Abstract
We provide a framework for health services–related researchers, practitioners, and policy makers to guide future health disparities research in areas ranging from detecting differences in health and health care to understanding the determinants that underlie disparities to ultimately designing interventions that reduce and eliminate these disparities. To do this, we identified potential selection biases and definitions of vulnerable groups when detecting disparities.
The key factors to understanding disparities were multilevel determinants of health disparities, including individual beliefs and preferences, effective patient–provider communication; and the organizational culture of the health care system. We encourage interventions that yield generalizable data on their effectiveness and that promote further engagement of communities, providers, and policymakers to ultimately enhance the application and the impact of health disparities research.
Eliminating disparities in health and health care is a priority identified in the US Department of Health and Human Services’ Healthy People 2010 initiative.1 Health care organizations such as the Veterans Health Administration (VHA) also have identified disparities as a key focus of their medical, social, and research missions.2 Although many health services researchers have addressed health disparities among vulnerable populations, there are currently no comprehensive frameworks to follow for advancing a research agenda within the context of the health care system. We describe a framework for guiding future health disparities research that can be used by researchers, clinicians, managers, and policymakers within the health care setting. Our framework outlines a research trajectory from basic detection of disparities in health and health care to understanding the factors that underlie those disparities to ultimately developing and implementing interventions designed to reduce and eliminate those disparities.
THREE PHASES OF HEALTH DISPARITIES RESEARCH
Our framework organizes the process of health disparities research into 3 phases: detection, understanding, and reduction or elimination. This framework’s origins are in epidemiology, which Last defined as “the study of the distribution [detection] and determinants [understanding] of health-related states or events in defined populations, and the application of this study to the control of health problems [reduction/elimination].”3(p42) Figure 1 ▶ shows the progressive nature of health disparities research and the key issues and challenges associated with each phase. The first phase, detectionsecond phase of health disparities research, understanding why disparities exist, involves identifying factors that explain gaps in health and health care between vulnerable and less vulnerable groups. The third phase of research involves the development, implementation, and evaluation of interventions that reduce or eliminate health and health care disparities.
FIGURE 1—
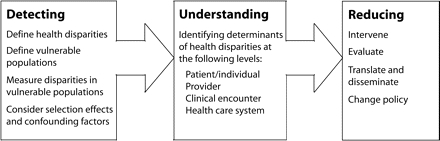
The 3 phases of the disparities research agenda.
Note. In our framework, the health disparities research agenda progresses in 3 sequential phases of research. Phase 1 (detecting disparities) informs phase 2 studies (understanding disparities), which in turn informs phase 3 research (interventions to reduce or eliminate disparities).
We will describe the theoretical origins of this framework and the key conceptual and methodological issues each phase of health disparities research must consider when designing disparities studies. Specifically, we will identify areas in need of more research and more effective strategies for conducting health disparities research from the standpoint of health care researchers, practitioners, administrators, and policymakers.
Background and Theoretical Underpinning
As research on health and health care disparities becomes increasingly sophisticated, there is an ever-greater need for delineating a comprehensive research agenda. The majority of current research has focused on documenting health disparities or outlining their underlying causes,4–8 and little work in current disparities research has focused on identifying the key methodological issues (e.g., measurement of vulnerability).7 Although some disparities can be explained by underlying differences in disease severity or health care access among individuals within vulnerable and less vulnerable groups, such differences do not completely explain persistent gaps in health and health care.9
We need a more comprehensive framework for advancing the field of disparities research from detection and understanding to designing interventions that will reduce or eliminate health disparities, specifically within the realm of the health care setting. Stewart and Nápoles-Springer described 2 types of health disparities frameworks: one that takes a more global—or public health—approach by outlining the social determinants of health and another that focuses on the health care system.7 In contrast to public health–based frameworks, which focus on causes of disparities within communities or society,8 our framework focuses on research within the context of the health care system, because it is here that health care researchers, practitioners, and policymakers have the greatest opportunities for reducing or eliminating differences in quality of health care.
Our framework differs from existing frameworks in that (1) it focuses on the health care system, (2) it provides a more precise definition of vulnerable groups, and (3) it provides a road map for moving the disparities research agenda forward. At the same time, we acknowledge the importance of factors outside the health care system that can contribute to health disparities, such as the environment and the political economy.8 Still, unanswered questions remain about the role of health services factors as both causes of and solutions to heath disparities, notably the roles of patient, provider, and health care organizational factors.
PHASE 1: DETECTION
The observation that certain segments of the population receive a lower quality of care (defined by health care processes or health outcomes) compared with less vulnerable segments is the foundation of health disparities research. It also is the focus of the majority of work to date in this field. Although this work is often conceptually simple, the definition of health disparities and the selection of study populations are often determined on the basis of unstated assumptions. Definitions of health disparities are not always consistent, and the selected comparison groups often do not reflect a priori knowledge or hypotheses. Therefore, we will propose a thorough definition of disparities and vulnerable populations and will then discuss methodological issues associated with the detection of disparities.
What Is a Health Disparity?
We define health disparities as observed clinically and statistically significant differences in health outcomes or health care use between socially distinct vulnerable and less vulnerable populations that are not explained by the effects of selection bias. The requirement of statistical significance provides increased measurement objectivity that is critical for empirical research and for drawing valid conclusions from the observed evidence.10
Our definition of health disparities was made on the basis of definitions proposed by Rathore and Krumholz11 and the Institute of Medicine’s Unequal Treatment report.9 However, we expanded these definitions of health disparities to include differences in health outcomes or health status (e.g., life expectancy, medical outcomes of acute and chronic illnesses) and health care use (i.e., differences in quality or receipt of care). Observed differences in health outcomes or health status represent inequalities, or measurable gaps between groups. These disparities in health outcomes or health status may be caused or exacerbated by patient, provider, or system-level factors that result in differential treatment (i.e., receipt of health care) or by societal inequities such as differential power or socioeconomic status (SES). It is therefore important that health care researchers understand and examine how underlying individual, provider, and system-level or organizational factors influence health and health care disparities.
Disparities as Gaps in Quality
Health disparities also reflect gaps in the quality of care delivered.9 In this context, disparities in quality of care imply underperformance of processes of care considered to be best practices or inferior health care outcomes among a vulnerable population.12,13 Defining health disparities as gaps in quality of care provided may offer a particularly important framework for researchers interested in detecting disparities, because health care administrators and policymakers are increasingly embracing evidence-based performance measures as tools for detecting gaps in quality of care, and they are using such measures to leverage performance improvement.14 Hence, disparity studies that focus on the detection of potential gaps in the quality of care provided can be a particularly powerful approach, because this concept resonates with health care providers and leaders. Consequently, some researchers have encouraged the development of quality measures designed to monitor disparities in the quality of health care between subpopulations.15
Consider Selection Effects
Our definition also rules out selection effects, which can lead to confounding or observed but not necessarily true differences in health care quality or outcomes between groups. The effects of selection bias are not well understood and are sometimes difficult to reconcile with previous findings. For example, Jha et al. found that among VA inpatients with cardiovascular disease, African Americans experienced lower mortality compared with Whites.16 This result appears to be a disparity paradox that contradicts previous observations that Whites tend to have better medical outcomes compared with African Americans. Perhaps African Americans faced higher access barriers to care outside the VA Health Care System compared with Whites; therefore, VHA use may occur earlier among African Americans and thus lead to a less severely ill study population—selection characteristics that may remain unmeasured and inadequately adjusted for in analyses of health care outcomes. Simultaneously, perhaps Whites approach the VHA for care at a much later stage of illness when all other health care options are exhausted. When detecting disparities, it is therefore important to consider whether the origin of the disparity is attributable to selection or illness severity differences between vulnerable and less vulnerable patients.
Disparities in Patient Preferences
Rathore and Krumholz11 and the Institute of Medicine9 did not include observed differences in access to care or patient preferences as part of their definition of disparities. By contrast, we consider disparities that arise from these 2 factors as potentially worthy of remediation. For example, it is important to consider reasons for a given preference of care and to distinguish between preferences that represent deeply held beliefs that are based on codified cultural or religious traditions from more transient beliefs that are based on unequal access to health care information or popular health myths. Although it is always useful to understand patient preferences, it is important to note that patient preferences should not be regarded as sacrosanct and that some preferences may be appropriately amenable to intervention and change.
Vulnerable Populations
Moreover, our definition of disparities also requires that the disparity occur in a vulnerable population. In contrast to the Institute of Medicine report, which defines disparities as “racial or ethnic differences in the quality of health care. . . ”,9(p9) we define vulnerable populations more broadly than by race/ethnicity alone.
We define vulnerable populations as groups that have faced discrimination because of underlying differences in social status, which can lead to potential gaps in health or health care. Our definition of a vulnerable population is similar to the one proposed by Aday,10 that is, subpopulations who are “at risk of poor physical, psychological, and/or social health”10(p5) because of differences in underlying social status owing to race/ ethnicity, gender, and so on. Social status is part of the underlying definition of vulnerability, because differences in social status are “made manifest in the differential availability of personal and political power and associated human and social capital resources to different subgroups.”10(p5) Defining vulnerable groups on the basis of underlying social status highlights the essential social roots of discrimination experienced by certain groups, and it lends credence to the often implicit role of restitution in sustaining the health disparity research agenda.
The issue of defining vulnerable populations in the context of health disparities was included in recent proposals by the US Congress to amend the Public Health Service Act. In particular, the definition of “health disparity populations” proposed in Senate Bill 2091 modifies the original designation of vulnerable populations in the Public Health Service Act from “underrepresented minority individuals” to “racial or ethnic minorities or health disparity populations.” 17 Under this proposal, a population is a health disparity population if there is “a significant disparity in the overall rate of disease incidence, prevalence, morbidity, mortality, or survival rates in the population as compared with the health status of the general population.”17 This bill noted that the reason for including this broader definition is because the largest numbers of medically underserved individuals are lower-SES Whites, even though there is a higher proportion of racial/ethnic minorities among the medically underserved.17 This broad definition is consistent with our proposed definition of vulnerable groups and definitions proposed by the National Institutes of Health and the VHA. Both consider characteristics other than race/ ethnicity, such as membership in traditionally underserved groups (e.g., inhabitants of Appalachia, under the National Institutes of Health definition, and women and rural populations, under the VHA definition), permanent disability, cohorts defined by shared military status (e.g., Gulf War veterans), and living conditions that pose special challenges to health care delivery (e.g., homeless, institutionalized, or homebound patients).
Defining Vulnerable Populations
The definition we propose assumes that underlying bias and discrimination are experienced by groups other than those defined by race/ethnicity alone, including those defined by socioeconomic—or class—differences. Isaacs and Schroeder argued that socioeconomic position (i.e., class) should be considered when defining vulnerable populations, because it may explain disparities above and beyond race/ethnicity alone. For example, in the United States, differences in heart disease death rates are greater between higher-SES and lower-SES individuals compared with the differences between Whites and African Americans.18 Moreover, recent evidence has suggested that class mobility has stalled for some segments of the US population19; hence, class differences may reflect permanent and underlying differences in social status.18
By contrast, Williams suggested that underlying differences in social status are chiefly felt by racial/ethnic minorities—independent of class—because of their experience with racism, bias, and discrimination throughout US history. 20 Williams argued that racism is still an underlying driving force in determining economic opportunities for minorities because of historical bias and discrimination and stigma of inferiority, which can in turn adversely affect health by restricting socioeconomic opportunities and mobility.
Nonetheless, Isaacs and Schroeder18 and Williams20 advocated for better measures of class and racism and for future research that better elucidates the association between class, racism, and health outcomes. One reason for the lack of comprehensive studies on class and health disparities is that measures of class have not been fully developed; education, income, and employment serve as limited proxies at best. Although researchers in Great Britain distinguish people by social class (ranked I–V) on the basis of public records, in the United States, a similar method would be limited because variations in other important class markers, such as education, acculturation, and wealth, exist within employment strata.
The debate about whether to include class within the definition of vulnerable populations can be reduced to the question of whether vulnerability is defined only on the basis of historical experiences of bias and discrimination or whether vulnerability can be considered independent of historical experiences. Many groups may currently experience bias and discrimination (e.g., the homeless, recent immigrants); however, such experiences depend on their current social status, which may change over time. This distinction is important because historical vulnerability and more transient vulnerability may have different sets of underlying characteristics and thus may require different types of interventions. Although our core definition of vulnerability clearly includes individuals who have historically experienced ongoing bias and discrimination, we also include those who have more transient vulnerability, such as those who have limited economic or social resources. Thus, it is important to understand and study both underlying vulnerable group status (e.g., subpopulations with a history of ongoing bias and discrimination) and potentially mutable factors of vulnerability brought forth by differences in social or human capital (e.g., family, social networks, income, education) in order to inform future research.
It is likely that the definition of vulnerable populations will evolve as the field of health disparities research progresses and as new underserved communities and subpopulations are identified. There is growing consensus that groups can be discriminated against on the basis of a broad range of characteristics, including sexual orientation, religious affiliation, degree of acculturation, and stigmatizing health conditions such as mental illness.10 This more flexible definition therefore leaves room for the inclusion of new subpopulations that also may face discrimination but have not been recognized to date.
PHASE 2: UNDERSTANDING
Understanding disparities involves identifying the potential determinants of gaps in health or health outcomes between vulnerable and less vulnerable groups, which in turn can inform interventions that reduce or eliminate these differences.21,22 We encourage a more comprehensive study of potential determinants (mediators and moderators)23 that might explain the associations between vulnerability and health disparities that cut across multiple levels.
Considering Multilevel Factors
Figure 2 ▶ shows key potential determinants of health disparities from the perspective of health services researchers, including individual, provider, and health care system factors. This view is consistent with Stewart and Nápoles-Springer, who emphasized the need for assessing underlying determinants such as individual preferences, provider factors, and the organization and delivery of care at the practice or health system level.7
FIGURE 2—
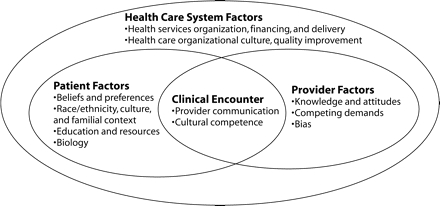
Understanding the origins of health and health care disparities from a health services research perspective: key potential determinants of health disparities within the health care system, including individual, provider, and health care system factors.
Individual factors, such as race/ethnicity, culture, education, and SES, are all important when seeking to understand the origins of health disparities. To date, most health services research has focused on the role of these individual factors21 and, to a lesser extent, on emerging issues such as individual preferences or possible biological or genetic factors. Moreover, provider factors—including knowledge, attitudes, bias, and even financial incentives—also influence health or health care disparities. Providers in particular may be vulnerable to subconscious processes such as bias or stereotyping, especially within busy health care settings,24 which in turn can adversely affect patient engagement in care. Although the clinical encounter is a key focal point for understanding disparities, fundamental aspects of the health care system (e.g., organization, financing, delivery) also are likely to play a role in explaining disparities. The next 4 sections highlight some of the emerging potential determinants of health disparities: individual preferences, biological factors, provider factors, and health care organizational culture.
Individual Preferences
The role individual preferences play in influencing the medical care received has received increasing attention. Individual cultural beliefs and familial experiences are known to influence individual preferences about health care access and outcomes. Historically, most health promotion interventions have focused on changing patient preferences—especially when such preferences preclude individuals from seeking needed medical care—unless such preferences are determined on the basis of weighing the pros and cons of a risky procedure. Recently, there has been a growing realization of the need to differentiate between patient preferences that are grounded in ethnicity or culture, that is, long-standing cultural traditions or deeply held and well-codified beliefs about health and medical treatment, from those that are grounded in modifiable perceptions or even misleading information, such as urban legends or popular myths that arise from unequal access to health care information. For example, Jehovah’s Witnesses may choose not to have curative surgery because, on the basis of their religious beliefs, they are unable to receive blood transfusions. By contrast, some African Americans choose not to have potentially curative lung cancer surgery because of the myth that the surgery and the concomitant exposure of the tumor to oxygen may cause the cancer to spread.25 Thus, understanding the root causes of patient preferences is important when determining the appropriateness of an intervention and when tailoring interventions that address underlying patient beliefs.
At the same time, it also is important to consider the potential that providers may stereotype patients who hold beliefs that contrast with standard medical practice. Providers may assume patients hold beliefs about certain treatments because of their racial/ ethnic background when in fact they do not. Such stereotyping may lead to inappropriate withholding of care on the basis of an assumption that certain groups would not want more aggressive therapy.24 The balance to be struck between a desire to change patient preferences on the basis of beliefs that may not coincide with standard medical care versus accepting and acting medically in concordance with such beliefs has important implications for the assumptions that are made about disparities and the development of interventions aimed at reducing disparities.
Biology and Genetics
The recent sequencing of the human genome has generated marked interest in studying the potential genetic determinants of health outcomes. Although underlying genetic makeup may eventually be found to affect a number of health outcomes, could it also explain underlying health disparities between vulnerable and less vulnerable populations? With the exception of specific genes attributed to diseases such as sickle-cell anemia, Tay-Sachs disease, and cystic fibrosis, differences in genetic makeup have not been found to explain health disparities between vulnerable and less vulnerable groups on the basis of race/ethnicity. Thus, Horn and Beal argued that race/ethnicity should only be studied as a social construct (i.e., representing underlying social and cultural factors) rather than as a biological construct.8
Still, recent evidence suggests that biological or genetic differences in race/ethnicity could lead to different treatment responses and thereby affect health outcomes. One such study, the African American Heart Failure Trial26 suggested that African Americans were less likely than were Whites to respond to common heart failure medications. The study also found that combining 2 drugs (isosorbide dinitrate and hydralazine) for heart failure reduced 1-year mortality by 43% among African Americans.26 Nonetheless, this study was controversial because no genetic analysis was performed. Furthermore, only African Americans were enrolled in the study; hence, differential effects between racial/ethnic groups could not be assessed.
Although the African American Heart Failure Trial has been praised for broadening the inclusiveness of clinical trials, most of which are conducted with White males,27 the debate continues as to whether such research truly enhances the understanding of disparities or merely strengthens misleading views of race/ ethnicity and health behaviors as purely biological concepts.28,29 There also is growing concern about the use of genetic information at the health system level (e.g., by insurance companies) to “redline” individuals (i.e., make them uninsurable on the basis of genetic risk for disease), even though genetic information at best predisposes an individual to a greater risk for the disease rather than directly causes the disease. Overall, more sophisticated research that differentiates individuals by meaningful genetic markers—and not just by skin color—is needed.
Provider Factors
Emerging research suggests that provider factors, notably potential stereotyping by providers of patients from different racial/ethnic groups,24 and patient–provider communication problems are important contributors to health disparities. Evidence suggests that elderly African Americans are less likely to receive lung cancer surgery compared with Whites, even after control for socioeconomic factors, access to care, and clinical severity.30 This finding may be attributed to barriers in communication between patients and providers: African American patients may feel less engaged with their care or less included in the decisionmaking process compared with Whites, which in turn can lead to mistrust in treatment procedures24,31 and may reinforce the aforementioned beliefs about oxygen exposure and lung cancer.25
Lack of engagement in treatment among patients and subsequent suboptimal care may be attributed to provider communication style.5,32,33 For example, in a study that analyzed taped conversations between providers and patients, providers were more likely to communicate in a verbally dominant manner with their African American patients compared with their White patients.33 Poor communication can lead to patient mistrust of the provider and subsequent refusal of treatment. Moreover, providers may fail to consider the patient’s culture within the clinical encounter and subsequently fail to appropriately tailor messages about health promotion or disease prevention (i.e., cultural competence).32 Hence, experts have identified improving patient–provider communication and provider training in cultural competence as key targets for improving patient trust and reducing health disparities.5
Health Care Organizational Culture
Health care organizational factors are increasingly being recognized as important determinants of health disparities.16 A growing body of research suggests that disparities in the receipt of preventive care among minorities compared with Whites are attributable to organizational characteristics, including location, resources, and complexity of a clinic or practice. One of the pioneering studies that examined the role of health care system factors was the Medical Outcomes Study,34 which assessed whether variations in processes and outcomes of care were explained by differences in types of health care systems (health maintenance organization vs fee-for-service)35 and provider factors.36 In particular, health care system type was significantly associated with differences in patient use and outcomes.35,37
Beyond the type of health care system, other organizational factors have been suggested to be determinants of patient health care use and outcomes, including coordination, continuity, and comprehensiveness of services delivered.38 These factors are potentially more mutable than health care system type, and more research is needed to determine whether differences in specific organizational features influence health disparities. Until recently, the lack of comprehensive multisite data on patients and facilities precluded a rigorous and quantitative analysis of health care organizational factors. However, the growing body of evidence that suggests organizational factors play an important role in health disparities has prompted more in-depth research on the role of key mutable organizational processes across treatment settings.39–41
Simultaneously, health care organizations are increasingly being held accountable for improving quality of care. This has led to more sophisticated studies that identify health system factors that may act as barriers or facilitators to quality of care and, ultimately, health or health care disparities. Emerging research from the VHA—a closed health care system that has the capacity to conduct national assessments of health care practices, providers, and patients—suggests that specific organizational features, including management, staffing, and organizational culture, may explain differences in health care quality and outcomes.39,40 Moreover, activities that signify a “quality improvement culture,” such as the use of clinical reminders, were associated with improved diabetes-related outcomes.40 Organizational culture, especially one that provides incentives and mechanisms for quality improvement, also may improve the provision of culturally appropriate and equitable care.41,42 The availability of culturally appropriate services, including tailored self-management programs and linkages to community resources (e.g., faith-based programs),42,43 also may contribute to reduced disparities and should be considered when assessing organizational features and culture.
Ultimately, when designing and conducting phase 2 research, it is critical to identify particular mechanisms that can be acted upon to reduce or eliminate the disparity. Some determinants of disparities (e.g., knowledge, communication) may be more amenable to intervention than are other disparities (e.g., religious beliefs, familial context). One of the key challenges of this research phase is to determine what can be modified through patient-based, provider-based, and health system–based interventions and thus directly inform phase 3 research.
PHASE 3: REDUCING DISPARITIES
Phase 3 of our proposed research agenda is the development and implementation of interventions that reduce or eliminate disparities in health or health care. This phase is the least well represented in the literature. Four issues are important at this stage: (1) developing appropriate intervention strategies, especially for community-based settings that serve vulnerable populations, (2) instituting appropriate evaluation techniques, (3) determining whether a strategy for reducing disparities is ready for implementation and translation into routine care settings, and (4) developing strategies that promote policy changes on the basis of the intervention.
Developing Interventions
Interventions that reduce or eliminate disparities are designed on the basis of findings from phase 2 research during which potential explanatory factors of disparities are identified. Some key interventions to date that have been successful in reducing health disparities shared 2 common features: they were customized a priori to address the origins of health disparities among their target population (i.e., individual, provider, or system-level factors among a vulnerable group), and they used state-of-the-art methods of implementation among specific vulnerable groups (e.g., involved community-based settings, were offered at convenient times, allowed consumer choice). Notably, an intervention for improving diabetes-related outcomes had tailored education sessions for individuals with low health literacy.44 A depression care management program was found to be equally effective among Whites and minorities alike, perhaps because the intervention encouraged patient choice and offered culture-specific services (e.g., provider cultural competency training, interpreters).45 Another intervention for reducing HIV risk behaviors among African American women was designed to promote confidence in sexual decisionmaking through communication skills and ethnic pride.46 Although by no means a comprehensive review of effective interventions, these studies are examples of effective approaches that reduce or eliminate health disparities.
Although randomized controlled trials have been considered the gold standard in clinical studies,5 there is increasing debate about whether randomized controlled trials are appropriate for all research settings and whether they can adequately assess the effects of multilevel provider or system-level changes on health care and outcomes. Additionally, there is concern about the limited external validity of randomized controlled trials,47 because they are designed for ideal controlled settings that may not be generalizable to a broader and more representative sample of individuals or community-based practices.48,49 Moreover, because of historical experiences with research, such as the Tuskegee Syphilis Study experiment, vulnerable groups (in this case African Americans) may be reluctant to participate in research that requires randomization.50 Providers in the community also may be reluctant to participate if they perceive the intervention as a threat to or a judgment of their practice or if they feel that their patients are being “used” for research.51
Nonetheless, randomized controlled trials ensure the best opportunity for participants to have an equal opportunity for receiving the intervention. Alternatively, interventions could be randomized at the health care practice or site level, rather than the patient level, which may be more appealing to community-based providers and consumer advocates who elect to participate. Other alternative approaches, such as nonequivalent control group designs (e.g., interrupted time-series designs) also allow for a more representative inclusion of individuals, providers, and communities, but these approaches have their own limitations in that designers cannot fully control for selection effects, confounding, or historical trends.
Evaluation
Evaluation is an important component of the intervention process.17 Data generated from the performance of an intervention are important for ultimately making the business case at the policy level to sustain and improve such interventions in the future. When making the business case, researchers may want to invest in a program evaluation approach.47 Program evaluation involves the systematic collection and analysis of information on all aspects of the program, and it has been used to assess the impact of demonstration programs that involve multilevel interventions.44 Evaluating the intervention process involves collecting data from all parties involved (e.g., participants, providers, communities) on the feasibility and acceptance of the intervention and identifying potential barriers to and facilitators of the intervention.
Information on the intervention’s performance can be qualitative as well as quantitative in nature. Health services researchers are increasingly integrating qualitative techniques with quantitative data-driven findings to enrich and inform the dialog between researchers and community members. Qualitative information not only assists health services researchers with better understanding the underlying determinants of health disparities but also informs the degree to which an intervention was successful and accepted by participants. Crabtree and Miller52 described 3 types of qualitative research techniques that could be applied to health disparities research: observational qualitative research (e.g., mapping out relationships, journals), interviewing (e.g., focus groups, semistructured one-on-one interviews), and material culture assessment (e.g., archives, storytelling). For example, unstructured interviews allow researchers to gather information from health care leaders and community representatives about the barriers to and facilitators of a program’s success. Semistructured interviews or storytelling can be used to generate hypotheses about why an intervention was or was not successful (e.g., a walk-through of an individual’s experience with the program). Hence, qualitative studies can complement the quantitative data that is gathered as part of the intervention.
Ultimately, a key aspect of the evaluation is to ensure that feedback about the intervention is disseminated back to patients, providers, and community members. It is important to encourage ongoing engagement with patients, providers, and community representatives throughout the evaluation process so that they can provide input on key measures, interpretations of the results, and dissemination of findings.51
Implementation and Translation
The next issue is determining whether a strategy for reducing disparities is ready for implementation and translation into routine care beyond the initial intervention trial. A useful framework for determining whether an intervention is ready for broader translation is provided by the VHA Quality Enhancement Research Initiative Framework.53 This framework specifically outlines steps for translating evidence-based strategies that improve care and outcomes: (1) implement quality improvement programs across different sites by developing toolkits (i.e., training manuals, outcomes measures), (2) evaluate the implementation effort, and (3) further refine the intervention for wider dissemination.
Overall, the key to widespread translation of phase 3 health disparities research is customizing and adapting interventions for vulnerable groups and ensuring adequate resources and technical assistance for the evaluation.51 Successful adaptation can be facilitated with input from community members and the providers who serve them. In fact, researchers have often benefited from community-based collaborations, because community members often develop creative and innovative strategies for adapting the intervention to local settings.51
Researcher–Community Collaborations
Although interventions designed to reduce disparities can be successful in the realm of the health care setting, in many cases the translation, dissemination, and eventual sustainability of an intervention could be hindered because of underlying causes of disparities at the community or policy levels. Sustaining interventions may therefore involve changes at these levels, such as the financing or organization of health systems, changes in current laws at the local or national level, or changes in policies that promote economic growth or community development. Nonetheless, there is growing debate about what researchers can and should do within this policy realm. Researchers have been increasingly called on to become advocates for change not only in health care but also in the social determinants of health beyond the research setting—either through community outreach or political activism—in order to reduce the research–practice gap. Although research in this area has not traditionally sought to affect change at the broadest policy levels (e.g., training/distribution of health care personnel, education reform), findings from such projects often have implications for policy change. It is for this reason that we believe it is critical for researchers to collaborate and communicate with policymakers and communities about the policy implications of research findings.53
One way to reconcile these perspectives is to have researchers become more familiar with the policy arena by learning which key stakeholders can leverage support for programs that reduce disparities and then engaging such individuals at the beginning of the research program to garner their support for the policy change.53 Although many of the underlying causes of disparities often occur outside the health care system, researchers engaged with community members, providers, and policymakers still have the potential to address and intervene on the root causes of disparities. Notably, funding agencies have increasingly called on researchers to engage in community-based participatory research programs as a way of understanding the origins of disparities and for implementing and sustaining interventions in the long run.54 Although this role through community engagement is more hands-on and not always familiar to researchers, building a strong relationship between researchers, communities, and policymakers throughout the research process is critical for meeting the goal of reducing disparities. Communities and policymakers will benefit from better data on health outcomes and, in many cases, are more than willing to work with researchers to improve the collection and interpretation of health data.4
CONCLUSIONS
We described a research road map for detecting, understanding, and reducing or eliminating health and health care disparities that can be useful to investigators engaged in this area of research. When detecting disparities, researchers should consider potential selection biases and be precise when defining disparities or vulnerable groups. In this effort, researchers are encouraged to assess the multilevel determinants of health and health care disparities, including individual, provider, and organizational factors, to better understand the root causes of disparities. Finally, when developing and implementing interventions designed to reduce and eliminate disparities, researchers should consider study designs that yield generalizable data on the effectiveness of the intervention and encourage participation of vulnerable populations. Ultimately, researchers are encouraged to translate their intervention to different settings, disseminate their findings to communities, policymakers, and other stakeholders to maximize benefit in the field, and strengthen the policy implications of their work.
Acknowledgments
This research was supported by the Center for Health Equity Research and Promotion, VA Pittsburgh and VA Philadelphia Healthcare Systems (grant HFP01063). A. M. Kilbourne was funded by a Career Development Award Merit Review Entry Program (grant 02269) and a Merit Award from the VA Health Services Research and Development program (grant IIR 02–283). M. J. Fine was supported in part from a mid-career development award (5K24-AI01769-05) from the National Institute of Allergy and Infectious Diseases and by Project EXPORT (1P60-MD00207) from the National Center for Minority Health and Health Disparities.
We thank Harold Pincus and Judy Lave for comments on an earlier draft.
Note. The views expressed in this article are those of the authors and do not necessarily represent the views of the US Department of Veterans Affairs.
Human Participant Protection No protocol approval was needed for this study.
Peer Reviewed
Contributors A. M. Kilbourne developed the framework and supervised all aspects of the article. G. Switzer assisted with writing and editing the framework. K. Hyman synthesized the literature and assisted with further refining the framework. M. Crowley-Matoka provided substantial input on the social sciences literature pertaining to the framework. M. J. Fine originated the framework and assisted with the synthesis of its components and editing.
References
- 1.Thomas SB, Fine MJ, Ibrahim SA. Health disparities: the importance of culture and health communication. Am J Public Health. 2004;94:2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Dept of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: US Government Printing Office; 2000.
- 3.Last JM. A Dictionary of Epidemiology. New York, NY: Oxford University Press; 1988.
- 4.Brach C, Fraser I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev. 2000;57(suppl 1): 181–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braveman PA. Monitoring equity in health and health care: a conceptual framework. J Health Popul Nutr. 2003;21:181–192. [PubMed] [Google Scholar]
- 6.Cooper LA, Hill MN, Powe NR. Designing and evaluating interventions to eliminate racial and ethnic disparities in health care. J Gen Intern Med. 2002;17: 477–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stewart AL, Nápoles-Springer AM. Advancing health disparities research: can we afford to ignore measurement issues? Med Care. 2003;41:1207–1220. [DOI] [PubMed] [Google Scholar]
- 8.Horn IB, Beal AC. Child health disparities: framing a research agenda. Ambul Pediatr. 2004;4: 269–275. [DOI] [PubMed] [Google Scholar]
- 9.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington DC: National Academy Press; 2002. [PMC free article] [PubMed]
- 10.Aday LA. At Risk in America: The Health and Health Care Needs of Vulnerable Populations in the United States. San Francisco, Calif: Jossey-Bass, 1993:1–7.
- 11.Rathore SS, Krumholz HM. Differences, disparities, and biases: clarifying racial variations in health care use. Ann Intern Med. 2004;141:635–638. [DOI] [PubMed] [Google Scholar]
- 12.Donabedian A, Wheeler JR, Wyszewianski L. Quality, cost, and health: an integrative model. Med Care. 1982;20:975–992. [DOI] [PubMed] [Google Scholar]
- 13.Wyszewianski L, Donabedian A. Equity in the distribution of quality of care. Med Care. 1981; 19(suppl 12):28–56. [DOI] [PubMed] [Google Scholar]
- 14.Lurie N. Addressing health disparities: where should we start? Health Serv Res. 2002;37:1125–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Braveman PA, Egerter SA, Cubbin C, Marchi KS. An approach to studying social disparities in health and health care. Am J Public Health. 2004;94: 2139–2148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jha AK, Shlipak MG, Hosmer W, et al. Racial differences in mortality among men hospitalized in the Veterans Affairs health care system. JAMA. 2001;285: 297–303. [DOI] [PubMed] [Google Scholar]
- 17.US Congress. Senate Bill 2091. Health Care Equality and Accountability Act. Section 903 a 1. Available at: http://thomas.loc.gov/cgi-bin/query/z?c109:S.16. Accessed February 12, 2004.
- 18.Isaacs SL, Schroeder SA. Class—the ignored determinant of the nation’s health. N Engl J Med. 2004;351: 1137–1142. [DOI] [PubMed] [Google Scholar]
- 19.Wessel D. As rich-poor gap widens in the US, class mobility stalls. Wall Street Journal. May 13, 2005. Available at: http://online.wsj.com/article_print/0,SB111595026421432611,00.htm. Accessed August 22, 2005.
- 20.Williams DR. Race/ethnicity and socioeconomic status: measurement and methodological issues. Int J Health Serv 1996;26:483–505. [DOI] [PubMed] [Google Scholar]
- 21.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 22.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34:1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 23.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59: 877–883. [DOI] [PubMed] [Google Scholar]
- 24.Burgess DJ, Fu SS, van Ryn M. Why do providers contribute to disparities and what can be done about it? J Gen Int Med. 2004;19:1154–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Margolis ML, Christie JD, Silvestri GA, Kaiser L, Santiago S, Hansen-Flaschen J. Racial differences pertaining to a belief about lung cancer surgery: results of a multicenter survey. Ann Intern Med. 2003;139: 558–563. [DOI] [PubMed] [Google Scholar]
- 26.Taylor AL, Ziesche S, Yancy C, et al. African-American heart failure trial investigators. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. 2004;351:2049–2057. [DOI] [PubMed] [Google Scholar]
- 27.Freimuth VS, Quinn SC, Thomas SB, et al. African Americans’ views on research and the Tuskegee Syphilis Study. Soc Sci Med. 200;52:797–808. [DOI] [PubMed]
- 28.Fine MJ, Ibrahim SA, Thomas SB. The role of race and genetics in health disparities research. Am J Public Health. 2005;95:2125–2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cacioppo JT, Hawkley LC. Social isolation and health, with an emphasis on underlying mechanisms. Perspect Biol Med. 2003;46(suppl 3):S39–S52. [PubMed] [Google Scholar]
- 30.Bach PB, Cramer LD, Warren JL, Begg CB. Racial differences in the treatment of early-stage lung cancer. N Engl J Med. 1999;341:1198–1205. [DOI] [PubMed] [Google Scholar]
- 31.King TE Jr., Brunetta P. Racial disparity in rates of surgery for lung cancer. N Engl J Med. 1999;341: 1231–1233. [DOI] [PubMed] [Google Scholar]
- 32.Freimuth VS, Quinn SC. The contributions of health communication to eliminating health disparities. Am J Public Health. 2004;94:2053–2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient–physician communication during medical visits. Am J Public Health. 2004;94:2084–2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tarlov AR, Ware JE Jr, Greenfield S, Nelson EC, Perrin E, Zubkoff M. The Medical Outcomes Study. An application of methods for monitoring the results of medical care. JAMA. 1989;262:925–930. [DOI] [PubMed] [Google Scholar]
- 35.Greenfield S, Rogers W, Mangotich M, Carney MF, Tarlov AR. Outcomes of patients with hypertension and non-insulin dependent diabetes mellitus treated by different systems and specialties. Results from the medical outcomes study. JAMA. 1995;274:1436–1444. [PubMed] [Google Scholar]
- 36.Stewart AL, Sherbourne CD, Wells KB, et al. Do depressed patients in different reatment settings have different levels of well-being and functioning? J Consult Clin Psychol. 1993;61:849–857. [DOI] [PubMed] [Google Scholar]
- 37.Ware JE Jr, Bayliss MS, Rogers WH, Kosinski M, Tarlov AR. Differences in 4-year health outcomes for elderly and poor, chronically ill patients treated in HMO and fee-for-service systems. Results from the Medical Outcomes Study. JAMA. 1996;276: 1039–1047. [PubMed] [Google Scholar]
- 38.Safran DG, Tarlov AR, Rogers WH. Primary care performance in fee-for-service and prepaid health care systems. Results from the Medical Outcomes Study. JAMA. 1994;271:1579–1586. [PubMed] [Google Scholar]
- 39.Jackson GL, Yano EM, Edelman D, et al. Veterans Affairs primary care organizational characteristics associated with better diabetes control. Am J Manag Care. 2005;11:225–237. [PubMed] [Google Scholar]
- 40.Meterko M, Mohr DC, Young GJ. Teamwork culture and patient satisfaction in hospitals. Med Care. 2004; 42:492–498. [DOI] [PubMed] [Google Scholar]
- 41.Shortell SM, Zimmerman JE, Rousseau DM, et al. The performance of intensive care units: does good management make a difference? Med Care. 1994;32: 508–525. [DOI] [PubMed] [Google Scholar]
- 42.Cooper LA, Brown C, Vu HT, et al. Primary care patients’ opinions regarding the importance of various aspects of care for depression. Ann Gen Hosp Psychiatry. 2000;22:163–173. [DOI] [PubMed] [Google Scholar]
- 43.Substance Abuse and Mental Health Services Administration National Mental Health Information Center. Culture, race, and ethnicity—supplement. A report of the Surgeon General. Available at: http://www.mentalhealth.org/cre/toc.asp. Accessed October 15, 2004. [PubMed]
- 44.Rothman RL, DeWalt DA, Malone R, et al. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004;292:1711–1716. [DOI] [PubMed] [Google Scholar]
- 45.Miranda J, Duan N, Sherbourne C, et al. Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized controlled trial. Health Serv Res. 2003;38:613–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.DiClemente RJ, Wingood GM. A randomized controlled trial of an HIV sexual risk-reduction intervention for young African-American women. JAMA. 1995; 274:1271–1276. [PubMed] [Google Scholar]
- 47.Rossi P, Freeman H. Evaluation—A Systematic Approach. 5th ed. Thousand Oaks, Calif: Sage Publications, Inc; 1993.
- 48.Roy-Byrne PP, Sherbourne CD, Craske MG, et al. Moving treatment research from clinical trials to the real world. Psychiatr Serv. 2003;54:327–332. [DOI] [PubMed] [Google Scholar]
- 49.Kilbourne AM, Schulberg HC, Post EP, et al. Translating evidence-based depression management services to community-based primary care practices. Milbank Q. 2004;82:631–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Corbie-Smith G, Thomas SB, St George DM. Distrust, race, and research. Arch Intern Med. 2002;162: 2458–2463. [DOI] [PubMed] [Google Scholar]
- 51.Horowitz CR, Davis MH, Palermo AG, Vladeck BC. Approaches to eliminating sociocultural disparities in health. Health Care Financ Rev. 2000;21:57–74. [PMC free article] [PubMed] [Google Scholar]
- 52.Crabtree BF, Miller WL. Doing Qualitative Research. 2nd ed. Thousand Oaks, Calif: Sage Publications, Inc; 1999:15–18.
- 53.Rubenstein LV, Mittman BS, Yano EM, Mulrow CD. From understanding health care provider behavior to improving health care: the QUERI framework for quality improvement. Quality Enhancement Research Initiative. Med Care. 2000;38(6 suppl 1):I129–I141. [PubMed] [Google Scholar]
- 54.Agency for Healthcare Research and Quality. The role of community-based participatory research: creating partnerships, improving health. Available at: http:// www.ahrq.gov/research/cbprrole.htm. Accessed October 15, 2004.


