Abstract
The 13C4 monoclonal antibody (MAb) recognizes the B subunit of Stx1 (StxB1) and neutralizes the cytotoxic and lethal activities of Stx1. However, this MAb does not bind to the B polypeptide of Stx2, despite the 73% amino acid sequence similarity between StxB1 and StxB2. When we compared the amino acid sequences of StxB1 and StxB2, we noted three regions of dissimilarity (amino acids 1 to 6, 25 to 32, and 54 to 61) located near each other on the crystal structure of StxB1. To identify the 13C4 epitope, we generated seven Stx1/Stx2 B chimeric polypeptides that contained one, two, or three of the dissimilar StxB1 regions. The 13C4 MAb reacted strongly with StxB1 and the triple-chimeric B subunit but not with the other chimeras. Mice immunized with the triple-chimeric B subunit survived a lethal challenge with Stx1 but not Stx2, substantiating the identified regions as the 13C4 MAb epitope and suggesting that the incorporation of this epitope into StxB2 altered sites necessary for anti-Stx2-neutralizing Ab production. Next, single amino acid substitutions were made in StxB1 to mimic Stx1d, a variant not recognized by the 13C4 MAb. The 13C4 MAb reacted strongly to StxB1 with the T1A or G25A mutations but not with the N55T change. Finally, we found that the 13C4 MAb blocked the binding of Stx1 to its receptor, globotriaosyl ceramide. Taken together, these results indicate that the 13C4 MAb prevents the interaction of Stx1 with its receptor by binding three nonlinear regions of the molecule that span receptor recognition sites on StxB1, one of which includes the essential residue 55N.
In the United States, Shiga toxin-producing Escherichia coli (STEC) strains account for about 110,000 infections per year (16). Enterohemorrhagic E. coli (EHEC) strains are a subset of STEC that contain a large pathogenicity island called the locus of enterocyte effacement and carry a 90-kb plasmid (13, 30, 32). Enterohemorrhagic E. coli serotype O157:H7 in particular is noted for it association with food-, water-, or petting zoo-linked outbreaks of Stx-mediated disease (4, 23, 28). A possible complication from an infection with an Stx-producing organism is the hemolytic uremic syndrome (HUS), a syndrome that is characterized by hemolytic anemia, thrombic thrombocytopenia, and renal failure. The majority of patients with HUS are children (5, 23), and there is a 5 to 10% fatality rate for those individuals. Furthermore, HUS survivors may have lasting kidney damage. Currently, there are no FDA-approved therapies or vaccines in the United States to combat or prevent illness from STEC, but several promising options for the future are under investigation. These options include receptor mimics and active and passive immunization strategies (reviewed in references 17 and 31). Several recent vaccine candidates not described in the above-mentioned reviews include Stx1 and Stx2 genetic toxoids, a plant-based Stx2 toxoid, and a chimeric StxA2/StxB1 toxoid that elicits a neutralizing antibody response and provides protection against a lethal challenge of both Stx1 and Stx2 (25, 33, 34). Several groups are pursuing passive immunization strategies that utilize humanized or human monoclonal antibodies (MAb) that neutralize one or more Stxs (6, 7, 12, 18, 19, 35).
STEC may produce one or more types of Stxs. There are two main serogroups of Stxs, Stx/Stx1 and Stx2. Stx is produced from Shigella dysenteriae type1, while Stx1 and Stx2 are produced from Escherichia coli. The Stx/Stx1 and Stx2 groups are defined by the fact that polyclonal antiserum to one toxin group does not cross-neutralize the cytotoxicity of the other toxin group (27, 34). Stx and Stx1 are virtually identical, with only one amino acid difference in the A subunit. The Stx1 and Stx2 A and B subunits are 68 and 73% similar at the amino acid level, respectively, and the crystal structures of Stx and Stx2 are remarkably similar (8, 9). Variants of Stx1 and Stx2 include Stx1c, Stx1d, Stx2c, Stx2d, Stx2d-activatable (Stx2dact), Stx2e, and Stx2f (reviewed in reference 17).
The Stxs are complex holotoxins with an AB5 structure. The active domain (A) contains an N-glycosidase that depurinates the 28S rRNA of the 60S ribosomal subunit, an event that stops protein synthesis and eventually leads to cell death. The A subunit is ∼32 kDa and is proteolytically cleaved by trypsin or furin into an ∼28-kDa A1 subunit and an ∼5-kDa A2 peptide, components that are connected through a single disulfide bond. The A1 subunit contains the active domain, and the A2 peptide noncovalently tethers the active domain to the binding domain. The binding subunit (B) consists of five identical ∼7.7-kDa monomers that form a pentamer through which the C terminus of the A2 peptide traverses. Each of the B subunit monomers has two cysteine residues that form a disulfide bond within each monomer. The B pentamer preferentially binds the eukaryotic receptor globotriaosyl ceramide (Gb3) (or globotetraosylceramide as is the case for Stx2e). Three receptor binding sites per B monomer have been proposed (14). However, several studies suggest that the second receptor binding site is the primary site through which each monomer interacts with its receptor (14, 24, 29).
The murine 13C4 MAb that was generated in our laboratory over 20 years ago by Nancy Strockbine binds to StxB1 and neutralizes Stx1 but does not bind to StxB2 or neutralize Stx2 (26). Previously, Boyd et al. attempted to map the epitope of the 13C4 MAb (2). Although those authors did not succeed in mapping the 13C4 MAb binding site, they did conclude that the epitope was conformational and that the disulfide bond formed within each StxB1 monomer was critical for the proper folding of that molecule and recognition by the 13C4 MAb. Recently, it was reported that the 13C4 MAb does not detect Stx1d, an Stx1 variant that differs from StxB1 by only three amino acids in the mature B subunit (3). In this report, we define the sites on StxB1 recognized by the 13C4 MAb that are necessary for the generation of Stx1-neutralizing antibodies and protective immunity. We also demonstrate that this 13C4 MAb epitope overlaps the amino acid sequence for the second and likely major receptor binding site on each StxB1 monomer.
MATERIALS AND METHODS
Bacterial strains, plasmids, and media.
Bacteria were grown in Luria-Bertani (LB) broth or on LB agar (Becton Dickinson and Company, Sparks, MD) supplemented with 100 μg/ml of ampicillin or 20 μg/ml of chloramphenicol as needed for the selection of recombinant plasmids. Bacterial strains and plasmids used in this study are listed in Table 1.
TABLE 1.
Bacterial strains and plasmids used in this study
| Strain or plasmid | Relevant characteristic(s) | Source or reference |
|---|---|---|
| E. coli strains | ||
| XL10 Gold | Tetr Δ(mcrA)183 Δ(mcrCB-hsdSMR-mrr)173 endA1 supE44 thi-1 recA1 gyrA96 relA1 lac Hte [F′ proAB lacIqZΔM15 Tn10 (Tetr) Amy Camr] | Stratagene |
| BL21(DE3) | F−ompT hsdSB(rB− mB−) gal dcm (DE3) | Novagen |
| Cloning vectors | ||
| pTrcHis2 C | E. coli expression vector (Ampr) | Invitrogen |
| pBluescript II KS (−) | E. coli cloning vector (Ampr) | Stratagene |
| pACYC184 | E. coli cloning vector (Cmr Tetr) | NEB |
| Recombinant plasmids | ||
| pMJS1 | pBluescript II KS (−) clone of stx1 | 25 |
| pMJS2 | pBluescript II KS (−) clone of stx2 | 25 |
| pMJS35 | pTrcHis2 C clone of stxB1 | This study |
| pMJS36 | pTrcHis2 C clone of stxB2 | This study |
| pMJS36A | pTrcHis2 C clone of stxB1-stxB2 chimeric gene (StxB1 = aa 1-6) | This study |
| pMJS36B | pTrcHis2 C clone of stxB1-stxB2 chimeric gene (StxB1 = aa 25-32) | This study |
| pMJS36C | pTrcHis2 C clone of stxB1-stxB2 chimeric gene (StxB1 = aa 54-61) | This study |
| pMJS36AB | pTrcHis2 C clone of stxB1-stxB2 chimeric gene (StxB1 = aa 1-6, 25-32) | This study |
| pMJS36AC | pTrcHis2 C clone of stxB1-stxB2 chimeric gene (StxB1 = aa 1-6, 54-61) | This study |
| pMJS36BC | pTrcHis2 C clone of stxB1-stxB2 chimeric gene (StxB1 = aa 25-32, 54-61) | This study |
| pMJS36ABC | pTrcHis2 C clone of stxB1-stxB2 chimeric gene (StxB1 = aa 1-6, 25-32, 54-61) | This study |
| pMJS37 | pACYC184 clone of stxA1 | This study |
| pMJS39 | pTrcHis2 C clone of stxB1 with single mutation (T1A) | This study |
| pMJS40 | pTrcHis2 C clone of stxB1 with single mutation (G25A) | This study |
| pMJS41 | pTrcHis2 C clone of stxB1 with single mutation (N55T) | This study |
Construction of plasmids that contain the stxB1-stxB2 chimeric genes.
A set of seven stxB1-stxB2 chimeric genes encoding either one, two, or all three StxB1 regions (hereafter referred to as regions A, B, and C) that comprise the putative 13C4 MAb epitope was generated by PCR with the splicing by overlap extension (SOE) protocol (11). Regions A, B, and C contain amino acids (aa) 1 to 6, 25 to 32, and 54 to 61, respectively, of StxB1. All primers used in this study are listed in Table 2. Initially, stxB1 and stxB2 were amplified by PCR from clones that contain stx1 or stx2, respectively, and ligated into pBluescript II KS (−) (Stratagene, La Jolla, CA). The stxB1-stxB2 chimeric genes were then generated by SOE PCR and ligated into pBluescript II KS (−). To add a common epitope to all of the chimeric B subunits, the stxB1-stxB2 hybrid genes were again amplified by PCR, and six histidine codons were incorporated immediately downstream of these B genes. During this round of PCR, an optimized Shine-Dalgarno sequence for enhanced translation (TAAGGAGGACAGCTATG [the optimized Shine-Dalgarno sequence is underlined, and the translational start site is in bold]) was also added upstream of the start codons. The modified chimeric genes were then ligated into the expression vector pTrcHis2 C (Invitrogen, Carlsbad, CA) and transformed into E. coli strain BL21(DE3). Cloning the genes for the B subunits in this manner allowed the transcription of the chimeric genes to be under the control of the pTrc promoter and added a common epitope to all the expressed constructs. This common tag on the proteins provided a means to normalize the amounts of B subunit proteins in different bacterial lysates through Western blot analyses with a MAb that recognized the six-histidine epitopes. Three additional individual mutations were generated by SOE PCR in stxB1 to mimic the three amino acid differences between the mature StxB1d and StxB1 (T1A, G25A, or N55T). These constructs were sequenced at the Biomedical Instrumentation Center at the Uniformed Services University of the Health Sciences to verify that the correct mutations were generated.
TABLE 2.
Synthetic oligonucleotide primers used in this study
| Primer | Sequence (5′→3′)a | Purpose/region of homology |
|---|---|---|
| 2F6 | GGTAAAATTGAGTTTTCCAAGTATAA | Used with 1R6 to generate pMJS36A, pMJS36AB, pMJS36AC, and pMJS36ABC |
| 1R6 | TTATACTTGGAAAACTCAATTTTACCAGTTACACAATCAGGCGTCGC | Used with 2F6 to generate pMJS36A, pMJS36AB, pMJS36AC, and pMJS36ABC |
| 1F2532 | GGTGATAAAGAATTATTTACCAACCGCTGGAATCTGCAACCGTTACTGCAAAGT | Used with 1R2532 to generate pMJS36B, pMJS36AB, pMJS36BC, and pMJS36ABC |
| 1R2532 | GTTGGTAAATAATTCTTTATCACCAACCTTCACTGTAAATGTGTCATCCTCATT | Used with 1F2532 to generate pMJS36B, pMJS36AB, pMJS36BC, and pMJS36ABC |
| 1F5461 | ACTAATGCCTGTCATAATGGAGGGGGATTTGCTGAAGTGCAGTTTAATAATGAC | Used with 1R5461 to generate pMJS36C, pMJS36AC, pMJS36BC, and pMJS36BC |
| 1R5461 | CCCTCCATTATGACAGGCATTAGTTTTGATTGTGACAGTCATTCCTGTCAACTG | Used with 1F5461 to generate pMJS36C, pMJS36AC, pMJS36BC, and pMJS36BC |
| 1B5SD | GATCGGATCCTAAGGAGGACAGCTATGAAAAAAACATTATTAATAGCTGCATCGCTTTCATTTTTTTCAGCAAGTGCGCTGGCG | stxB1 upstream primer with optimized Shine-Dalgarno sequence, used to generate pMJS35, pMJS36A, pMJS36AB, pMJS36AC, and pMJS36ABC |
| 1B3N2 | GATCGAATTCTCAGTGGTGGTGGTGGTGGTGACGAAAAATAACTTCGCTGAATCCCCCTCCATTATGACAGGC | stxB1 His-tagged downstream primer, used to generate pMJS35 |
| 2B5SD | GATGGGATCCTAAGGAGGACAGCTATGAAGAAGATGTTTATGGCGGTTTTATTTGCATTAGC | stxB2 upstream primer with optimized Shine-Dalgarno sequence, used to generate pMJS36 pMJS36B, pMJS36C, and pMJS36BC |
| 2B3N2 | GATCGAATTCTCAGTGGTGGTGGTGGTGGTGGTCATTATTAAACTGCACTTCAGCAAATCCGGAGCCTGATTCACAGG | stxB2 His-tagged downstream primer #1, used to generate pMJS36, pMJS36A, pMJS36B, and pMJS36AB |
| 2B3N3 | GATCGAATTCTCAGTGGTGGTGGTGGTGGTGGTCATTATTAAACTGCACTTCAGCAAATCCCCCTCCATTATGACAGGC | stxB2 His-tagged downstream primer #2, used to generate pMJS36C, pMJS36AC pMJS36BC, and pMJS36ABC |
| 1dBAF | CGCCTGATTGTGTAACTGGAAAGGTGG | Used with 1dBAR to generate pMJS39 |
| 1dBAR | CCAGTTACACAATCAGGCGCCGCCAGCGCACTTGCTGAAAAAAATGAAAGCGATGC | Used with 1dBAF to generate pMJS39 |
| 1dBBF | GCAGATAAAGAATTATTTACCAACAGATGG | Used with 1dBBR to generate pMJS40 |
| 1dBBR | CTGTTGGTAAATAATTCTTTATCTGCCACTTTAACTGTAAAGGTATCGTCATC | Used with 1dBBF to generate pMJS40 |
| 1dBCF | ACTGCCTGTCATAATGGAGGGGGATTCAGC | Used with 1dBCR to generate pMJS41 |
| 1dBCR | CCCTCCATTATGACAGGCAGTAGTTTTAATGGTTACAGTCATCCCCGTAATTTGCGC | Used with 1dBCF to generate pMJS41 |
| MJS1 | GATCGGATCCCCCTGTAACGAAGTTTGCGTAACAGC | stx1 upstream primer, used with 1A3 to generate pMJS37 |
| 1A3 | GATCTCTAGACCTCAACTGCTAATAGTTCTGCGC | stxA1 downstream primer, used with MJS1 to generate pMJS37 |
Restriction enzyme sites are underlined; sites of mutations are in bold.
Western blotting.
Purified Stx1 or whole-cell bacterial lysates that contained His-tagged StxB1 or StxB2 or the seven His-tagged chimeric StxB1/StxB2 proteins were subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis and Western blot analysis as previously described (25) In brief, overnight cultures of E. coli BL21(DE3) that contained clones of the His-tagged B subunits were diluted 1:50 into 5 ml of LB broth and incubated for 3 h at 37°C. The cultures were then induced with 1 mM isopropyl β-d-thiogalactopyranoside (IPTG) and incubated for an additional 5 h. The induced cultures were then aliquoted into microfuge tubes, and sodium dodecyl sulfate-polyacrylamide gel electrophoresis sample buffer (containing 0.6 M dithiothreitol, 10% sodium dodecyl sulfate) was added. These samples were stored at −80°C. Prior to being loaded onto 15% polyacrylamide gels, the samples were heated to 95°C for 5 min. The concentrations of wild-type and chimeric B subunits loaded were normalized on preliminary Western blots by detection with the anti-six-histidine MAb (Novagen, Madison, WI) and quantified using the NIH Image J program (http://rsb.info.nih.gov/nih-image). Finally, two polyacrylamide gels were equivalently loaded with normalized samples and subjected to Western blot analysis with either the anti-six-histidine or the 13C4 MAb hybridoma tissue culture supernatant diluted 1:5 as the primary antibody. The secondary antibody for both Western blots was goat anti-mouse immunoglobulin G (IgG) conjugated to horseradish peroxidase (HRP) (Bio-Rad, Hercules, CA) at a dilution of 1:3,000. The secondary antibody was detected by chemiluminescence with the ECL-Plus Western blotting detection kit (Amersham Bioscience, Little Chalfont, Buckinghamshire, England).
Purification of the StxB1/StxB2 triple-chimeric B subunit ABC.
An overnight culture of E. coli BL21(DE3) that contained the pTrcHis2 C stxB1-stxB2 triple-chimeric B subunit clone pMJS36ABC was diluted 1:50 into 3 liters of LB broth. After 3 h of growth, the cultures were induced with 1 mM IPTG and incubated for an additional 5 h. The bacteria were sedimented by centrifugation and concentrated 75-fold by resuspension in 40 ml of 50 mM phosphate buffer containing 300 mM NaCl, pH 7.6 (sonication buffer). The concentrated bacterial suspensions were then disrupted by sonication and clarified by centrifugation. Each clarified lysate was then applied to a nickel affinity column (QIAGEN Inc., Valencia, CA) and eluted from the column with sonication buffer that contained 250 mM imidazole. The eluted proteins were then dialyzed against phosphate-buffered saline (PBS), pH 7.4, concentrated with a Centricon 3,000-molecular-weight-cutoff filter (Millipore Corporation, Bedford, MA), and sterilized by filtration through a 0.2-μm filter. After purification, the total protein concentration of the StxB1/StxB2 triple-chimeric ABC preparation was 288 ng/μl, as determined by a bicinchoninic acid assay (Pierce, Rockford, IL). The triple-chimeric B subunit ABC was recognized in the purified sample by Western blot analysis with the anti-six-histidine and 13C4 MAbs. A silver-stained gel showed that the triple-chimeric B subunit ABC was the major purified protein, although other bands were evident (data not shown).
Mouse immunization and challenge.
Preimmune serum was collected from 13 CD-1 male mice that weighed between 14 and 16 g (Charles River Laboratories, Boston, MA). The mice were then immunized intraperitoneally with 14.4 μg of the purified StxB1/StxB2 triple-chimeric B subunit ABC in PBS mixed 1:1 with TiterMax Gold, a water-in-oil adjuvant (total volume, 100 μl; TiterMax USA Inc., Norcross, GA). The mice were boosted at 3-week intervals with the same amount of the purified triple-chimeric B subunit ABC in adjuvant, for a total of four boosts. Two weeks after the last boost, the 13 immunized mice were divided into two groups, one containing 7 mice and the other containing 6 mice, and challenged with 10 times the 50% lethal dose (LD50) of either Stx1 (1,250 ng) or Stx2 (10 ng), respectively. The 14 naïve CD-1 male mice were divided into two groups that contained 7 mice each and challenged with 10 LD50s of either Stx1 or Stx2.
ELISA.
Ten days after the fourth and final boost, serum was collected from each of the immunized mice. These samples were compared to the appropriate preimmune serum sample by enzyme-linked immunosorbent assays (ELISA) to determine serum IgG levels directed against StxB1 or StxB2, as reported previously (25). Serum samples from the 14 naïve mice were analyzed as negative controls. Briefly, 100 μg of purified Stx1 or Stx2 in PBS was used as the antigen, and mouse serum was used as the primary antibody after dilution in PBS that contained 0.05% Tween 20 (PBST-20). The secondary antibody, goat anti-mouse IgG conjugated to HRP, was added at a dilution of 1:3,000 in PBST-20. The ELISA titer was defined as the dilution of the postimmunization serum that was +0.1 optical density (405 nm) units above the prebleed value after the background optical density at 405 nm had been subtracted from it. These assays were performed once in duplicate.
In vitro neutralization assays.
The pre- and postimmunization sera from the 13 immunized mice and sera from the 14 naïve mice were used in in vitro neutralization assays against 10 50% cytotoxic doses (CD50s) of Stx1 and 25 CD50s of Stx2 by a previously described procedure (15, 25). The actual CD50 values were calculated retrospectively at the completion of the experiment. The neutralization titer was defined as the dilution of the mouse serum or 13C4 MAb that neutralized 50% of the cytotoxic effect of Stx1 or Stx2 on Vero cells. These assays were performed once in duplicate.
To examine the capacity of the 13C4 MAb to neutralize Stx1 with single amino acid changes in the B subunit that mimicked the differences of the 13C4 MAb-nonreactive variant Stx1d, we used the following approach. A second plasmid that contained stxA1 was cotransformed into bacteria that harbored clones that expressed StxB1 or StxB1 with the T1A, G25A, or N55T mutation. Bacteria cotransformed with both of these plasmids produced holotoxins that were cytotoxic for Vero cells. Clarified sonic lysates of bacteria that expressed these Stx1 holotoxins were subjected to in vitro neutralization assays with the 13C4 MAb (approximately 10 CD50s per toxin). We reasoned that if the individual amino acid changes altered reactivity with the 13C4 MAb, then the antibody would then no longer neutralize the toxicity of the mutant Stx1 for Vero cells.
Gb3 binding inhibition assay.
A Gb3 binding assay was used to determine whether the 13C4 MAb could inhibit Stx1 from interacting with its receptor. Unless otherwise noted, the Gb3 binding assay was done as described previously (1, 33). In brief, 1,200 pg of purified Stx1 was diluted in PBS that contained 0.05% Tween 80 (PBST-80) and 0.1% bovine serum albumin (hereafter called binding solution), and equal volumes of Stx1 were mixed with either binding solution, undiluted 13C4 MAb (Hycult Biotechnology, Uden, The Netherlands), or serially diluted (1:4) 13C4 MAb in binding solution. The toxin-antibody mixture (total volume, 120 μl) was incubated for 2 h at 37°C in 5%CO2, and 100 μl was then applied to Gb3 (Matreya, Inc., State College, PA)-coated microtiter plates (1 μg/well) that had been washed with PBST-80. The samples were incubated for 2 h at 37°C with the primary antibody, rabbit anti-Stx1 polyclonal antibody diluted 1:5,000 in binding solution. After washing unbound primary antibody from the wells with PBST-80 and PBS, the secondary antibody, goat anti-rabbit IgG conjugated to HRP (Bio-Rad), was added at a dilution of 1:1,000 and incubated for 1 h at 37°C. After another wash with PBST-80, followed by a wash with PBS, the secondary antibody was detected with a tetramethylbenzidine peroxidase enzyme immunoassay substrate kit (Bio-Rad), and the microtiter plates were incubated at room temperature for 15 min to allow for a color change to develop. The reaction mixtures were then transferred to a fresh microtiter plate and read at 600 nm. These assays were done twice in triplicate. Controls for this experiment included incubating Stx1 with an isotype-matched irrelevant MAb (11E10; Hycult Biotechnology) or with no antibody.
RESULTS
Analysis of StxB1 and StxB2 amino acid alignment and Stx1 B pentamer crystal structure.
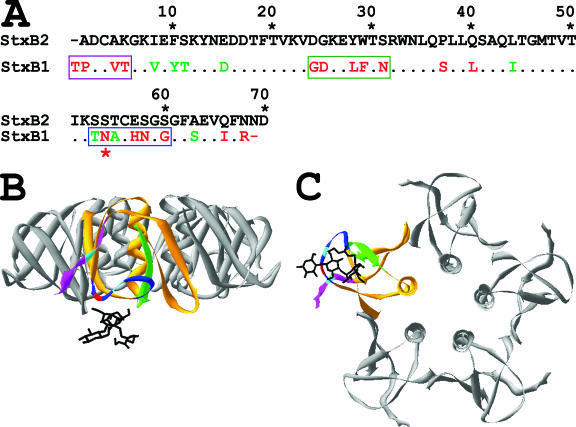
When the amino acids of the mature StxB1 and StxB2 proteins were aligned, three regions of high dissimilarity between the two proteins were evident (Fig. 1A). Two of these regions are centered around the cysteine residues at the N and C termini of the protein and comprise amino acids 1 to 6 and 54 to 61, respectively. The third region is in the middle of StxB1 and spans amino acids 25 to 32. Upon examination of the crystal structure of StxB1, we noticed that the three regions of dissimilarity were proximal to each other, as illustrated with the ribbon diagrams of the Stx1 B pentamer in Fig. 1B and C.
FIG. 1.
Amino acid alignment of StxB2 and StxB1 (A) and illustration of the 13C4 MAb epitope on the crystal structure of the Stx1 B pentamer complexed with an analogue of its Gb3 receptor at site number two (B and C; side view and bottom view, respectively). In panel A, green and red amino acids depict conserved and nonconserved amino acids, respectively. The three segments of the 13C4 MAb epitope are boxed in panel A and colored similarly in panel B. The red asterisk beneath StxB1 indicates the critical asparagine at residue 55. In panels B and C, the 13C4 MAb epitope is depicted on a single StxB1 monomer in the Stx1 B pentamer. The two cysteine residues that generate the disulfide bond are colored light blue in the crystal structure. The critical asparagines residue at position 55 is colored red in panels B and C. The amino acid sequences were aligned using the Align Plus 5 program, version 5.03 (Scientific & Educational Software, Durham, NC) following the global-ref alignment procedure (20) and the scoring matrix BLOSUM 62 (10). Accession numbers for StxB1 and StxB2 are M19473 and X07865, respectively. The program DeepView/Swiss-PDB viewer was used to model the X-ray crystallographic coordinates of the Stx1 B pentamer complexed with an analogue of its Gb3 receptor (14). The Brookhaven Protein Data Bank accession number for the crystal structure is 1BOS.
Western blot analysis of chimeric StxB1/StxB2 proteins with the 13C4 monoclonal antibody.
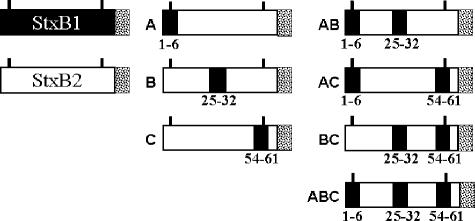
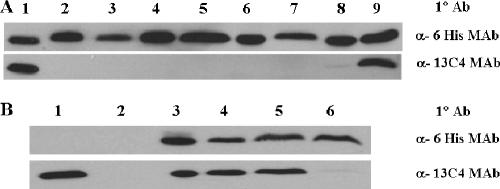
To map the 13C4 MAb epitope, wild-type StxB1 and StxB2 and seven chimeric Stx1/Stx2 B subunits consisting of one, two, all three, or all possible combinations of the three unique StxB1 regions were generated by a series of PCR and splicing by overlap extension reactions (Fig. 2). The 13C4 MAb reacted strongly with Stx1, StxB1, and the triple-chimeric B subunit ABC that contained all three unique regions of StxB1 but only weakly with the double-chimeric B subunit AC; no signal was detected with the other chimeras (Fig. 3).
FIG. 2.
Illustration of histidine-tagged StxB1 and StxB2 and the seven histidine-tagged chimeric StxB1/StxB2 proteins. StxB1 is shown in black, while Stx2 is shown in white; the six-histidine tags at the C termini are speckled. The names of the seven chimeric proteins are shown to the left of the respective chimeric proteins, and the regions of StxB1 are listed beneath the chimeric B subunits. The first region in the StxB1 subunit, region A, consists of residues 1 to 6, while the second region, B, spans residues 25 to 32 and the third region, C, ranges from amino acids 54 to 61. The two cysteine residues in each B subunit are denoted by bars above the B subunits.
FIG. 3.
Western blot analyses of histidine-tagged StxB1, StxB2, and chimeric StxB1/StxB2 proteins (A) and StxB1 with single amino acid mutations (B) probed with α-six-His or α-13C4 MAbs. In panel A, lane 1 shows StxB1 and lane 2 shows StxB2. Lanes 3 to 9 contain the chimeric proteins that consist of Stx2 except for the following regions: for lane 3, StxB1 (aa 1 to 6); for lane 4, StxB1 (aa 25 to 32); for lane 5, StxB1 (aa 54 to 61); for lane 6, StxB1 (aa 25 to 32 and 54 to 61); for lane 7, StxB1 (aa 1 to 6 and 25 to 32); for lane 8, StxB1 (aa 1 to 6 and 54 to 61); and for lane 9, StxB1 (aa 1 to 6, 25 to 32, and 54 to 61). Lanes for panel B: 1, 100 ng Stx1; 2, vector only; 3, StxB1; 4, StxB1 T1A; 5, StxB1 G25A; 6, StxB1 N55T.
Analysis of StxB1 that contains single amino acid mutations by Western blotting and in vitro neutralization with the 13C4 MAb.
The 13C4 MAb does not recognize Stx1d, an Stx1 variant that has only three amino acid differences in the mature B subunit from Stx1 (4). Therefore, we generated three single StxB1 mutations that mimic those three differences (T1A, G25A, and N5T) and probed the resulting proteins with the 13C4 MAb by Western blotting. The 13C4 MAb detected Stx1, StxB1, and StxB1 with the T1A and G25A mutations but not StxB1 with the N55T mutation (Fig. 3). To further investigate the capacity of the 13C4 MAb to bind and neutralize the single amino acid mutations in StxB1, in vitro neutralization assays were done. The 13C4 MAb neutralized wild-type Stx1 and the Stx1 with the StxB1 T1A and G25A mutations, but not StxB1 with the N55T mutation (data not shown). The findings that the 13C4 MAb neither recognized the B subunit with the single N55T mutation nor neutralized StxB1 N55T strongly suggest that the 55th residue is critical for the binding of the 13C4 MAb. The critical asparagine residue is highlighted in Fig. 1A to C.
Immune response to StxB1/StxB2 triple-chimeric B subunit ABC immunization.
The 13 CD-1 mice that were immunized with the purified triple-chimeric StxB1/StxB2 protein ABC displayed high ELISA titers to Stx1 and Stx2, i.e., 5.1 and 3.8 logs above background, respectively (Table 3). None of the preimmune sera from the 13 immunized mice or sera from the 14 naïve mice displayed any appreciable ELISA titers to Stx1 or Stx2.
TABLE 3.
Stx1 and Stx2 IgG ELISA and neutralization titers from mice immunized with the triple-chimeric B subunit ABC
The geometric means ± standard deviations of the log IgG serum titers to Stx1 or Stx2.
The geometric means ± standard deviations of the log 50% neutralization titers to approximately 10 or 25 CD50s of Stx1 or Stx2, respectively. Sera from 12 out of 13 or 2 out of 13 mice neutralized Stx1 or Stx2, respectively. Samples that did not neutralize Stx1 or Stx2 were assigned a value of 0.3.
Because in vitro neutralization titers are a better indicator of a protective immune response than are ELISA titers (34) the sera were used in in vitro neutralization assays with purified Stx1 or Stx2 (CD50, 10 or 25, respectively). Serum samples from 12 of 13 immunized mice displayed high neutralization titers to Stx1, while samples from only 2 mice had neutralization titers to Stx2, which were 2.7 and 0.4 logs above background, respectively (Table 3). The preimmune sera from the 13 immunized mice and the sera from the 14 naïve mice displayed no neutralizing antibodies to Stx1 or Stx2. These data suggest that the StxB1 regions of the triple-chimeric B subunit ABC represent a neutralizing epitope.
Protection of immunized mice against lethal toxin challenge.
Two weeks after the final boost, the 14 control mice and the 13 immunized mice were challenged with 10 LD50s of either Stx1 or Stx2. The 14 nonimmunized mice were divided into two groups of 7 each and challenged with either Stx1 (group 1) or Stx2 (group 3). The 13 immunized mice were divided into two challenge groups; the Stx1 challenge group (group 2) contained 7 mice, while the Stx2 challenge group (group 4) contained 6 mice. Six of the seven immunized mice survived the Stx1 challenge, while only one of six immunized mice survived the Stx2 challenge (Table 4). None of the 14 naïve mice survived the Stx1 or Stx2 challenge; in fact, all of these animals died within 4 days of toxin administration. The survival of the immunized mice from the challenge experiments correlated directly with in vitro neutralizing antibody titers of the serum samples from those animals. Specifically, prior to Stx1 challenge, six of seven immunized mice had high neutralizing serum antibody titers to Stx1, and all six survived. The mouse that did not survive the lethal Stx1 challenge did not have neutralizing serum antibodies to Stx1. For the immunized group that was challenged with Stx2, two of the six mice had neutralizing serum antibody titers to Stx2, and the mouse with the highest neutralizing titer to Stx2 survived the lethal Stx2 challenge. The five immunized mice with either low (one mouse) or no (four mice) neutralizing serum antibody titers to Stx2 did not survive the Stx2 challenge.
TABLE 4.
Protection of mice immunized with the triple-chimeric B subunit ABC against a lethal challenge of Stx1 or Stx2
| Group | Immunization with ABC | Challenge with 10 LD50s ofa: | No. of surviving mice/total no. of mice |
|---|---|---|---|
| 1 | − | Stx1 | 0/7 |
| 2 | + | Stx1 | 6/7 |
| 3 | − | Stx2 | 0/7 |
| 4 | + | Stx2 | 1/6 |
The LD50s were previously determined to be 125 and 1 ng/mouse for Stx1 and Stx2, respectively. The average weight of the mice at the time of the challenge was 44.9 g.
Gb3 binding inhibition assay.
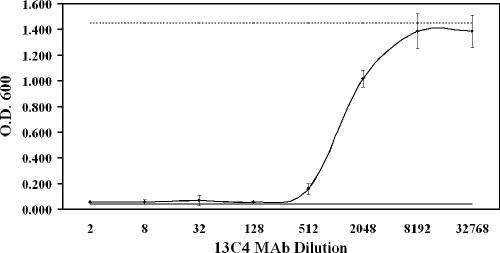
An in vitro binding inhibition assay was used to determine whether the 13C4 MAb could prevent the binding of Stx1 to Gb3. Stx1 and 13C4 MAb were incubated together and then overlaid onto Gb3-coated microtiter plates. Stx1 binding to Gb3 was not detected until the 13C4 MAb was diluted past 1:512 from a 0.1-mg/ml stock (Fig. 4). Maximal Stx1 binding occurred after the 13C4 was diluted to 1:8,000 or greater. These results show that the 13C4 MAb completely inhibited the binding of 1,000 pg of Stx1 to Gb3 in a dose-dependent manner.
FIG. 4.
The 13C4 MAb inhibits the binding of Stx1 to Gb3 in a dose-dependent manner. The individual circles represent averages of two experiments performed in triplicate, and the error bars indicate standard deviations (± 1). The solid line represents the background (1 μg Gb3 plus 1,000 pg of Stx1 and secondary antibody without primary antibody), while the dashed line represents Stx1 binding without the addition of the 13C4 MAb. O.D. 600, optical density at 600 nm.
DISCUSSION
Our results demonstrate that the 13C4 epitope is conformational in nature. We found that three nonlinear regions of StxB1 were required for full binding of MAb 13C4 to StxB1/StxB2 chimeras. Our results are consistent with the data of Boyd et al., who showed that the 13C4 MAb is a conformational epitope (2). Although the StxB1/StxB2 triple-chimeric B subunit ABC contains mostly StxB2 (only 22 out of 71 amino acids correspond to those of StxB1), ELISA and neutralization titers higher for Stx1 than for Stx2 were achieved after immunization with the triple-chimeric B subunit. These observations could reflect the fact that the 22 amino acids that comprise the 13C4 epitope are on the outside of the B pentamer and therefore are good targets for neutralizing antibodies. Furthermore, the localization of these regions on the outer face of the toxin B pentamer may increase the likelihood that these amino acids are immunodominant. Indeed, we found that when the 22 amino acids comprising the 13C4 MAb epitope were inserted into StxB2 and used to immunize mice, six of seven mice survived a lethal challenge of 10 LD50s of Stx1, whereas only one of six mice survived a lethal challenge of 10 LD50s of Stx2.
We further found that the asparagine at the 55th residue of StxB1 is a critical amino acid of the 13C4 MAb epitope by creating single amino acid substitutions to mimic the changes found in StxB1d (T1A, G25A, and N55T) and testing those mutants for binding or neutralization by the 13C4 MAb. The 13C4 MAb did not bind to StxB1 with the N55T mutation, nor did the antibody neutralize the Stx1 with the N55T mutation. The asparagine at the 55th residue of StxB1 is also a critical amino acid for the binding of another Stx1-neutralizing monoclonal antibody (5-5B) that recognizes the Stx1 B subunit but fails to recognize Stx1d (21). Additionally, a third MAb (2H3) that recognizes StxB1, but not StxB1d, has been described, and residue 55 may play a role in that difference as well (3). Finally, another MAb, VTm1.1 (later humanized and called TMA-15), recognizes StxB2 and neutralizes Stx2 (12, 22) but fails to recognize StxB2 when the 56th amino acid is mutated (E56H). The 55th residue of StxB1 and the 56th residue of StxB2 are both located on the outside of the B monomers in approximately the same location. Our results and the findings of others as summarized above support the idea that the 55th and 56th amino acids of StxB1 and StxB2, respectively, are critical residues for neutralizing MAbs directed against Stx1 and Stx2.
A crystal structure analysis of the Stx1 B pentamer complexed with a Gb3 analogue has shown that there are three receptor binding sites per StxB1 monomer (14). Here we identified the 13C4 MAb epitope and then used the structural information provided by Ling and colleagues (14) to map the 13C4 MAb epitope to regions of StxB1 that span the first and second receptor binding sites. Based on that analysis, we predicted that the 13C4 MAb epitope overlaps two Gb3 binding sites and speculated that the 13C4 MAb neutralizes the activity of Stx1 by either directly or indirectly (through steric hindrance) interfering with the engagement of the toxin with its glycolipid receptor. We then tested that hypothesis with our Gb3 binding inhibition assay, which showed that the 13C4 MAb completely blocked the binding of Stx1 to its receptor in a dose-dependent manner. Taken together, our results indicate that the creation of a vaccine that can elicit anti-StxB1-neutralizing antibodies may require all three of the nonlinear regions of the B subunit that comprise the 13C4 MAb epitope, since the domains responsible for protection are not contiguous. Furthermore, we speculate that the corresponding amino acids in the StxB2 molecule are required to elicit neutralizing antibodies to the Stx2 B subunit.
Acknowledgments
We acknowledge Eddy Twiddy for the purification of Stx1 and Stx2 used in these studies and Stephen Darnell for reference database management.
This research was supported by National Institutes of Health/National Institute for Allergy and Infectious Diseases grant #AI20148-24 and Uniformed Services University of the Health Sciences grant #RO73KD.
The views and assertions made concerning the results of this article are those of the authors and should not be construed as the views of the Department of Defense.
Editor: D. L. Burns
Footnotes
Published ahead of print on 9 October 2006.
REFERENCES
- 1.Ashkenazi, S., and T. G. Cleary. 1989. Rapid method to detect Shiga toxin and Shiga-like toxin I based on binding to globotriosyl ceramide (Gb3), their natural receptor. J. Clin. Microbiol. 27:1145-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boyd, B., S. Richardson, and J. Gariepy. 1991. Serological responses to the B subunit of Shiga-like toxin 1 and its peptide fragments indicate that the B subunit is a vaccine candidate to counter action of the toxin. Infect. Immun. 59:750-757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bürk, C., R. Dietrich, G. Açar, M. Moravek, M. Bülte, and E. Märtlbauer. 2003. Identification and characterization of a new variant of Shiga toxin 1 in Escherichia coli ONT:H19 of bovine origin. J. Clin. Microbiol. 41:2106-2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. 2005. Outbreaks of Escherichia coli O157:H7 associated with petting zoos—North Carolina, Florida, and Arizona, 2004 and 2005. Morb. Mortal. Wkly. Rep. 54:1277-1280. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. 1994. Addressing emerging infectious disease threats: a prevention strategy for the United States (executive summary). Morb. Mortal. Wkly. Rep. 43(RR-5):1-18. [PubMed] [Google Scholar]
- 6.Dowling, T. C., P. A. Chavaillaz, D. G. Young, A. Melton-Celsa, A. O'Brien, C. Thuning-Roberson, R. Edelman, and C. O. Tacket. 2005. Phase 1 safety and pharmacokinetic study of chimeric murine-human monoclonal antibody cαStx2 administered intravenously to healthy adult volunteers. Antimicrob. Agents Chemother 49:1808-1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edwards, A. C., A. R. Melton-Celsa, K. Arbuthnott, J. R. Stinson, C. K. Schmitt, H. C. Wong, and A. D. O'Brien. 1998. Vero cell neutralization and mouse protective efficacy of humanized monoclonal antibodies against Escherichia coli toxins Stx1 and Stx2, p. 388-392. In J. B. Kaper and A. D. O'Brien (ed.), Escherichia coli O157:H7 and other Shiga toxin-producing E. coli strains. ASM Press, Washington, D.C.
- 8.Fraser, M. E., M. M. Chernaia, Y. V. Kozlov, and M. N. James. 1994. Crystal structure of the holotoxin from Shigella dysenteriae at 2.5 Å resolution. Nat. Struct. Biol. 1:59-64. [DOI] [PubMed] [Google Scholar]
- 9.Fraser, M. E., M. Fujinaga, M. M. Cherney, A. R. Melton-Celsa, E. M. Twiddy, A. D. O'Brien, and M. N. James. 2004. Structure of Shiga toxin type 2 (Stx2) from Escherichia coli O157:H7. J. Biol. Chem. 279:27511-27517. [DOI] [PubMed] [Google Scholar]
- 10.Henikoff, S., and J. G. Henikoff. 1992. Amino acid substitution matrices from protein blocks. Proc. Natl. Acad. Sci. USA 89:10915-10919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higuchi, R. 1989. Using PCR to engineer DNA, p. 61-70. In H. A. Erlich (ed.), PCR technology. Stockton Press, New York, N.Y.
- 12.Kimura, T., M. S. Co, M. Vasquez, S. Wei, H. Xu, S. Tani, Y. Sakai, T. Kawamura, Y. Matsumoto, H. Nakao, and T. Takeda. 2002. Development of humanized monoclonal antibody TMA-15 which neutralizes Shiga toxin 2. Hybrid. Hybrid. 21:161-168. [DOI] [PubMed] [Google Scholar]
- 13.Levine, M. M. 1998. Immunoprophylaxis of Shiga toxin-producing Escherichia coli infection and disease: strengths and weaknesses of various strategies, p. 405-408. In J. B. Kaper and A. D. O'Brien (ed.), Escherichia coli O157:H7 and other Shiga toxin-producing E. coli strains. ASM Press, Washington, D.C.
- 14.Ling, H., A. Boodhoo, B. Hazes, M. D. Cummings, G. D. Armstrong, J. L. Brunton, and R. J. Read. 1998. Structure of the Shiga-like toxin I B-pentamer complexed with an analogue of its receptor Gb3. Biochemistry 37:1777-1788. [DOI] [PubMed] [Google Scholar]
- 15.Marques, L. R., M. A. Moore, J. G. Wells, I. K. Wachsmuth, and A. D. O'Brien. 1986. Production of Shiga-like toxin by Escherichia coli. J. Infect. Dis. 154:338-341. [DOI] [PubMed] [Google Scholar]
- 16.Mead, P. S., L. Slutsker, V. Dietz, L. F. McCaig, J. S. Bresee, C. Shapiro, P. M. Griffin, and R. V. Tauxe. 1999. Food-related illness and death in the United States. Emerg. Infect. Dis. 5:607-625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Melton-Celsa, A. R., M. J. Smith, and A. D. O'Brien. March. 2005, posting date. Chapter 8.7.8, Shiga toxins: potent poisons, pathogenicity determinants, and pharmacological agents, In R. Curtiss III et al (ed.), EcoSal—Escherichia coli and Salmonella: cellular and molecular biology. ASM Press, Washington, D.C. [Online.] http://www.ecosal.org. [DOI] [PubMed]
- 18.Mukherjee, J., K. Chios, D. Fishwild, D. Hudson, S. O'Donnell, S. M. Rich, A. Donohue-Rolfe, and S. Tzipori. 2002. Human Stx2-specific monoclonal antibodies prevent systemic complications of Escherichia coli O157:H7 infection. Infect. Immun. 70:612-619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mukherjee, J., K. Chios, D. Fishwild, D. Hudson, S. O'Donnell, S. M. Rich, A. Donohue-Rolfe, and S. Tzipori. 2002. Production and characterization of protective human antibodies against Shiga toxin 1. Infect. Immun. 70:5896-5899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Myers, E. W., and W. Miller. 1988. Optimal alignments in linear space. Comput. Appl. Biosci. 4:11-17. [DOI] [PubMed] [Google Scholar]
- 21.Nakao, H., C. Kataoka, N. Kiyokawa, J. Fujimoto, S. Yamasaki, and T. Takeda. 2002. Monoclonal antibody to Shiga toxin 1, which blocks receptor binding and neutralizes cytotoxicity. Microbiol. Immunol. 46:777-780. [DOI] [PubMed] [Google Scholar]
- 22.Nakao, H., N. Kiyokawa, J. Fujimoto, S. Yamasaki, and T. Takeda. 1999. Monoclonal antibody to Shiga toxin 2 which blocks receptor binding and neutralizes cytotoxicity. Infect. Immun. 67:5717-5722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paton, J. C., and A. W. Paton. 1998. Pathogenesis and diagnosis of Shiga toxin-producing Escherichia coli infections. Clin. Microbiol. Rev. 11:450-479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shimizu, H., R. A. Field, S. W. Homans, and A. Donohue-Rolfe. 1998. Solution structure of the complex between the B-subunit homopentamer of verotoxin VT-1 from Escherichia coli and the trisaccharide moiety of globotriaosylceramide. Biochemistry 37:11078-11082. [DOI] [PubMed] [Google Scholar]
- 25.Smith, M. J., L. D. Teel, H. M. Carvalho, A. R. Melton-Celsa, and A. D. O'Brien. 2006. Development of a hybrid Shiga holotoxoid vaccine to elicit heterologous protection against Shiga toxins types 1 and 2. Vaccine 24:4122-4129. [DOI] [PubMed] [Google Scholar]
- 26.Strockbine, N. A., L. R. Marques, R. K. Holmes, and A. D. O'Brien. 1985. Characterization of monoclonal antibodies against Shiga-like toxin from Escherichia coli. Infect. Immun. 50:695-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strockbine, N. A., L. R. Marques, J. W. Newland, H. W. Smith, R. K. Holmes, and A. D. O'Brien. 1986. Two toxin-converting phages from Escherichia coli O157:H7 strain 933 encode antigenically distinct toxins with similar biologic activities. Infect. Immun. 53:135-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tarr, P. I., C. A. Gordon, and W. L. Chandler. 2005. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet 365:1073-1086. [DOI] [PubMed] [Google Scholar]
- 29.Thompson, G. S., H. Shimizu, S. W. Homans, and A. Donohue-Rolfe. 2000. Localization of the binding site for the oligosaccharide moiety of Gb3 on verotoxin 1 using NMR residual dipolar coupling measurements. Biochemistry 39:13153-13156. [DOI] [PubMed] [Google Scholar]
- 30.Tzipori, S., H. Karch, K. I. Wachsmuth, R. M. Robins-Browne, A. D. O'Brien, H. Lior, M. L. Cohen, J. Smithers, and M. M. Levine. 1987. Role of a 60-megadalton plasmid and Shiga-like toxins in the pathogenesis of infection caused by enterohemorrhagic Escherichia coli O157:H7 in gnotobiotic piglets. Infect. Immun. 55:3117-3125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tzipori, S., A. Sheoran, D. Akiyoshi, A. Donohue-Rolfe, and H. Trachtman. 2004. Antibody therapy in the management of Shiga toxin-induced hemolytic uremic syndrome. Clin. Microbiol. Rev. 17:926-941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tzipori, S., I. K. Wachsmuth, C. Chapman, R. Birden, J. Brittingham, C. Jackson, and J. Hogg. 1986. The pathogenesis of hemorrhagic colitis caused by Escherichia coli O157:H7 in gnotobiotic piglets. J. Infect. Dis. 154:712-716. [DOI] [PubMed] [Google Scholar]
- 33.Wen, S. X., L. D. Teel, N. A. Judge, and A. D. O'Brien. 2006. A plant-based oral vaccine to protect against systemic intoxication by Shiga toxin type 2. Proc. Natl. Acad. Sci. USA 103:7082-7087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wen, S. X., L. D. Teel, N. A. Judge, and A. D. O'Brien. 2006. Genetic toxoids of Shiga toxin types 1 and 2 protect mice against homologous but not heterologous toxin challenge. Vaccine 24:1142-1148. [DOI] [PubMed] [Google Scholar]
- 35.Yamagami, S., M. Motoki, T. Kimura, H. Izumi, T. Takeda, Y. Katsuura, and Y. Matsumoto. 2001. Efficacy of postinfection treatment with anti-Shiga toxin (Stx) 2 humanized monoclonal antibody TMA-15 in mice lethally challenged with Stx-producing Escherichia coli. J. Infect. Dis. 184:738-742. [DOI] [PubMed] [Google Scholar]