposure. Parasitemia of the infected mice was analyzed microscopically in blood samples taken from the tail vein.
Dermal and WBC RNA extraction.
In order to analyze local inflammatory responses upon infection in the ear dermis, total RNA was extracted from the ear dermal layers using TRIzol reagent (GIBCO-Invitrogen) following the manufacturer's recommendations. Systemic immune responses during infection were assessed at the mRNA level in the white blood cell (WBC) fraction of total heparinized blood. The WBC fraction was obtained by erythrocyte lysis that was achieved by a 1/5 dilution of the blood in erythrocyte lysis buffer (10 mM Tris-HCl [pH 7.5], 0.83% NH4Cl). After 5 min, the lysis was stopped by adding 3 volumes of RPMI 1640 medium (GIBCO-Invitrogen), and cells were pelleted by centrifugation for 8 min at 410 × g. RNA was extracted from the cell pellet using TRIzol reagent.
Quantitative reverse transcription-PCR (RT-QPCR) analysis.
One microgram of total RNA was reverse transcribed using oligo(dT)12-18 and Superscript II reverse transcriptase (GIBCO-Invitrogen). Quantitative real-time PCR was performed in a Bio-Rad (Hercules, CA) iCycler with Bio-Rad iQ SYBR green Supermix. PCR conditions were as described before (48, 49). Used primers were as follows: gamma interferon (IFN-γ) sense (5′-GCTCTGAGACAATGAACGCT-3′), IFN-γ antisense (5′-AAAGAGATAATCTGGCTCTGC-3′), interleukin-6 (IL-6) sense (5′-GTCAGATACCTGACAACAGG-3′), IL-6 antisense (5′-GTCTTCTGGAGTACCATAGC-3′), inducible nitric oxide synthase (iNOS) sense (5′-TCCACCAGGAGATGTTGAAC-3′), iNOS antisense (5′-TGGAGCCAAGGCCAAACACAG-3′), IL-12p35 sense (5′-GGAGGTTTCTGGCGCAGAGT-3′), IL-12p35 antisense (5′-GATGACATGGTGAAGACGGCC-3′), TNF sense (5′-GTCTACTCCCAGGTTCTCTTC-3′), TNF antisense (5′-CCTTCACAGAGCAATGACTC-3′), IL-10 sense (5′-GGACTTTAAGGGTTACTTGG-3′), IL-10 antisense (5′-ACTCAATACACACTGCAGGTG-3′), S12 sense (5′-CCTCGATGACATCCTTGGCCTGAG-3′), and S12 antisense (5′-GGAAGGCATAGCTGCTGGAGGTGT-3′). The amplicon sizes were, respectively, 229, 368, 458, 401, 302, 344, and 367 bp. For all primer sets, each PCR cycle consisted of 1 min of denaturation at 94°C, 45 s of annealing at 54°C, and 1 min of extension at 72°C. Gene expression was normalized using the gene encoding ribosomal protein S12 as an extensively validated housekeeping gene (14, 61) and expressed relative to the naive condition.
Serum cytokine analysis.
Cytokine responses (IFN-γ, TNF alpha, and IL-10) were analyzed for sera from mice infected at different time points after infection by cytokine-specific sandwich enzyme-linked immunosorbent assays (ELISAs) (Pharmingen, R&D Systems) using horseradish peroxidase-based detection.
Antigen-specific antibody titers and Ig isotypes.
Murine antitrypanosome antibody responses were assessed by solid-phase ELISA. For antibody titer measurement and isotype determination, Immunosorb plates (Nunc) were coated with 200 ng AnTat1.1E sVSG per well in 0.1 M NaHCO3 (pH 8.3) and blocked with 10% fetal bovine serum in PBS. Serial one-half serum dilutions were applied to antigen-coated wells followed by specific immunoglobulin (IgG1, IgG2a, IgG2b, IgG3, and IgM) detection using an isotyping kit (EmTec).
Graphs and statistical analysis.
All graphs were prepared by the use of GraphPad Prism 4.0 software (GraphPad Software). The same software was used for statistical analysis (two-tailed unpaired t tests, one-way analysis of variance) of the data. Data are represented as means ± standard errors of the mean.
RESULTS
Tsetse fly saliva accelerates the early onset of trypanosome infection.
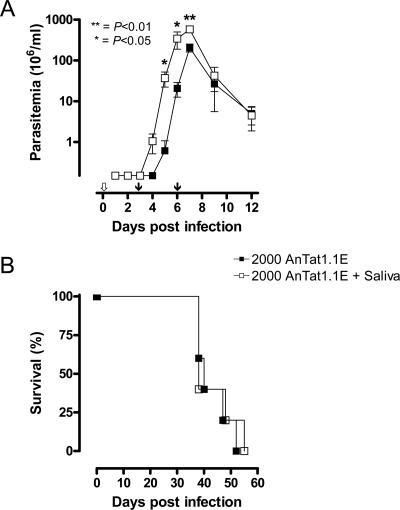
Trypanosome infections were initiated intrapinnally in the presence and absence of tsetse fly saliva, and parasite concentrations in the blood were subsequently analyzed. Experimental infections were conducted in TLR-2/4−/− mice to exclude the effect of bacterial endotoxins that are present in the saliva isolates due to the harvesting procedure (data not shown). In four independent experiments, a significant infection-accelerating effect of tsetse fly saliva was observed in the early stage of infection (Fig. 1A). This observation includes a reproducible earlier detection of parasites within 4 days of infection in the tail vein blood samples and statistically significant higher parasite concentrations up to the first parasitemia peak (day 5, P < 0.05; day 6, P < 0.05; day 7, P < 0.01) for mice in which the trypanosomes were coinjected with tsetse saliva. The differences in absolute peak parasitemia levels were not always statistically significant, and no long-lasting effect of saliva on the parasite levels was observed after the first peak (Fig. 1A). As such, survival times were not significantly different between the two experimental series (Fig. 1B).
FIG. 1.
Initiation of T. brucei brucei AnTat1.1E infections in the presence and absence of G. morsitans morsitans saliva. Shown are the effects on the parasitemia (A) and survival (B) of TLR-2/4−/− mice. Arrows in panel A indicate the analysis of early inflammatory responses at the dermal infection site by RT-QPCR (empty arrow, 1 and 3 hours after infection initiation) and systemic immune responses measured by ELISA for serum and by RT-QPCR for RNA extracted from the white blood cell fraction (filled arrows, 3 and 6 days after infection initiation). The presented data are representative of four independent experiments with at least four mice per group.
Saliva suppresses early inflammatory responses in the dermal infection site.
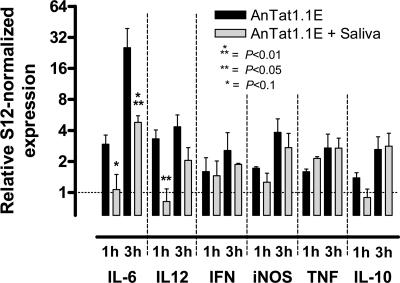
The early onset of a local inflammatory response upon intradermal trypanosome inoculation with or without saliva was analyzed by RT-QPCR on RNA extracts from the ear dermis. Inflammatory cytokine mRNA levels were upregulated within 3 hours of trypanosome infection. Upon coadministration of the parasites with saliva, local transcription of early inflammatory cytokines IL-6 and IL-12p35 was suppressed after, respectively, 1 (IL-6, P < 0.1; IL-12p35, P < 0.05) and 3 (IL-6, P < 0.01; IL-12p35, P = 0.17) hours of infection (Fig. 2). Dermal transcription of IFN-γ, iNOS, TNF, and IL-10 was slightly upregulated upon infection but not significantly altered within 3 h of infection upon coadministration of saliva.
FIG. 2.
Local effects of tsetse fly saliva on dermal inflammation at 1 and 3 hours after infection of TLR-2/4−/− mice: relative S12-normalized levels of mRNA encoding IL-6, IL-12, IFN-γ, iNOS, TNF, and IL-10 in dermal RNA extracts from intrapinnally infected TLR-2/4−/− mice. The presented data represent two independent infection experiments with, respectively, two and four mice per group per time point.
Saliva affects systemic cytokine transcription and translation during infection.
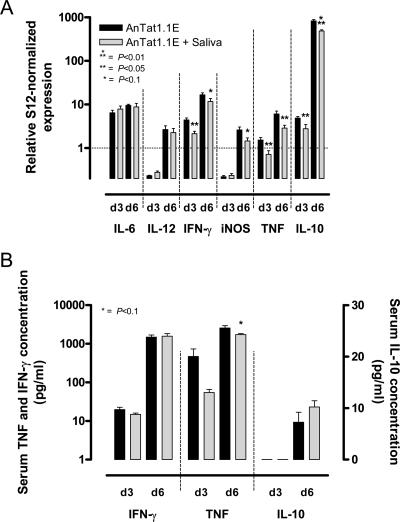
Systemic cytokine responses were analyzed in the blood at the transcriptional and translational levels after 3 and 6 days of infection, corresponding, respectively, to the early and progressed stages of systemic parasitemia (Fig. 1A). Cytokine transcription was assessed using RT-QPCR on RNA extracts from the WBC fraction (Fig. 3A). Several transcripts encoding type I and type II cytokines were significantly upregulated during infection compared to the naive condition. Il-6 and Il-12p35 transcripts, which were suppressed by saliva at the dermal infection site within a few hours of infection (Fig. 2), were not influenced systemically at days 3 and 6 postinfection (p.i.) (Fig. 3A). Although infections initiated with saliva resulted in a significantly more severe parasite burden, systemic transcription of several inflammatory cytokines by WBC was reduced in the early stage of infection. TNF mRNA (days 3 and 6 p.i., P < 0.05) and IL-10 mRNA (day 3 p.i., P < 0.05; day 6 p.i., P < 0.01) levels were lower before the first parasitemia peak upon infection with saliva. Transcripts encoding IFN-γ (day 3 p.i., P < 0.05; day 6 p.i., P < 0.1) and iNOS (day 6 p.i., P < 0.1) also tended to be suppressed.
FIG. 3.
Effect of tsetse fly saliva on the systemic immune response at 3 and 6 days after infection of TLR-2/4−/− mice. (A) Relative S12-normalized IL-6, IL-12, IFN-γ, iNOS, TNF, and IL-10 mRNA levels measured by RT-QPCR in RNA extracts from the white blood cell fraction. (B) Serum IFN-γ, TNF, and IL-10 cytokine concentrations measured by specific capture ELISAs. The presented data are representative of two independent infection experiments with four mice per group per time point.
The reduced TNF mRNA levels upon saliva-facilitated infection were also associated with lower serum TNF concentrations (day 3 p.i., P = 0.17; day 6 p.i., P < 0.1) (Fig. 3B). The transcriptional and translational differences for TNF coincide with the increased early outgrowth of the parasite population. IL-10 and IFN-γ concentrations were not affected in the serum.
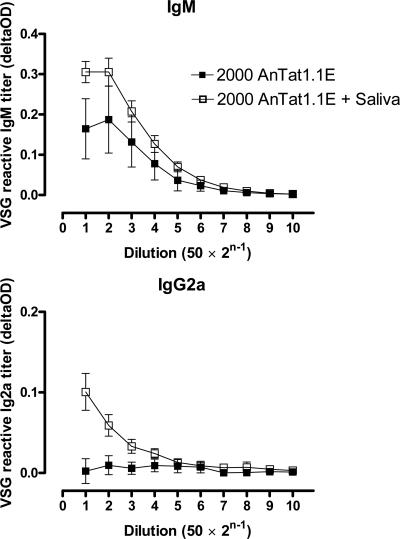
Saliva does not inhibit antitrypanosome antibody titers.
Antibody induction against the major membrane component of the infecting trypanosome clone, AnTat1.1E VSG, was analyzed in the early stage of trypanosome infection with or without tsetse fly saliva. IgM was the only AnTat1.1E sVSG-reactive antibody isotype that was significantly induced in both experimental groups prior to the first peak of parasitemia, as measured in ELISA at day 6 postinfection (Fig. 4). Associated with the higher parasite concentrations observed in the saliva-facilitated infection, an increased anti-sVSG IgM antibody titer was detected for mice where trypanosomes were coinjected with tsetse fly saliva. Moreover, sVSG-reactive IgG2a antibodies could be detected upon coinjection of trypanosomes with saliva, while this antibody isotype was undetectable at day 6 after infection without saliva (Fig. 4).
FIG. 4.
Isotype-specific titration (serial dilutions shown on x axis; dilution = 50 × 2n−1) of AnTat1.1E sVSG-reactive antibodies (IgM and Ig2a) 6 days after intradermal infection of TLR-2/4−/− mice (n = 4) with T. brucei brucei AnTat1.1E in the presence and absence of tsetse fly saliva. deltaOD, background-subtracted optical density.
Repetitive saliva exposure promotes the onset of trypanosome infection.
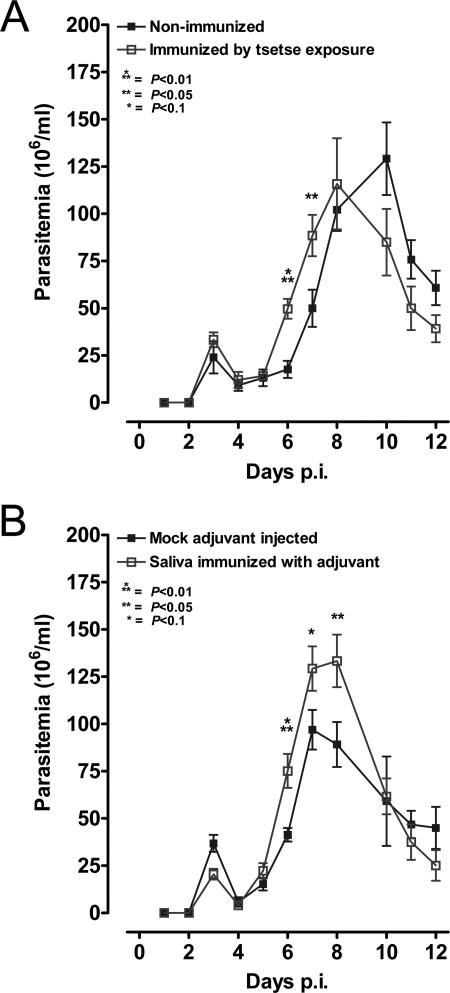
To evaluate the effect of repeated confrontation with saliva and saliva-induced immune responses on the onset of a trypanosome infection, mice were preexposed to repetitive tsetse fly bites. This preexposure resulted in an accelerated onset of a subsequent AnTAR1 infection initiated by the bite of a tsetse fly (day 6 p.i., P < 0.01; day 7 p.i., P < 0.05) (Fig. 5A). Consistent with the natural exposure, experimental immunization of mice against tsetse fly saliva also resulted in a significantly earlier onset of parasitemia upon natural trypanosome challenge in comparison to what was seen for control mice (day 6 p.i., P < 0.01; day 7 p.i., P < 0.1; day 8 p.i., P < 0.05) (Fig. 5B). Immunogenicity of saliva components was analyzed by Western blotting and ELISA, and it was shown that saliva-specific antibodies, including IgE isotypes, were raised upon exposure to saliva as described earlier (4). Post-first peak parasite concentrations in the blood and survival times of infected mice were not different in the different experimental groups.
FIG. 5.
Effect of repetitive exposure to tsetse saliva on the initiation of a tsetse fly-transmitted T. brucei brucei AnTAR1 infection. Shown is parasitemia onset in (BALB/c × C57BL/6)F1 mice confronted with saliva by repeated exposure to tsetse flies (A) and by immunization against saliva in adjuvant (B). The presented data from the two independent settings are the result of single infection experiments with six mice per group.
DISCUSSION
The interaction of African trypanosomes with the host immune system is complex and involves several aspects, such as the antigenic plasticity of the parasite as well as the modulation of immune responses. In order to maintain controlled growth, trypanosomes coordinately alter their major surface antigen (VSG) coat and modify functions of antigen-presenting cells (8, 43) as well as T lymphocytes (56) and B lymphocytes (2). During a trypanosome infection, an equilibrated balance between inflammation and anti-inflammation was shown to be crucial for successfully controlling parasites while limiting the outcome of immune pathology (33, 44). Information on the immunology of African trypanosomiasis is available mainly from experimental trypanosome infections that exclude the vector-host interaction. The presented data demonstrate that tsetse fly salivary components play a significant role in the early infection stage by accelerating the early outgrowth of the trypanosome population. This effect did not result from differences in infectious dose or improved trypanosome viability in a saliva environment. As such, the faster onset of the trypanosome infection could be the result of the interference of tsetse fly saliva with host hemostatic reactions (e.g., vasoconstriction) and host immune reactions, such as the recruitment and activation of host immune cells or the release of inflammatory mediators at the site of infection.
Vasoactive salivary factors, present in several blood-sucking arthropods (40, 52), might be responsible for increasing the parasite's efficiency in invading the lymphatic and blood vessels. In the case of Plasmodium, mosquito-mediated transmission resulted in an increased efficiency of the parasite to leave the dermal infection site compared to an experimental syringe injection (1). Moreover, the Lutzomyia sand fly promotes Leishmania transmission by the presence of the vasodilatory peptide maxadilan, with immune modulatory properties, in the saliva (29, 40, 41). In our study, trypanosome parasites reached earlier detectable levels in the bloodstream in the saliva-coinjected mice, indicating that salivary components might enhance vessel invasion from the dermal infection site.
Since trypanosomes are extracellular parasites, they are in principle more sensitive to antibody-mediated immune effects, including complement-mediated lysis (13, 46) and phagocytosis of opsonized parasites (9, 55). Although the involvement of antibodies in parasite clearance during an early stage of infection might be limited, the influence of tsetse fly saliva-facilitated infection on trypanosome-specific antibody induction was assessed by evaluating the levels of sVSG-specific antibodies in sera of infected mice. The higher parasite burden in the mice coinjected with saliva and trypanosomes is associated with higher titers of AnTat1.1E sVSG-specific IgM and IgG2a antibodies, most probably reflecting the increased confrontation of the host immune system with the trypanosomal VSG rather than a systemic saliva effect. The high VSG-specific antibody titers upon saliva-facilitated infection compared to those of the control infection might explain the equally efficient clearance of the first parasitemia peak despite the more severe parasite burden. Collectively, the infection-accelerating effect of saliva is not dependent on the inhibition of VSG-specific antibody induction.
Modulation of effector functions of APCs is another general feature of several arthropod salivary gland extracts. For instance, ticks and sand flies suppress the production of cytokines, NO, and reactive oxygen intermediates by APCs (26, 45, 59) and thereby might be involved in suppressing antipathogen responses. A major trypanosome component reported to trigger APCs is the VSG, in particular its glycosylphosphatidylinositol anchor. This molecule can trigger inflammatory TNF, IL-6, and IL-12 release from antigen-presenting cells through MyD88-dependent signaling, indicating an interaction with pattern recognition receptors (11). Within 3 hours of intradermal T. brucei brucei infection, local transcription of inflammatory genes was induced at the dermal site. Initiation of infection in the presence of tsetse fly saliva significantly suppressed local transcription of genes encoding IL-6 and IL12p35. Transcripts encoding other inflammatory molecules, such as TNF, IFN-γ, and iNOS, tended to be upregulated in the ear dermis in the early infection stage (1 to 3 h) but were not significantly inhibited by saliva. Systemically, reduced transcription of IFN-γ, TNF, and IL-10 in white blood cells was observed after 3 and 6 days of trypanosome infection initiated with saliva. Additionally, reduced TNF mRNA levels in the WBC compartment were corroborated by altered serum TNF concentrations at days 3 and 6 postinfection as measured by ELISA. As TNF was shown to exert trypanolytic activity for the AnTat1.1 T. brucei stock and to be directly involved in trypanosome control (33), the observed suppression correlates with the increased parasite burden upon saliva-facilitated infection. Together, these data indicate that the infection-promoting effect of tsetse fly saliva is associated with a suppression of local inflammatory responses (IL-6 and IL12p35 mRNA) as well as a systemic effect on TNF production. Here, the systemic effect might result from the direct translation of the local anti-inflammatory action of saliva and, indirectly, from the higher parasite burden or from a combination of both. However, as the affected cytokines are produced mainly by APCs in response to trypanosome antigens, our observations suggest that the saliva-facilitated parasite onset modulates the activation of these cells in the early infection stage.
Besides affecting the responsiveness of APCs to inflammatory trypanosome components, tsetse fly saliva might inhibit APC activation by interfering with inflammatory triggers released upon tissue damage at the dermal site of infection. Based on the molecular identification of salivary components and suggestive functional information, tsetse fly saliva might interfere with ATP-mediated triggering of purinergic receptors on APCs and the subsequent induction of inflammatory cytokines (10). In this context, the enzymatic degradation of extracellular nucleotides has been proposed as a mechanism of anti-inflammation exploited by both endo- and ectoparasites, including blood-sucking arthropods (15, 51). Tsetse fly saliva has been demonstrated to contain components with apyrase (36), putative 5′-nucleotidase (GenBank accession no., AAK63848), and adenosine deaminase (31) activity. With this array of enzymes, saliva could convert a potential inflammatory nucleotide (ATP) to anti-inflammatory degradation products, such as adenosine and inosine (19, 20).
Another important immunological aspect of the vector-host interaction is the occurrence of hypersensitivity reactions at the site of the bite that might result from repetitive exposure to insects. In the case of sand flies, saliva enhances the severity of Leishmania infection, while delayed-type hypersensitivity (DTH) responses, raised by repeated exposure to the vector (22, 57) or immunization against individual salivary components (41, 60), can abrogate the Leishmania infection transmitted by the sand fly. Tsetse fly saliva also promotes the onset of trypanosome infection, while repeated exposure to tsetse fly bites induces saliva-specific IgE antibodies that might be involved in local hypersensitivity reactions (4, 12). Moreover, DTH responses have been observed earlier for tsetse fly-exposed rabbits (12). To evaluate the effect of repeated confrontation with tsetse fly saliva on the onset of a naturally transmitted trypanosome infection, mice were repeatedly exposed to tsetse feeding and immunized against total saliva in adjuvant. Upon challenge with infected tsetse flies, the onset of infection was faster in exposed and saliva-immune mice than in control mice. This indicates that antisaliva immune responses can be beneficial for the initiation of trypanosome infection. This differs from what is seen for Leishmania transmission by the sand fly, where DTH responses against saliva or individual constituents can abrogate the infection (22, 41, 57, 60). However, the intracellular nature of the Leishmania parasite implies that the efficient penetration of APCs becomes a sensitive point in the onset of infection (47, 57), while trypanosomes as extracellular parasites appear unaffected by local hypersensitivity reactions (42) and might even benefit from the increased vasopermeability to leave the initial site of infection more efficiently. This does not exclude the possibility that other exposure schemes or immunization against individual salivary proteins might still result in protection against trypanosome transmission by tsetse flies. However, the presented saliva exposure experiments did not confer protective immunity against natural trypanosome challenge.
Together, the presented data demonstrate that tsetse fly saliva exerts an immune modulatory effect in the murine host associated with an infection-promoting effect during the early stage of a T. brucei brucei infection. Moreover, repeated exposure to saliva can make mice more sensitive to infection in the early stage. Evaluation of the possible epidemiological importance of both effects would depend on an extensive experimental assessment of the minimal infective dose as a crucial parameter.
Acknowledgments
This project was supported by funding from the VUB (Vrije Universiteit Brussel) and an IWT (Instituut voor de aanmoediging van innovatie door wetenschap en technologie in Vlaanderen) PhD grant (IWT1149). S.M. is an NFWO postdoctoral research fellow. The work was performed within the frame of an interuniversity attraction pole (IUAP) program with the partnership of the Prins Leopold Institute of Tropical Medicine (ITM).
This work was supported by the kind technical assistance of Ella Omasta, Jos Van Hees, and Marie-Thérèse Detobel.
Editor: W. A. Petri, Jr.
Footnotes
Published ahead of print on 5 September 2006.
REFERENCES
- 1.Amino, R., S. Thiberge, B. Martin, S. Celli, S. Shorte, F. Frischknecht, and R. Menard. 2006. Quantitative imaging of Plasmodium transmission from mosquito to mammal. Nat. Med. 12:220-224. [DOI] [PubMed] [Google Scholar]
- 2.Assoku, R. K., I. R. Tizard, and K. H. Neilsen. 1977. Free fatty acids, complement activation, and polyclonal B-cell stimulation as factors in the immunopathogenesis of African trypanosomiasis. Lancet 2:956-959. [DOI] [PubMed] [Google Scholar]
- 3.Belkaid, Y., S. Kamhawi, G. Modi, J. Valenzuela, N. Noben-Trauth, E. Rowton, J. Ribeiro, and D. L. Sacks. 1998. Development of a natural model of cutaneous leishmaniasis: powerful effects of vector saliva and saliva preexposure on the long-term outcome of Leishmania major infection in the mouse ear dermis. J. Exp. Med. 188:1941-1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caljon, G., J. Van Den Abbeele, J. M. Sternberg, M. Coosemans, P. De Baetselier, and S. Magez. 2006. Tsetse fly saliva biases the immune response to Th2 and induces anti-vector antibodies that are a useful tool for exposure assessment. Int. J. Parasitol. 36:1025-1035. [DOI] [PubMed] [Google Scholar]
- 5.Cavassani, K. A., J. C. Aliberti, A. R. Dias, J. S. Silva, and B. R. Ferreira. 2005. Tick saliva inhibits differentiation, maturation and function of murine bone-marrow-derived dendritic cells. Immunology 114:235-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cross, G. A. 1990. Cellular and genetic aspects of antigenic variation in trypanosomes. Annu. Rev. Immunol. 8:83-110. [DOI] [PubMed] [Google Scholar]
- 7.Cross, G. A. 1975. Identification, purification and properties of clone-specific glycoprotein antigens constituting the surface coat of Trypanosoma brucei. Parasitology 71:393-417. [DOI] [PubMed] [Google Scholar]
- 8.Darji, A., A. Beschin, M. Sileghem, H. Heremans, L. Brys, and P. De Baetselier. 1996. In vitro simulation of immunosuppression caused by Trypanosoma brucei: active involvement of gamma interferon and tumor necrosis factor in the pathway of suppression. Infect. Immun. 64:1937-1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dempsey, W. L., and J. M. Mansfield. 1983. Lymphocyte function in experimental African trypanosomiasis. V. Role of antibody and the mononuclear phagocyte system in variant-specific immunity. J. Immunol. 130:405-411. [PubMed] [Google Scholar]
- 10.Di Virgilio, F., P. Chiozzi, D. Ferrari, S. Falzoni, J. M. Sanz, A. Morelli, M. Torboli, G. Bolognesi, and O. R. Baricordi. 2001. Nucleotide receptors: an emerging family of regulatory molecules in blood cells. Blood 97:587-600. [DOI] [PubMed] [Google Scholar]
- 11.Drennan, M. B., B. Stijlemans, J. Van den Abbeele, V. J. Quesniaux, M. Barkhuizen, F. Brombacher, P. De Baetselier, B. Ryffel, and S. Magez. 2005. The induction of a type 1 immune response following a Trypanosoma brucei infection is MyD88 dependent. J. Immunol. 175:2501-2509. [DOI] [PubMed] [Google Scholar]
- 12.Ellis, J. A., S. Z. Shapiro, O. ole Moi-Yoi, and S. K. Moloo. 1986. Lesions and saliva-specific antibody responses in rabbits with immediate and delayed hypersensitivity reactions to the bites of Glossina morsitans centralis. Vet. Pathol. 23:661-667. [DOI] [PubMed] [Google Scholar]
- 13.Flemmings, B., and C. Diggs. 1978. Antibody-dependent cytotoxicity against Trypanosoma rhodesiense mediated through an alternative complement pathway. Infect. Immun. 19:928-933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ghassabeh, G. H., P. De Baetselier, L. Brys, W. Noel, J. A. Van Ginderachter, S. Meerschaut, A. Beschin, F. Brombacher, and G. Raes. 2006. Identification of a common gene signature for type II cytokine-associated myeloid cells elicited in vivo in different pathologic conditions. Blood 108:575-583. [DOI] [PubMed] [Google Scholar]
- 15.Gounaris, K., and M. E. Selkirk. 2005. Parasite nucleotide-metabolizing enzymes and host purinergic signalling. Trends Parasitol. 21:17-21. [DOI] [PubMed] [Google Scholar]
- 16.Hall, L. R., and R. G. Titus. 1995. Sand fly vector saliva selectively modulates macrophage functions that inhibit killing of Leishmania major and nitric oxide production. J. Immunol. 155:3501-3506. [PubMed] [Google Scholar]
- 17.Hannier, S., J. Liversidge, J. M. Sternberg, and A. S. Bowman. 2004. Characterization of the B-cell inhibitory protein factor in Ixodes ricinus tick saliva: a potential role in enhanced Borrelia burgdoferi [sic] transmission. Immunology 113:401-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hannier, S., J. Liversidge, J. M. Sternberg, and A. S. Bowman. 2003. Ixodes ricinus tick salivary gland extract inhibits IL-10 secretion and CD69 expression by mitogen-stimulated murine splenocytes and induces hyporesponsiveness in B lymphocytes. Parasite Immunol. 25:27-37. [DOI] [PubMed] [Google Scholar]
- 19.Hardart, G. E., G. W. Sullivan, H. T. Carper, and G. L. Mandell. 1991. Adenosine and 2-phenylaminoadenosine (CV-1808) inhibit human neutrophil bactericidal function. Infect. Immun. 59:885-889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hasko, G., D. G. Kuhel, Z. H. Nemeth, J. G. Mabley, R. F. Stachlewitz, L. Virag, Z. Lohinai, G. J. Southan, A. L. Salzman, and C. Szabo. 2000. Inosine inhibits inflammatory cytokine production by a posttranscriptional mechanism and protects against endotoxin-induced shock. J. Immunol. 164:1013-1019. [DOI] [PubMed] [Google Scholar]
- 21.Hertz, C. J., H. Filutowicz, and J. M. Mansfield. 1998. Resistance to the African trypanosomes is IFN-gamma dependent. J. Immunol. 161:6775-6783. [PubMed] [Google Scholar]
- 22.Kamhawi, S., Y. Belkaid, G. Modi, E. Rowton, and D. Sacks. 2000. Protection against cutaneous leishmaniasis resulting from bites of uninfected sand flies. Science 290:1351-1354. [DOI] [PubMed] [Google Scholar]
- 23.Kopecky, J., M. Kuthejlova, and J. Pechova. 1999. Salivary gland extract from Ixodes ricinus ticks inhibits production of interferon-gamma by the upregulation of interleukin-10. Parasite Immunol. 21:351-356. [DOI] [PubMed] [Google Scholar]
- 24.Kovar, L., J. Kopecky, and B. Rihova. 2001. Salivary gland extract from Ixodes ricinus tick polarizes the cytokine profile toward Th2 and suppresses proliferation of T lymphocytes in human PBMC culture. J. Parasitol. 87:1342-1348. [DOI] [PubMed] [Google Scholar]
- 25.Kubes, M., P. Kocakova, M. Slovak, M. Slavikova, N. Fuchsberger, and P. A. Nuttall. 2002. Heterogeneity in the effect of different ixodid tick species on human natural killer cell activity. Parasite Immunol. 24:23-28. [DOI] [PubMed] [Google Scholar]
- 26.Kuthejlova, M., J. Kopecky, G. Stepanova, and A. Macela. 2001. Tick salivary gland extract inhibits killing of Borrelia afzelii spirochetes by mouse macrophages. Infect. Immun. 69:575-578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lanham, S. M., and D. G. Godfrey. 1970. Isolation of salivarian trypanosomes from man and other mammals using DEAE-cellulose. Exp. Parasitol. 28:521-534. [DOI] [PubMed] [Google Scholar]
- 28.Leboulle, G., M. Crippa, Y. Decrem, N. Mejri, M. Brossard, A. Bollen, and E. Godfroid. 2002. Characterization of a novel salivary immunosuppressive protein from Ixodes ricinus ticks. J. Biol. Chem. 277:10083-10089. [DOI] [PubMed] [Google Scholar]
- 29.Lerner, E. A., and C. B. Shoemaker. 1992. Maxadilan. Cloning and functional expression of the gene encoding this potent vasodilator peptide. J. Biol. Chem. 267:1062-1066. [PubMed] [Google Scholar]
- 30.Levine, R. F., and J. M. Mansfield. 1984. Genetics of resistance to the African trypanosomes. III. Variant-specific antibody responses of H-2-compatible resistant and susceptible mice. J. Immunol. 133:1564-1569. [PubMed] [Google Scholar]
- 31.Li, S., and S. Aksoy. 2000. A family of genes with growth factor and adenosine deaminase similarity are preferentially expressed in the salivary glands of Glossina m. morsitans. Gene 252:83-93. [DOI] [PubMed] [Google Scholar]
- 32.Lima, H. C., and R. G. Titus. 1996. Effects of sand fly vector saliva on development of cutaneous lesions and the immune response to Leishmania braziliensis in BALB/c mice. Infect. Immun. 64:5442-5445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Magez, S., M. Radwanska, A. Beschin, K. Sekikawa, and P. De Baetselier. 1999. Tumor necrosis factor alpha is a key mediator in the regulation of experimental Trypanosoma brucei infections. Infect. Immun. 67:3128-3132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Magez, S., B. Stijlemans, G. Caljon, H. P. Eugster, and P. De Baetselier. 2002. Control of experimental Trypanosoma brucei infections occurs independently of lymphotoxin-alpha induction. Infect. Immun. 70:1342-1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Magez, S., B. Stijlemans, M. Radwanska, E. Pays, M. A. Ferguson, and P. De Baetselier. 1998. The glycosyl-inositol-phosphate and dimyristoylglycerol moieties of the glycosylphosphatidylinositol anchor of the trypanosome variant-specific surface glycoprotein are distinct macrophage-activating factors. J. Immunol. 160:1949-1956. [PubMed] [Google Scholar]
- 36.Mant, M. J., and K. R. Parker. 1981. Two platelet aggregation inhibitors in tsetse (Glossina) saliva with studies of roles of thrombin and citrate in in vitro platelet aggregation. Br. J. Haematol. 48:601-608. [DOI] [PubMed] [Google Scholar]
- 37.Mbow, M. L., J. A. Bleyenberg, L. R. Hall, and R. G. Titus. 1998. Phlebotomus papatasi sand fly salivary gland lysate down-regulates a Th1, but up-regulates a Th2, response in mice infected with Leishmania major. J. Immunol. 161:5571-5577. [PubMed] [Google Scholar]
- 38.Mejri, N., N. Franscini, B. Rutti, and M. Brossard. 2001. Th2 polarization of the immune response of BALB/c mice to Ixodes ricinus instars, importance of several antigens in activation of specific Th2 subpopulations. Parasite Immunol. 23:61-69. [DOI] [PubMed] [Google Scholar]
- 39.Montgomery, R. R., D. Lusitani, A. De Boisfleury Chevance, and S. E. Malawista. 2004. Tick saliva reduces adherence and area of human neutrophils. Infect. Immun. 72:2989-2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moro, O., and E. A. Lerner. 1997. Maxadilan, the vasodilator from sand flies, is a specific pituitary adenylate cyclase activating peptide type I receptor agonist. J. Biol. Chem. 272:966-970. [DOI] [PubMed] [Google Scholar]
- 41.Morris, R. V., C. B. Shoemaker, J. R. David, G. C. Lanzaro, and R. G. Titus. 2001. Sandfly maxadilan exacerbates infection with Leishmania major and vaccinating against it protects against L. major infection. J. Immunol. 167:5226-5230. [DOI] [PubMed] [Google Scholar]
- 42.Naessens, J., D. M. Mwangi, J. Buza, and S. K. Moloo. 2003. Local skin reaction (chancre) induced following inoculation of metacyclic trypanosomes in cattle by tsetse flies is dependent on CD4 T lymphocytes. Parasite Immunol. 25:413-419. [DOI] [PubMed] [Google Scholar]
- 43.Namangala, B., L. Brys, S. Magez, P. De Baetselier, and A. Beschin. 2000. Trypanosoma brucei brucei infection impairs MHC class II antigen presentation capacity of macrophages. Parasite Immunol. 22:361-370. [DOI] [PubMed] [Google Scholar]
- 44.Namangala, B., W. Noel, P. De Baetselier, L. Brys, and A. Beschin. 2001. Relative contribution of interferon-gamma and interleukin-10 to resistance to murine African trypanosomosis. J. Infect. Dis. 183:1794-1800. [DOI] [PubMed] [Google Scholar]
- 45.Norsworthy, N. B., J. Sun, D. Elnaiem, G. Lanzaro, and L. Soong. 2004. Sand fly saliva enhances Leishmania amazonensis infection by modulating interleukin-10 production. Infect. Immun. 72:1240-1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Otesile, E. B., M. Lee, and H. Tabel. 1991. Plasma levels of proteins of the alternative complement pathway in inbred mice that differ in resistance to Trypanosoma congolense infections. J. Parasitol. 77:958-964. [PubMed] [Google Scholar]
- 47.Puri, A., S. Y. Rizvi, W. Haq, P. Y. Guru, B. Kundu, R. P. Saxena, R. Shukla, K. B. Mathur, and K. C. Saxena. 1993. Immunostimulant activity of a novel lipopeptide and its protective action against Leishmania donovani. Immunopharmacol. Immunotoxicol. 15:539-556. [DOI] [PubMed] [Google Scholar]
- 48.Raes, G., L. Brys, B. K. Dahal, J. Brandt, J. Grooten, F. Brombacher, G. Vanham, W. Noel, P. Bogaert, T. Boonefaes, A. Kindt, R. Van den Bergh, P. J. Leenen, P. De Baetselier, and G. H. Ghassabeh. 2005. Macrophage galactose-type C-type lectins as novel markers for alternatively activated macrophages elicited by parasitic infections and allergic airway inflammation. J. Leukoc. Biol. 77:321-327. [DOI] [PubMed] [Google Scholar]
- 49.Raes, G., P. De Baetselier, W. Noel, A. Beschin, F. Brombacher, and G. Hassanzadeh Gh. 2002. Differential expression of FIZZ1 and Ym1 in alternatively versus classically activated macrophages. J. Leukoc Biol. 71:597-602. [PubMed] [Google Scholar]
- 50.Ramamoorthi, N., S. Narasimhan, U. Pal, F. Bao, X. F. Yang, D. Fish, J. Anguita, M. V. Norgard, F. S. Kantor, J. F. Anderson, R. A. Koski, and E. Fikrig. 2005. The Lyme disease agent exploits a tick protein to infect the mammalian host. Nature 436:573-577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ribeiro, J. M., and I. M. Francischetti. 2003. Role of arthropod saliva in blood feeding: sialome and post-sialome perspectives. Annu. Rev. Entomol. 48:73-88. [DOI] [PubMed] [Google Scholar]
- 52.Ribeiro, J. M., R. H. Nussenzveig, and G. Tortorella. 1994. Salivary vasodilators of Aedes triseriatus and Anopheles gambiae (Diptera: Culicidae). J. Med. Entomol. 31:747-753. [DOI] [PubMed] [Google Scholar]
- 53.Ribeiro, J. M., J. J. Weis, and S. R. Telford III. 1990. Saliva of the tick Ixodes dammini inhibits neutrophil function. Exp. Parasitol. 70:382-388. [DOI] [PubMed] [Google Scholar]
- 54.Schneider, B. S., L. Soong, N. S. Zeidner, and S. Higgs. 2004. Aedes aegypti salivary gland extracts modulate anti-viral and TH1/TH2 cytokine responses to Sindbis virus infection. Viral Immunol. 17:565-573. [DOI] [PubMed] [Google Scholar]
- 55.Shi, M., G. Wei, W. Pan, and H. Tabel. 2004. Trypanosoma congolense infections: antibody-mediated phagocytosis by Kupffer cells. J. Leukoc. Biol. 76:399-405. [DOI] [PubMed] [Google Scholar]
- 56.Sileghem, M., R. Hamers, and P. De Baetselier. 1987. Experimental Trypanosoma brucei infections selectively suppress both interleukin 2 production and interleukin 2 receptor expression. Eur. J. Immunol. 17:1417-1421. [DOI] [PubMed] [Google Scholar]
- 57.Thiakaki, M., I. Rohousova, V. Volfova, P. Volf, K. P. Chang, and K. Soteriadou. 2005. Sand fly specificity of saliva-mediated protective immunity in Leishmania amazonensis-BALB/c mouse model. Microbes Infect. 7:760-766. [DOI] [PubMed] [Google Scholar]
- 58.Titus, R. G., and J. M. Ribeiro. 1988. Salivary gland lysates from the sand fly Lutzomyia longipalpis enhance Leishmania infectivity. Science 239:1306-1308. [DOI] [PubMed] [Google Scholar]
- 59.Urioste, S., L. R. Hall, S. R. Telford III, and R. G. Titus. 1994. Saliva of the Lyme disease vector, Ixodes dammini, blocks cell activation by a nonprostaglandin E2-dependent mechanism. J. Exp. Med. 180:1077-1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Valenzuela, J. G., Y. Belkaid, M. K. Garfield, S. Mendez, S. Kamhawi, E. D. Rowton, D. L. Sacks, and J. M. Ribeiro. 2001. Toward a defined anti-Leishmania vaccine targeting vector antigens: characterization of a protective salivary protein. J. Exp. Med. 194:331-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Van Ginderachter, J. A., S. Meerschaut, Y. Liu, L. Brys, K. De Groeve, G. Hassanzadeh Ghassabeh, G. Raes, and P. De Baetselier. 2006. Peroxisome proliferator-activated receptor γ (PPARγ) ligands reverse CTL suppression by alternatively activated (M2) macrophages in cancer. Blood 108:525-535. [DOI] [PubMed] [Google Scholar]
- 62.Vickerman, K., L. Tetley, K. A. Hendry, and C. M. Turner. 1988. Biology of African trypanosomes in the tsetse fly. Biol. Cell 64:109-119. [DOI] [PubMed] [Google Scholar]