Abstract
Complementary and alternative medicine is used by many cancer patients in most parts of the world, and its use is increasing. The aim of the present study was to examine, over 5 years, the perceived quality of life/life satisfaction in two samples of women with breast cancer who were treated with anthroposophic care or conventional medical treatment only. Data from admission, after 1 year and after 5 years are used for the comparisons. On admission to the study the women in anthroposophic care perceived their quality of life to be lower than that of the women in the conventional treatment group, especially for emotional, cognitive and social functioning and overall quality of life. Sixty women who actively chose treatment with anthroposophic medicine and 60 individually matched women treated with conventional medicine participated. Quality of life was measured by the EORTC QLQ-C30 and the Life Satisfaction Questionnaire. Twenty-six women within anthroposophic care and 31 women within conventional medicine survived the 5 years. Effect size (ES) estimation favored the anthroposophic group in seven of the subscales mostly measuring emotional functioning. The ES for four of the subscales favored the conventional treatment group, mostly concerning physical functioning. After 5 years there were improvements in overall quality of life and in emotional and social functioning compared to admission for the women in anthroposophic care. The improvements took place between admission and 1 year, but not further on. Only minor improvements were found in the matching group.
Keywords: complementary and alternative medicine, EORTC QLQ-C30, Life Satisfaction Questionnaire
Introduction
The Use of Complementary and Alternative Medicine
Complementary and alternative medicine (CAM) is used by many cancer patients in most parts of the world, and its use is increasing (1). Eisenberg et al. (2) found in a national survey of the use of alternative therapies in 1997 in the USA, that the range of use varied between 32 and 54% in different sociodemographic groups and that the use had increased 45% between 1990 and 1997. A cross-sectional study in Europe of 956 cancer patients in 14 countries showed that ∼36% had used CAM (3). Studies show that people who choose CAM differ from those who choose conventional medicine. A review of the literature show that CAM users tend to be better educated, of higher socioeconomic status, female and younger than non-users (4,5). Studies also show that seeking alternative treatment is more common among mentally distressed cancer patients (6,7).
A multicenter study from Norway showed survival data for a follow-up of 8 years for 515 cancer patients. The survival rate was lower for users of alternative medicine (AM), 21%, compared with non-users, 35%. The authors concluded that AM use may predict a shorter survival (8).
Anthroposophic Care in Sweden
In Sweden there is one anthroposophic hospital situated in the county of Stockholm. It has 74 beds and ∼3000 out-patients yearly. About 40% of the patients suffer from cancer (9). The patients actively seek this form of care themselves, but the fee is most often provided by the county council.
In anthroposophic medicine, natural scientific methods used in conventional medicine are not contraindicated. In order to reach true healing, however, the patient must be given the opportunity to mature through the complementary use of anthroposophic therapies. The term ‘complementary’ signifies that conventional therapy can be part of the treatment (10).
The Present Study
The present study is part of a major clinical study of the outcome of anthroposophic medicine, for women with breast cancer. By matching procedures, women with breast cancer not receiving complementary care are also studied, as is the relationship between different outcome measurements (11). The following outcome measures were used in the main study: (i) the perceived quality of life/life satisfaction and coping measured by questionnaires and tape-recorded interviews; (ii) medical investigation; and (iii) an immunological test package. The patients have been followed for 5 years. The design was based on prestudies performed in 1988–1994 (9).
The subjects in the major clinical study were women diagnosed with breast cancer that chose the anthroposophic hospital for treatment and individually matched women with breast cancer treated with conventional medicine only. A power analysis was performed on the basis of quality of life measurements in an earlier study where the Life Satisfaction Questionnaire (LSQ) was developed. In that study, 362 women with breast cancer filled out the EORTC QLQ-C30 and the LSQ (12). A sample size of 60 in each group was required to detect a difference of 0.5 SD with a power of 0.80. A difference of 0.5 SD for overall quality of life was considered big enough to give relevant information according to Anthony (13).
The results of the comparison between the two groups on admission and at the 1 year follow-up have been presented elsewhere (14,15). On admission to the study the women who choose anthroposophic care perceived their quality of life to be lower than that of the women in the conventional treatment group, especially for emotional, cognitive and social functioning and overall quality of life (14). The results from the 1 year follow-up showed that 36 matched pairs took part on all measurement occasions, and the patients choosing anthroposophic care showed increased quality of life/life satisfaction than those who received conventional treatment only in the scales/factors measuring physical, emotional, cognitive, social functioning and quality of daily activities and also less problem with sleep and appetite after 1 year compared with admission to the study (15).
The Aim of the Study
The aim of the present study was to examine, over 5 years, the perceived quality of life/life satisfaction in two samples of women with breast cancer who were treated with anthroposophic care or conventional medical treatment only. Data from admission, after 1 year and after 5 years are used for the comparisons.
Methods
Design and Participants
The subjects were women diagnosed with breast cancer who chose the anthroposophic hospital for treatment. Sixty women who met the inclusion criteria, i.e. 75 years old, or younger, residing in Stockholm, being able to communicate in Swedish, and expected to live for at least 6 months, were admitted from November 1995 to January 1999. In all, 68 women were invited to participate. Each woman was individually matched with a woman from an oncology out-patient department in the southern Stockholm area who received conventional medical cancer treatment. A total of 120 women were included. The matching criteria were based on the following principles: (i) stage of disease at entry—advanced inoperable tumor or distant metastases (n = 42 + 42) or operable tumors with or without node metastases (n = 18 + 18); (ii) age—over 50 years (n = 20 + 20) or 50 years or younger (n = 40 + 40); (iii) treatment during the 3 months before entering the study—radiotherapy or chemotherapy (n = 41 + 41) or no treatment (n = 19 + 19); and (iv) prognosis—favorable prognosis (35 + 35) or unfavorable (n = 25 + 25). Prognosis was related to the frequency and location of metastases. Prognosis was only applied as a matching variable in cases with metastatic disease. The groups were called ABCW (women with breast cancer in anthroposophic care) and CBCW (women with breast cancer in conventional care).
The women were between 28 and 75 years of age (M = 49.2, SD = 9.1) on entering the study (M = 49.4, SD = 9.7, range = 28–75 and M = 49.1, SD = 8.5, range = 29–70, respectively. Sixty-seven percent (n = 40) of the women who chose anthroposophic care (ABCW) and 78% (n = 47) in the other group (CBCW) were married or lived with a partner, and 75% (n = 45, ABCW) and 85% (n = 51, CBCW) had children. Time between diagnosis and admission to the study varied between 1 and 128 months for the women choosing anthroposophic care (M = 32.57, SD = 31.6) and between 1 and 238 months for the women in conventional treatment (M = 36.92, SD = 45.3). There was no significant difference between the two groups in these respects. Table 1 shows the frequency of women in the two groups who took part on the different occasions. Eight women dropped out of the study in the ABCW, but at the 5 year follow-up, three of those women had died leaving five dropouts. In the CBCW, eight women dropped out of the study. One reason the women gave for declining to further participate after inclusion was that they felt it was too demanding to be interviewed and fill out questionnaires several times. Progressions of the disease or other medical problems were other reasons. Furthermore, some women did not reply to the invitation to take part in the 6 month, 1 year or 5 year follow-up.
Table 1.
The frequency of women who answered the EORTC QLQ-C30 and the LSQ on different occasions in ABCW and CBCW
| Occasion | ABCW | CBCW | Matched pairs | ||||
|---|---|---|---|---|---|---|---|
| Participants | Deceased† | Dropouts | Participants | Deceased | Dropouts | ||
| Admission | 60 | 60 | 60 | ||||
| After 4 weeks | 53 | 1 | 6 | 58 | 2 | 52 | |
| After 3 months | 51 | 3 | 6 | 55 | 3 | 2 | 48 |
| After 6 months | 48 | 6 | 6 | 53 | 5 | 2 | 44 |
| After 1 year | 41 | 11 | 8 | 47 | 9 | 4 | 36 |
| After 5 years | 21 | 34 | 5‡ | 23 | 29 | 8 | 13 |
ABCW, women with breast cancer in anthroposophic care; CBCW, women with breast cancer in conventional care.
†Cumulative frequency.
‡Three of the eight women who were dropouts during the first year died before the 5 year follow-up.
Measures
The EORTC QLQ-C30
This consists of 30 items expressed in six functional scales (PF, physical functioning; RF, role functioning; EF, emotional functioning; CF, cognitive functioning; SF, social functioning; and QL, global quality of life) and nine symptom scales (FA, fatigue; NV, nausea and vomiting; PA, pain; DY, dyspnea; SL, sleep disturbance; AP, appetite loss; CO, constipation; DI, diarrhea; and FI, financial impact). In the present study, the Swedish edition of version 1.0 of the instrument was used (16). The scores on the functional scales are linearly transformed such that all scales range from 0 to 100, with a higher score representing a higher level of functioning. The symptoms scale items are also linearly transformed such that all scales/items range from 0 to 100. Higher scores represent a higher level of symptomatology/problems (16).
The LSQ
The LSQ consists of 34 items on 7-point scales. Examples: ‘How much have you been troubled by tiredness during the past week?’ Responses range from ‘1’, very much, to ‘7’, not at all. Scale point 7 represents the highest quality in all items. The 34 items are allocated to six different factors as follows: physical symptoms (PS), sickness impact (SI), quality of daily activities (QDA), socioeconomic situation (SES), quality of family relation (QFA) and quality of close friend relationship (QFR). The scores for each factor are calculated as follows: the raw scores of the items are summarized, divided by the highest point in the scale and multiplied by 100. Thus, 100 represents the maximum quality in each factor. The total quality of life/life satisfaction is calculated in the same way (17,18).
Interventions
Both groups had been treated according to a special regional care program for all patients belonging to the Stockholm/Gotland region (19). The women who chose anthroposophic care were additionally treated with a special care program during their stay at the anthroposophic hospital (mean value 14.3 days, range 5–29 days). The individually composed anthroposophic therapies consisted of holistic care including natural products, Iscador, diets, art therapy, rhythmic therapy, therapeutic massage and hydrotherapy (10). The anthroposophic hospital, built in 1985, is small with 74 beds. The hospital is situated in the countryside outside of Stockholm. The caring environment is by many patients considered as peaceful, ‘almost like a monastery or a retreat’. Television and radio are not available and phones are advised to be used sparsely. The aim of caring is to find rest and peace and good encounters with self and others, caring personnel as well as fellow patients. Bodily therapies, art therapies, anthroposophic and conventional medicines are individually prescribed by the responsible physician. The caring personnel consist of registered nurses and therapists specially trained in anthroposophic medicine and care.
Procedure
The women were followed for 5 years and were assessed by the questionnaires on six occasions as follows: on admission, after 1 month, after 3 months, after 6 months, after 1 year and after 5 years. Data from admission, after 1 year and after 5 years are used in the present study.
Data Analysis
Analysis of variance (ANOVA) for repeated measure within each group was used to identify significant differences, Bonferroni correction was used for the post-tests in order to control for mass significance. Effect size (ES) was used for comparisons between groups. A value close to 1 indicates that all variability is attributable to the difference between the matched pairs, whereas a value close to 0 indicates that little of the variability is explained (20). According to Cohen (21), an ES >0.20 should be considered small, an ES between 0.50 and 0.80 moderate, and an ES >0.80 large. SPSS version 11.0 was used for the statistical procedures.
Ethical Considerations
The main project had been approved after ethical investigation by the Regional Research Ethics Committee at the Karolinska Institute, Stockholm, in 1995 and 2001.
Results
Survival
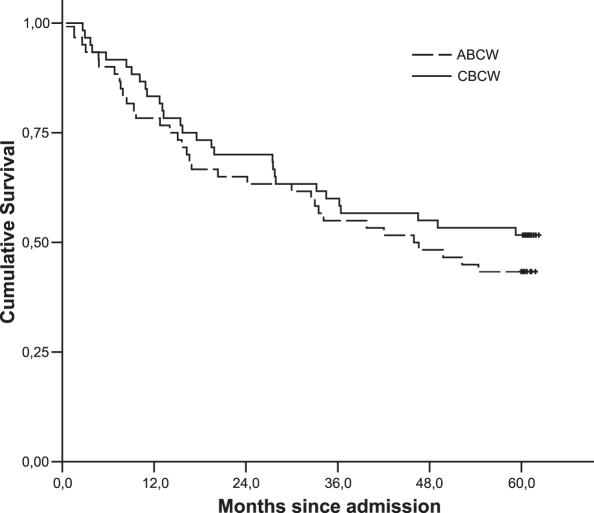
Twenty-six (43%) of the women who chose anthroposophic care and 31 (52%) of the women in the other group survived the data collection period. This difference is not statistically significant (Wilcoxon's signed rank test, Z = −1.508, P = 0.132). The cumulative survival is shown in Fig. 1.
Figure 1.
Cumulative survival during 5 years for ABCW and CBCW, respectively.
Time since diagnosis varied in both groups (range 1–128 months in ABCW and 1–238 months in CBCW). It means that survival time since diagnosis varied a lot in both groups. To use time since diagnosis as a covariate did not change the result. There was no statistically significant difference in survival between the two groups after 5 years (P = 0.134).
Quality of Life Over Time
On admission there were significant differences between the two groups (n = 60 + 60) in several of the scales of EORTC QLQ-30 (RF, EF, CF, SF, QL, FA, PA and FI) and in some of the factors of the LSQ (PS, SI, SES and TotQoL) (14).
ABCW
Changes over time calculated with the help of ANOVAs showed some significant changes within the ABCW (n = 21). In the EORTC QLQ-C30 there were significant improvements in four of the functional scales (EF, CF, SF and QL) and in four of the symptoms scales (FA, NV, PA and DY) (see Tables 2 and 3). Most improvements were seen between admission and 1 year, but not further on. In the LSQ there were significant improvements in four of the factors and in the total scale (PS, SI, QDA, SES and TotQL) (see Table 4). The improvements were seen between admission and 1 year but not further on.
Table 2.
The means, standard deviations, F and P-values (Wilks lambda and Bonferroni correction) for the scales of the EORTC QLQ-C30, functional scales, for admission, after 1 year and after 5 years
| Scale | ABCW (n = 21) | CBCW (n = 23) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Admission | 1 year | 5 years | Admission | 1 year | 5 years | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| PF | 80.00 | 22.8 | 84.26 | 15.7 | 78.10 | 26.8 | 80.87 | 19.5 | 84.33 | 15.9 | 80.00 | 19.1 |
| RF | 59.53 | 34.0 | 71.43 | 29.9 | 66.67 | 32.9 | 76.09 | 25.3 | 73.91 | 29.7 | 65.22 | 38.2 |
| EF | 54.76 | 18.7 | 73.41 | 16.6 | 67.10 | 19.9 | 72.83 | 25.5 | 66.39 | 30.1 | 72.46 | 27.1 |
| CF | 66.67 | 26.4 | 84.13 | 14.4 | 80.16 | 22.1 | 76.09 | 26.5 | 73.23 | 28.7 | 78.26 | 24.3 |
| SF | 61.11 | 28.1 | 83.33 | 21.7 | 78.57 | 28.5 | 80.43 | 21.1 | 73.26 | 29.2 | 80.43 | 30.4 |
| QL | 46.43 | 20.7 | 66.65 | 15.8 | 67.86 | 19.1 | 61.23 | 28.0 | 60.19 | 29.17 | 69.20 | 24.5 |
| Scale | F | P | Significance* | F | P | Significance* | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PF | 2.083 | 0.152 | n.s. | 0.892 | 0.078 | n.s. | ||||||
| RF | 1.160 | 0.335 | n.s. | 1.220 | 0.104 | n.s. | ||||||
| EF | 14.670 | 1<0.001 | 1–2** | 11.522 | 10.241 | n.s. | ||||||
| CF | 7.099 | 0.005 | 1–2, 1–3*** | 0.447 | 0.645 | n.s. | ||||||
| SF | 7.140 | 0.005 | 1–2 | 1.022 | 0.377 | n.s. | ||||||
| QL | 16.553 | 1<0.001 | 1–2, 1–3 | 11.612 | 10.223 | n.s. | ||||||
ABCW, women with breast cancer in anthroposophic care; CBCW, women with breast cancer in conventional care.
*P < 0.05 for significant difference; **1–2 = admission versus 1 year; ***1–3 = admission versus 5 years.
Table 3.
The means, standard deviations, F and P-values (Wilks lambda and Bonferroni correction) for the scales of the EORTC QLQ-C30, symptom scales, for admission, after 1 year and after 5 years
| Scale | ABCW (n = 21) | CBCW (n = 23) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Admission | 1 year | 5 years | Admission | 1 year | 5 years | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| FA | 55.56 | 23.6 | 33.86 | 20.0 | 40.74 | 28.8 | 35.27 | 23.4 | 40.10 | 30.7 | 30.43 | 26.0 |
| NV | 13.49 | 20.2 | 7.14 | 16.3 | 1.59 | 5.0 | 6.52 | 17.2 | 9.42 | 20.0 | 3.62 | 7.0 |
| PA | 39.68 | 29.1 | 17.46 | 18.6 | 22.22 | 27.0 | 25.36 | 29.7 | 24.68 | 29.3 | 23.19 | 33.2 |
| DY | 28.57 | 30.3 | 28.57 | 26.4 | 26.90 | 32.7 | 30.43 | 28.3 | 30.43 | 31.6 | 20.13 | 19.3 |
| SL | 41.27 | 27.7 | 26.98 | 27.1 | 38.10 | 32.1 | 28.79 | 36.1 | 31.86 | 31.7 | 30.30 | 35.5 |
| AP | 14.29 | 27.0 | 3.17 | 10.0 | 4.76 | 12.0 | 4.35 | 11.5 | 11.60 | 21.6 | 0.00 | 0.0 |
| CO | 22.22 | 28.5 | 15.87 | 22.7 | 17.46 | 25.0 | 10.14 | 23.4 | 5.80 | 16.4 | 8.70 | 15.0 |
| DI | 7.94 | 14.5 | 1.59 | 7.3 | 11.67 | 19.1 | 5.80 | 16.4 | 10.14 | 21.2 | 10.14 | 25.5 |
| FI | 42.86 | 46.1 | 36.51 | 40.7 | 28.57 | 33.8 | 18.84 | 22.1 | 17.05 | 24.3 | 18.84 | 33.1 |
| Scale | F | P | Significance* | F | P | Significance* | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FA | 7.099 | 0.005 | 1–2** | 1.157 | 0.334 | n.s. | ||||||
| NV | 4.036 | 0.035 | 1–3*** | 1.232 | 0.312 | n.s. | ||||||
| PA | 10.882 | 10.001 | 1–2, 1–3 | 10.115 | 10.892 | n.s. | ||||||
| DY | 0.047 | 0.954 | n.s. | 2.275 | 0.128 | n.s. | ||||||
| SL | 2.140 | 0.145 | n.s. | 0.121 | 0.887 | n.s. | ||||||
| AP | 1.947 | 0.170 | n.s. | 5.966 | 0.009 | n.s. | ||||||
| CO | 0.684 | 0.517 | n.s. | 0.287 | 0.754 | n.s. | ||||||
| DI | 5.428 | 0.014 | n.s. | 2.405 | 0.115 | n.s. | ||||||
| FI | 1.406 | 0.270 | n.s. | 0.313 | 0.734 | n.s. | ||||||
ABCW, women with breast cancer in anthroposophic care; CBCW, women with breast cancer in conventional care.
*P < 0.05 for significant difference; **1–2 = admission versus 1 year; ***1–3 = admission versus 5 years.
Table 4.
The means, standard deviations, F and P-values (Wilks lambda and Bonferroni correction) for the factors of the LSQ for admission, after 1 year and after 5 years
| Scale | ABCW (n = 21) | CBCW (n = 23) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Admission | 1 year | 5 years | Admission | 1 year | 5 years | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| PS | 84.26 | 13.5 | 90.30 | 10.5 | 87.66 | 12.3 | 89.44 | 10.3 | 88.91 | 12.5 | 91.05 | 11.2 |
| SI | 57.82 | 13.9 | 68.38 | 14.0 | 65.76 | 17.4 | 70.08 | 19.5 | 69.05 | 24.5 | 69.88 | 23.1 |
| QDA | 58.70 | 14.8 | 75.32 | 13.8 | 72.98 | 19.8 | 69.03 | 17.7 | 71.22 | 16.1 | 74.71 | 12.4 |
| SES | 63.66 | 16.6 | 73.47 | 17.0 | 72.79 | 15.3 | 74.35 | 12.6 | 70.37 | 17.1 | 77.44 | 16.5 |
| QFA | 73.47 | 16.2 | 73.74 | 13.6 | 75.65 | 13.7 | 76.03 | 16.5 | 71.30 | 17.4 | 76.05 | 17.0 |
| QFR | 77.14 | 10.4 | 74.29 | 12.2 | 78.50 | 10.2 | 78.73 | 13.8 | 77.11 | 11.2 | 70.56 | 21.2 |
| TotQL | 69.17 | 9.1 | 75.92 | 10.0 | 75.56 | 10.2 | 76.26 | 10.9 | 74.47 | 13.1 | 76.46 | 11.4 |
| Scale | F | P | Significance* | F | P | Significance* | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PS | 4.191 | 0.031 | 1–2** | 2.086 | 0.149 | n.s. | ||||||
| SI | 7.353 | <0.001 | 1–2, 1–3** | 0.044 | 0.957 | n.s. | ||||||
| QDA | 14.127 | 1<0.001 | 1–2, 1–3 | 11.106 | 10.349 | n.s. | ||||||
| SES | 32.541 | 3<0.001 | 1–2, 1–3 | 34.603 | 30.022 | 2–3**** | ||||||
| QFA | 0.236 | 0.792 | n.s. | 1.223 | 0.314 | n.s. | ||||||
| QFR | 0.960 | 0.401 | n.s. | 1.621 | 0.221 | n.s. | ||||||
| TotQL | 18.409 | 1<0.001 | 1–2, 1–3 | 10.465 | 10.634 | n.s. | ||||||
ABCW, women with breast cancer in anthroposophic care; CBCW, women with breast cancer in conventional care.
*P < 0.05 for significant difference; **1–2, admission versus 1 year; ***1–3, admission versus 5 years; ****2–3, 1 year versus 5 years.
CBCW
Changes over time calculated with the help of ANOVAs showed no significant change within the CBCW (n = 23) in any of the scales of the EORTC QLQ-C30, see Tables 2 and 3. There was one significant improvement in SES in the LSQ, between 1 and 5 years, see Table 4.
Comparison Between the 13 Matched Pairs of the ABCW and the CBCW
Table 5 presents the ES for the differences between the admission and the comparison after 5 years. There were small to moderate effects in nine of the scales of the EORTC QLQ-C30 (PF, RF, EF, CF, NV, PA, DY, AP and CO). In the LSQ, there was a small effect in SES and a large effect in QFR. For some scales/factors, the ES was attributable to improvement in one group and deterioration in the other; in others there were improvement in both groups but the improvement was greater in one of the groups, and still in others there was no change in one group but improvement in the other. The ES for seven of the scales/factors were in favor of the ABCW (RF, EF, CF, NV, PA, SES and QFR), and favored the CBCW for four of the scales/factors (PF, DY, AP and CO) (see Table 5).
Table 5.
The effect sizes (ES) after 5 years, means and standard deviations for the comparison of the scales of the EORTC QLQ-C30 and the factors of the LSQ (n = 13 matched pairs)
| ES† | ABCW | CBCW | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Admission | 5 years | Admission | 5 years | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| EORTC QLQ-C30 | |||||||||
| Functional | |||||||||
| PF‡ | −0.30 | 81.54 | 22.3 | 76.92 | 33.5 | 80.00 | 20.0 | 83.08 | 19.7 |
| RF§ | 0.47 | 50.00 | 35.4 | 65.38 | 37.6 | 76.92 | 25.9 | 65.38 | 42.7 |
| EF§ | 0.24 | 54.49 | 18.2 | 67.31 | 22.2 | 66.67 | 26.8 | 70.51 | 30.4 |
| CF§ | 0.22 | 64.10 | 24.4 | 79.49 | 24.7 | 74.36 | 28.6 | 79.49 | 21.7 |
| SF | 0.12 | 66.67 | 27.2 | 74.36 | 33.8 | 82.05 | 22.0 | 84.62 | 28.4 |
| QL | 0.18 | 44.87 | 19.4 | 65.38 | 21.7 | 56.41 | 34.0 | 69.23 | 21.3 |
| Symptom | |||||||||
| FA | −0.04 | 58.35 | 20.7 | 42.72 | 33.9 | 38.46 | 26.7 | 29.06 | 28.9 |
| NV§ | −0.23 | 10.26 | 18.7 | 1.28 | 4.6 | 6.41 | 14.5 | 2.56 | 6.3 |
| PA§ | −0.48 | 46.15 | 29.0 | 20.51 | 26.5 | 28.21 | 33.6 | 25.64 | 37.0 |
| DY‡ | 0.27 | 17.94 | 22.0 | 23.00 | 36.9 | 23.08 | 28.5 | 17.77 | 17.1 |
| SL | 0.05 | 41.03 | 24.2 | 43.59 | 34.4 | 35.90 | 34.6 | 35.90 | 39.6 |
| AP‡ | 0.27 | 5.13 | 12.5 | 5.13 | 12.5 | 5.12 | 12.5 | 0.00 | 0.0 |
| CO‡ | 0.22 | 17.95 | 22.0 | 17.95 | 25.9 | 15.38 | 29.2 | 7.69 | 14.6 |
| DI | −0.13 | 12.82 | 16.9 | 13.72 | 21.3 | 10.26 | 21.0 | 15.38 | 32.2 |
| FI | 0.00 | 38.46 | 46.8 | 33.33 | 36.0 | 25.04 | 24.2 | 20.51 | 39.8 |
| LSQ | |||||||||
| PS | 0.01 | 86.97 | 11.9 | 88.38 | 14.1 | 88.22 | 11.2 | 89.50 | 12.2 |
| SI | 0.10 | 57.88 | 11.6 | 64.65 | 19.9 | 68.13 | 20.9 | 72.16 | 24.7 |
| QDA | 0.02 | 60.13 | 14.9 | 71.23 | 21.9 | 67.82 | 20.3 | 76.29 | 12.1 |
| SES§ | 0.28 | 66.02 | 14.1 | 71.98 | 15.7 | 74.45 | 14.2 | 75.55 | 20.1 |
| QFA | 0.16 | 70.33 | 18.2 | 73.36 | 14.9 | 72.09 | 17.9 | 71.47 | 19.1 |
| QFR§ | 0.88 | 75.38 | 11.5 | 78.24 | 10.3 | 74.95 | 14.7 | 64.40 | 24.5 |
| TotQL | 0.15 | 69.45 | 8.5 | 74.35 | 11.6 | 74.28 | 12.1 | 74.90 | 12.9 |
ABCW, women with breast cancer in anthroposophic care; CBCW, women with breast cancer in conventional care.
†ES = 0.20–0.50, small; ES = 0.50–0.80, moderate; ES > 0.80, large (22).
‡In favor of the CBCW.
§In favor of the ABCW.
The Outcome of the Matching Procedure
In Table 6, prognosis on admission to the study is shown in relation to 5 year survival. Of those with favorable prognosis on admission to the study, 73% were still alive after 5 years and 27% were deceased. Of those with unfavorable prognosis on admission, 88% were deceased and 12% were still alive after 5 years. The outcome in terms of survival in relation to prognosis on admission was in total 79% (82% for ABCW and 77% for CBCW).
Table 6.
The outcome of the matching procedure concerning prognosis on admission and survival after 5 years
| Prognosis | ABCW (n = 60) | CBCW (n = 60) | ||
|---|---|---|---|---|
| Favorable | Unfavorable | Favorable | Unfavorable | |
| Still alive | 25 | 1 | 26 | 5 |
| Deceased | 10 | 24 | 9 | 20 |
ABCW, women with breast cancer in anthroposophic care; CBCW, women with breast cancer in conventional care.
For 49 of the 60 matched pairs, the outcome was the same: 26 were deceased and 23 alive after 5 years. For the remaining 11 pairs, 8 women who had chosen anthroposophic care died and their matched twins in conventional treatment were alive, and 3 women in anthroposophic care were alive, whereas their matched twins in conventional treatment had died.
Discussion
As reported earlier, the women who chose anthroposophic care rated their quality of life/life satisfaction lower on entering the study than that of the women in the conventional treatment group (14). They also used more passive and anxious coping compared with their matched ‘twins’ on admission to the study. The results from the 1 year follow-up showed that the women who took initiative to be referred to anthroposophic care reported increased quality of life/life satisfaction after treatment at the anthroposophic hospital compared with the women receiving conventional treatment (15). The results of the present study showed the same pattern; the women in anthroposophic care still reported increased quality of life after 5 years, but the improvements were seen between admission and 1 year and not further on.
The difference in survival rate between the two groups after 5 years, 43% in ABCW versus 52% in CBCW, was not statistically significant. Although the tendency toward lower survival rate in the group in anthroposophic care is in agreement with the results reported by Risberg et al. (8) that the survival rate was lower for CAM users, there are no data available in the present study that could explain this tendency. It is important to study survival of CAM users in future studies.
The finding that the women who chose anthroposophic treatment reported worse quality of life on admission than those on conventional treatment is in agreement with the outcome of other studies, showing that women who used CAM express more psychological problems and perceive worse quality of life (4,7).
The women treated with anthroposophic therapy expressed increased quality of life/life satisfaction after 5 years compared with admission to the study. The improvements took place between admission and 1 year but not further on. The women treated with conventional care assessed the same quality of life/life satisfaction after 5 years as on admission except for the factor called SES, where there was an increase from one to 5 years. Of the seven scales/factors in which the ES favored the women choosing anthroposophic care, five could be categorized as emotional (RF, EF, CF, SES and QFR), whereas the four scales in which the ES favored the women on conventional treatment could be categorized as physical (PF, DY, AP and CO) (see Table 5).
The intervention for the women in the ABCW was treatment at the anthroposophic hospital with a special program for ∼2 weeks (mean 14.2 days, range 5–29 days). This is a short time, especially for evaluation after 5 years. There are no systematic data covering the use of anthroposophic treatment for the time between the intervention and the 5 year follow-up. But according to the interview performed after 5 years, 16 of the 21 women who survived for 5 years had continued their contact with the anthroposophic hospital. Four women had had new treatment periods at the anthroposophic hospital and four both new treatments periods and visits to the anthroposophic primary health care clinic. Six women had visited the primary health care clinic, and the remaining two had had telephone contact.
Study Limitations
There are limitations of the study that must be considered. The first is the design of the study. A randomized clinical study would have been preferable, but it was not possible considering the resources available and the regulations of the Swedish health care system. Thus, the present design with individually matched pairs was an option. But since the women took initiatives themselves to be referred to anthroposophic care, there could be differences between the women in ABCW and the women in the CBCW that were not controlled for by the matching procedure. The women were individually matched regarding stage of disease, age, treatment during the 3 months before entering the study and prognosis. There were no differences between the groups regarding children or marital status but there was a difference regarding the professions of the women on admission of the study (14). In the ABCW ∼23% compared with none in the CBCW were working as artists, journalists or other cultural workers. This could be one explanation to why some of the women choose the anthroposophic hospital and it could also mean that the two groups differed psychologically. The groups were not equal regarding quality of life assessments at baseline and there could have been a spontaneous recovery in ABCW towards the level of the CBCW. The phenomenon regression to the mean must always be considered in longitudinal studies. A comparison with Swedish women aged 20–80 years randomly selected from the Swedish population register (22) showed that both ABCW and CBCW estimated the over all quality of life/life satisfaction, measured by the LSQ, lower at inclusion to the study (P < 0.001, ABCW, n = 60; P = 0.018, CBCW, n = 60). After 5 years there was no significant difference in over all quality of life in ABCW or CBCW compared to Swedish women (ABCW, n = 21; CBCW, n = 23).
Another limitation is the sample size and the fact that although there were 60 matched pairs on admission there were only 13 matched pairs who took part in the study after 5 years. It took ∼4 years to include the 120 women in the study and unfortunately it was not possible to go on for a longer time with the inclusion. This was partly due to economical restriction at the anthroposophic hospital. According to the power analysis prior to the study, 60 pairs would be enough, but 13 is of course too few. This means that there could be a risk of Type II error.
Study Strengths
Although there are limitations, there are also some strengths that should be mentioned. The first is that the instruments used have been tested for reliability and validity and show acceptable psychometric properties (16,17). The results were almost the same measured with the two instruments. Other strengths are the careful matching procedure and the low rate of dropouts. The 5 year comparison showed that for 82% of the matched pairs, the survival outcome was similar. Thus, it was concluded that the accuracy of the matching categories on admission of the study had been valid.
Conclusion
It was concluded that the women who had chosen a period of care at the anthroposophic hospital, and who had survived for 5 years had increased their quality of life/life satisfaction. After 5 years there were improvements in overall quality of life and in emotional and social functioning compared to admission for the women in anthroposophic care. The improvements took place between admission and 1 year, but not further on. Only minor improvements were found in the matching group.
Acknowledgments
The study was supported by the Swedish Council of Planning and Co-ordination of Research (No: 950204:6), the Swedish Cancer Society (No: 3684-B95-01XAB; 3684-B96-02XBB; No 3684-B97-03XAA), the Gyllenberg Foundation, Finland and the Agape Foundation, Sweden. Receiver of grants: Elisabeth Hamrin.
Conflict of Interest
Ursula Flatters is a physician and earlier chief administrator at the anthroposophic hospital where the women in ABCW were recruited and Thomas Hatschek worked earlier as oncologist at the out-patient department where the women in the CBCW were recruited. Maria Arman-Rehnsfeldt and Marie Backman collected the data. Maria Arman-Rehnsfeldt has nursing experience from both anthroposophic and conventional medicine and Marie Backman from conventional medicine only. The other two authors have no financial or organisational relationships that could bias the work.
References
- 1.Cassileth BR, Schraub S, Robinson E, Vickers A. Alternative medicine use world wide. Cancer. 2001;91:1390–3. doi: 10.1002/1097-0142(20010401)91:7<1390::aid-cncr1143>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 2.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280:1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 3.Molassiotis A, Fernandez-Ortega P, Pud D, Ozden G, Scott JA, Panteli V, et al. Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol. 2005;16:655–63. doi: 10.1093/annonc/mdi110. [DOI] [PubMed] [Google Scholar]
- 4.Cassileth BR, Deng G. Complementary and alternative therapies for cancer. Oncologist. 2004;9:80–9. doi: 10.1634/theoncologist.9-1-80. [DOI] [PubMed] [Google Scholar]
- 5.Goldstein MS, Brown ER, Ballard-Barbash R, Morgenstern H, Bastani R, Lee J, et al. The use of complementary and alternative medicine among California adults with and without cancer. Evid Based Complement Alternat Med. 2005;2:557–65. doi: 10.1093/ecam/neh138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Risberg T, Kolstad A, Cassileth BR. Use of alternative medicine among Norwegian cancer patients associated with mental distress—a follow-up study. Acta Oncol. 2002;41:646–51. doi: 10.1080/028418602321028265. [DOI] [PubMed] [Google Scholar]
- 7.Risberg T, Jacobsen BK. The association between mental distress and the use of alternative medicine among cancer patients in North Norway. Qual Life Res. 2003;12:539–44. doi: 10.1023/a:1025063705413. [DOI] [PubMed] [Google Scholar]
- 8.Risberg T, Vickers A, Bremnes RM, Wist EA, Kaasa S, Cassileth BR. Does use of alternative medicine predict survival from cancer? Eur J Cancer. 2003;39:372–7. doi: 10.1016/s0959-8049(02)00701-3. [DOI] [PubMed] [Google Scholar]
- 9.Hamrin E, Carlsson M, Häggmark C, Langius A, Wahlström A. Utvärdering av bröstcancerpatienters livssituation utifrån olika vårdperspektiv. Rapporförstudier. (Evaluation of the Life Situation among Breast Cancer Patients from Different Care Perspectives. Report from Prestudies. In Swedish with English summary). Linköping: Omvårdnadsforskning vid Hälsouniversitetet i Linköping; No 9/ 1996. [Google Scholar]
- 10.Evans M, Rodger I. Anthroposophical Medicine: Healing for Body, Soul and Spirit. London: Thorsons; 1992. [Google Scholar]
- 11.Hamrin E. Evaluation of complementary care in breast cancer—a scientific challenge. Eur J Cancer. 2001;37:407. [Google Scholar]
- 12.Carlsson M, Hamrin E. Measurement of quality of life in women with breast cancer. Development of a life satisfaction questionnaire (LSQ-32) and a comparison with the EORTC QLQC-30. Qual Life Res. 1996;5:265–74. doi: 10.1007/BF00434748. [DOI] [PubMed] [Google Scholar]
- 13.Anthony D. Edinburgh: Churchill Livingstone; 1999. Understanding advanced statistics. A guide for nurses and health care researchers. [Google Scholar]
- 14.Carlsson M, Arman M, Backman M, Hamrin E. Perceived quality of life and coping for Swedish women with breast cancer who choose complementary care. Cancer Nurs. 2001;24:395–401. doi: 10.1097/00002820-200110000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Carlsson M, Arman M, Backman M, Flatters U, Hatschek T, Hamrin E. Evaluation of quality of life/life satisfaction in women with breast cancer in complementary and conventional care. Acta Oncol. 2004;43:27–34. doi: 10.1080/02841860310020339. [DOI] [PubMed] [Google Scholar]
- 16.Fayers P, Aaronson N, Bjordal K, Curran D, Groenvold M. Scoring Manual. Brussels: EORTC Quality of Life Study Group; 1999. (Available at: http://www.eortc.be/home/qol/manuals.htm) [Google Scholar]
- 17.Carlsson M, Hamrin E. Evaluation of the life satisfaction questionnaire (LSQ) using structural equation modelling (SEM) Qual Life Res. 2002;11:415–25. doi: 10.1023/a:1015670628990. [DOI] [PubMed] [Google Scholar]
- 18.Carlsson M, Hamrin E. The Life Satisfaction Questionnaire (LSQ). Manual. Uppsala: Department of Public Health and Caring Sciences, Uppsala University and Linköping: Department of Medicine and Care, University of Linköping; 2002. [Google Scholar]
- 19.Rutqvist LE, Fornander T, Fernstad R, Wilkin N, Bäckdahl M, Skoog L, et al. Bröstcancer. Diagnostik, behandling och uppföljning i Stockholm-Gotland regionen. Vårdprogram. (Breast Cancer. Diagnostics, Treatment and Follow-up in the Stockholm-Gotland Region. Care Program. In Swedish) Stockholm: Onkologiskt Centrum Stockholm-Gotland, 1996. [Google Scholar]
- 20.Hair JF, Anderson RE, Tatham RL, Black WC. Multivariate Data Analysis. 5th edn. Prentice-Hall International Inc.; 1998. [Google Scholar]
- 21.Cohen J. Statistical Power Analysis for the Behavioural Sciences. 2th edn. Mahwah, NJ: L. Erlbaum; 1998. [Google Scholar]
- 22.Carlsson M, Hamrin E, Lindqvist R. Psychometric assessment of the Life Satisfaction Questionnaire (LSQ) and a comparison of a randomised sample of Swedish women and those suffering from breast cancer. Qual Life Res. 1999;8:245–53. doi: 10.1023/a:1008875306645. [DOI] [PubMed] [Google Scholar]