Abstract
This study examined the drug use patterns of pregnant women in two inner city sites, selected to overrepresent cocaine users. Women who used cocaine were much more likely to have used some combination of cigarettes, alcohol, and marijuana in addition to cocaine during pregnancy. There was little difference in the patterns of drug use in the two study sites, Trenton, New Jersey, and northwestern Philadelphia. A number of demographic and lifestyle variables of cocaine users, soft drug users (cigarettes, alcohol, and/or marijuana), and abstainers were compared. The cocaine-using group was significantly older and had more children, had less stable and more isolated living situations, was less likely to be employed and more likely to be receiving public assistance during pregnancy, and was more likely to have a higher drug- and alcohol-using social environment and family history than soft drug users or abstainers. Of significance was that many of the high-risk lifestyle factors exhibited by cocaine users were also seen, albeit to a lesser extent, among the soft drug users. These findings have implications for the timing of intervention strategies that would be most effective.
INTRODUCTION
Drug use continues to be a major problem in the United States. It is of particular concern when the user is a pregnant woman and the substances to which her fetus is exposed are known or suspected human teratogens. Cocaine, which is easily affordable and obtainable in the form of crack, readily crosses the placenta (1, 2). The incidence of cocaine use by women of childbearing age has been reported to be about 15% (3) and recent estimates range from 10% to 30% of women using during pregnancy in urban centers (4–9).
The biological mechanisms of the effect of cocaine on the developing central nervous system provide a theoretical basis for concern about the impact on later functional capacity. These include possibly permanent alteration of neurotransmitter activity due to direct actions of cocaine on the fetus’s brain, as well as indirect consequences of effects of cocaine on the peripheral circulation of the mother, leading to reduced oxygen delivery to the fetus’s brain (10–12). Some empirical support of long-term consequences of prenatal cocaine exposure is beginning to accrue (11, 13–15).
Soft drugs, especially alcohol, cigarettes, and marijuana, are frequently used during pregnancy, often in conjunction with cocaine (7, 16). Ample evidence supports the long-term developmental consequences of these prenatal exposures (17). Moreover, combinations of these substances may interact in the body to produce more dangerous teratogens (18).
The present study examined the substance use patterns of pregnant women in two inner-city samples selected to overrepresent cocaine users. In addition, the study determined demographic and lifestyle variables associated with different drug use patterns. The results have implications for timing and strategies of intervention.
METHODS
Subjects
The sample consisted of 323 pregnant women recruited between February 1993 and June 1994 for a longitudinal study of effects of prenatal cocaine exposure on child outcome. Pregnant women attending participating hospital-based prenatal clinics, or newly delivered women in Trenton, New Jersey, or northwestern Philadelphia were approached. Women were recruited at Mercer Medical Center in Trenton, one of the three hospitals in the city with an obstetrics service and the largest census (approximately 3,000 births/year). In Philadelphia, recruitment was conducted at the Medical College of Pennsylvania, one of six inner-city Philadelphia hospitals with an obstetrics service with a census comparable to the others (approximately 2,500 births/year). If a woman agreed to participate, she signed an informed consent form. She was then interviewed about prenatal substance use, demographic and lifestyle information. All interviews were conducted in an exam room at the hospital, in the mother’s room on the maternity ward if she had just delivered, in our laboratories near the hospitals, or in the woman’s home, within 2 weeks of the infant’s birth. A federal certificate of confidentiality backed up our guarantee that the study would not divulge confidential information obtained from the interviews. In addition, vouchers for purchase of goods and services in local stores were provided as incentives.
Substance use interview information was confirmed by results of prenatal and neonatal urine screens if available, and analysis of the newborns’ meconium. The infants’ meconium samples were screened using radioimmunoassay followed by confirmatory gas chromatography/mass spectrometry for the presence of benzoylecgonine (cocaine metabolite), cannabinoids, opiates, amphetamines, and phencyclidine. Twelve women who denied cocaine use were determined to have used cocaine by the meconium screen. Meconium samples were not available from the infants of 19 women who admitted cocaine use in the interview. Since the major focus of the research project was on the developmental consequences to the children of effects of prenatal cocaine exposure, opiate and phencyclidine users were excluded due to the confounds such exposure would introduce. There was very little phencyclidine use detected in either city during the period of recruitment. The proportion of the sample using cocaine is not representative of cocaine use during pregnancy in these cities since a special effort was made to recruit cocaine users. All subjects were inner-city clinic patients, predominantly African-American (89%), with 7% Caucasian, 2% Hispanic, and 1% Asian.
Measures
Meconium assays revealed information about only certain substances, and nothing about the form of cocaine, timing or quantity of use. This information was obtained through a semistructured interview currently being used by several federally funded studies of prenatal cocaine exposure around the country. These were conducted by trained interviewers—substance abuse counselors, or study personnel trained in substance use interview techniques by the counselors—and a clinical psychologist. The drug use interview contained questions about the frequency of usage of prescription and nonprescription medications; the frequency, amount, and trimester of use of cocaine, alcohol, cigarettes, marijuana, opiates, phencyclidine, and other street drugs, as well as tranquilizers, amphetamines, and barbiturates; the form of cocaine used; the disruptiveness of substance abuse to the person’s life; and history of substance abuse.
Demographic and lifestyle variables also were collected using structured interviews conducted by staff members. Questions included age, living arrangements, educational achievement, sources of income, family history of substance abuse, and information about other children.
RESULTS
Drug Use Patterns
Of the 323 subjects, 105 (32.5%) used cocaine. Of these, 57% smoked crack, 19% snorted cocaine, 21% smoked freebase cocaine, and 2% used a combination of methods excluding crack. There were 140 women (43.3%) who were negative for the screened substances and did not admit any use of cocaine, cigarettes, alcohol, or marijuana during pregnancy, 9 women (2.8%) were determined to have used marijuana with or without concomitant use of alcohol and/or cigarettes, and 69 women (21.4%) admitted cigarette and/or alcohol use only.1
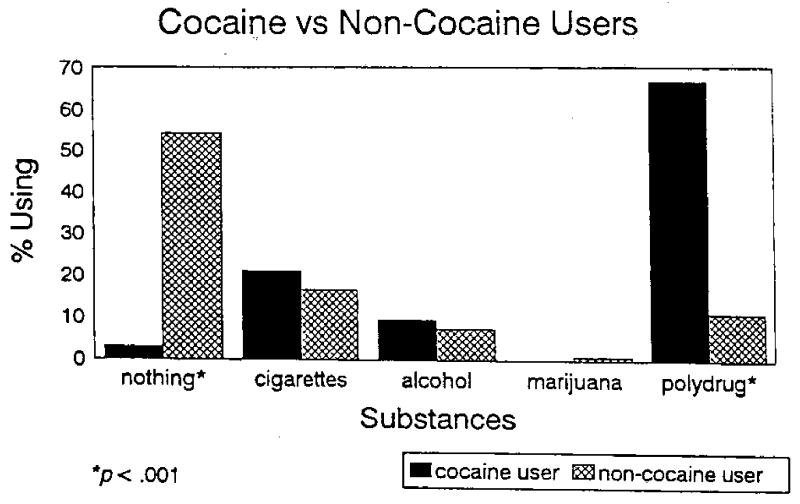
Figure 1 displays the relative use of no soft drugs, cigarettes, alcohol or marijuana alone, or a combination of cigarettes, alcohol, and/or marijuana (polydrug) by cocaine and non-cocaine users. Non-cocaine users were significantly more likely to have used none of the soft drugs (64.2% non-cocaine users vs 2.9% cocaine users, χ2(1) = 108.2, p < .001), while users of cocaine were significantly more likely to have been polydrug consumers (38.1 % cocaine users vs 7.8% non-cocaine users consumed alcohol and cigarettes during pregnancy, χ2(1) = 44.8, p < .001; 5.7% cocaine users vs .5% non-cocaine users smoked cigarettes and marijuana during pregnancy, Fisher’s Exact Test, p < .01; and 21.0% cocaine users vs 1.8% non-cocaine users consumed cigarettes, marijuana, and alcohol during pregnancy, χ2(1) = 35.0, p < .001). There were no differences between cocaine users and non-cocaine users in smoking cigarettes alone, just alcohol drinking or just marijuana use during pregnancy (16.5% vs 21.0% cigarette, 7.3% vs 9.5% alcohol and .9% vs 0% marijuana, for non-cocaine users and users respectively). There were too few women who used the combination of alcohol and marijuana with or without cocaine (2 in non-cocaine user group, 1 in cocaine user group) to determine whether the use of this combination of substances differs reliably between these groups.
Fig. 1.
Substance use during pregnancy.
Site Differences
The drug use pattern in two study sites, northwestern Philadelphia and Trenton, New Jersey, were compared. Northwestern Philadelphia is an inner-city urban neighborhood, with predominantly African-American residents. It is one section of a large (population 1,585,577), heterogeneous eastern city, where 39.9% of the overall population is African-American. The median income for a family of four is $24,603, with 2.2% of the resident families earning above $100,000. Trenton is a smaller (population 88,675), more homogeneous state capital city, in which 49.3% of the population is African-American. The median income is $25,719, with 1.5% of the resident families earning over $100,000. The two cities are approximately 40 miles apart.
The use of cigarettes, alcohol, marijuana, or any combination of these substances, as well as use of none of these substances during pregnancy, was compared across sites within the cocaine-using and non-cocaine-using groups. The only significant difference was in alcohol use among non-cocaine users. In Trenton, 11.4% of these subjects reported alcohol use during pregnancy, compared to 3.5% in Philadelphia (χ2(1) = 5.0, p < .03). The difference in the number of women who claimed to have used none of these substances during pregnancy approached significance among non-cocaine users. In Trenton, 58.1% fell into this category compared to 69.9% of the women in Philadelphia (χ2(1) = 3.3, p < .07).
Differences in Demographic and Lifestyle Variables
A number of demographic and lifestyle variables were compared across three groups: subjects who used cocaine during their pregnancies; those who used alcohol, cigarettes, and/or marijuana but no cocaine (soft drug users); and subjects who used none of these substances (abstainers). Table 1 presents the data. The three groups were compared on continuous variables using one-way analyses of variance. The Duncan Multiple Range Test was used post hoc to locate the significant group differences. Categorical variables were analyzed using chi-square analyses or Fisher’ Exact Test. Differences in drug use patterns between Trenton and Philadelphia were tested for each dependent variable and will be noted if significant.
Table 1.
Comparison of Cocaine Users, Soft Drug Users, and Abstainers on Demographic and Lifestyle Variables
| Abstainers | Soft drug users | Cocaine users | |
|---|---|---|---|
| Mother’s age (years):*** | |||
| M | 22.6a | 24.3b | 29.2c |
| SD | 4.8 | 6.2 | 4.5 |
| N | 139 | 78 | 104 |
| Mother’s education (years in school): | |||
| M | 11.4 | 11.1 | 11.5 |
| SD | 1.4 | 1.3 | 1.5 |
| N | 139 | 76 | 104 |
| Number live births:*** | |||
| M | 1.2a | 1.4a | 2.6b |
| SD | 1.3 | 1.4 | 1.9 |
| N | 139 | 78 | 104 |
| Number moves in previous year** | |||
| M | .60a | .82a,b | 1.13b |
| SD | 1.0 | 1.1 | 1.6 |
| N | 139 | 78 | 104 |
| Number people ≥ 18 years in household: | |||
| M | 2.3 | 2.2 | 2.4 |
| SD | 1.0 | 1.1 | 2.0 |
| N | 138 | 77 | 99 |
| Number people < 18 years in household: | |||
| M | 2.3 | 2.1 | 2.1 |
| SD | 1.6 | 1.5 | 1.9 |
| N | 138 | 77 | 99 |
| Married: | |||
| % | 14 | 14 | 12 |
| Number | 19 | 11 | 12 |
| Lives alone:† | |||
| % | 14a | 24b | 23b |
| Number | 19 | 19 | 24 |
| Lives with partner and children: | |||
| % | 25 | 26 | 20 |
| Number | 34 | 20 | 21 |
| Lives with own family members:* | |||
| % | 62a | 49b | 47b |
| Number | 86 | 38 | 49 |
| Shelter/institution:*** | |||
| % | 0a | 1a | 10b |
| Number | 0 | 1 | 10 |
| Currently employed:† | |||
| % | 14a | 14a | 6b |
| Number | 20 | 11 | 6 |
| Currently in school:*** | |||
| % | 21a | 21a | 3b |
| Number | 29 | 16 | 3 |
| Partner currently employed: | |||
| % | 46 | 42 | 41 |
| Number | 25 | 15 | 14 |
| Partner currently in school: | |||
| % | 8 | 6 | 3 |
| Number | 4 | 2 | 1 |
| Main source of income—public assistance:** | |||
| % | 60a | 63a | 80b |
| Number | 83 | 49 | 83 |
| Main source of income—own or partner’s salary: | |||
| % | 21 | 19 | 12 |
| Number | 29 | 15 | 12 |
| Main source of income—other:* | |||
| % | 19a | 18a | 7b |
| Number | 26 | 14 | 7 |
| Partner/friends use illegal drugs:*** | |||
| % | 7a | 15b | 56c |
| Number | 9 | 12 | 57 |
| Partner/friends use alcohol:*** | |||
| % | 7a | 19b | 51c |
| Number | 10 | 15 | 50 |
| History of drug abuse in family of origin:* | |||
| % | 10a | 22b | 20b |
| Number | 14 | 17 | 21 |
| History of alcoholism in family of origin*** | |||
| % | 24a | 30a | 48b |
| Number | 33 | 23 | 50 |
p<.09
p<.05
p<.01
p<.001
Note. Values with different superscripts are significantly different. A value with superscript a,b is not different from values with a or b.
Age and parity
Analyses revealed significant differences in maternal age (F(2, 320) = 50.6, p < .001) and the number of previous live births (F(2, 320) = 28.0, p < .001). Cocaine users were oldest and had significantly more previous children than the other subjects. However, soft drug users were significantly older than abstainers. There was a significant group by site difference in the number of previous births (F(2, 311) = 10.5, p < .01), such that in Trenton, soft drug users had fewer previous births than abstainers. In Philadelphia, the number of previous live births among the soft drug users was intermediate between the number for abstainers and cocaine users.
Household
The number of moves in the previous year increased the more substantial the drug use. There was a significant group difference (F(2, 318) = 5.4, p < .01), with cocaine users having significantly less stable domiciles than abstainers. Soft drug users moved less often than cocaine users but more often than abstainers. The number of moves in this group did not differ significantly from that in either of the other groups.
There were a number of possible household situations in which the women lived during the pregnancy with or without other children. These included living with no other adults, living with a partner, living with extended family or friends, and living in a shelter or institution. There was a significant overall difference in the household situations during pregnancy of the different substance-using groups (χ2(6) = 25.4, p < .001). In order to identify which differences explained the overall significant finding, each type of situation was tested separately. The percentage of subjects living with their extended families differed (χ2(2) = 6.3, p < .05), as did the percentage living in shelters or institutions (χ2(2) = 19.2, p < .001). There was a trend for differences in living alone (χ2(2) = 5.1, p < .08). Cocaine and soft drug users were less likely to live in extended family situations and more likely to live alone during pregnancy than abstainers. Moreover, there was a difference between the sites, such that in Philadelphia, significantly more soft drug users lived alone than in Trenton (χ2(1) = 6.3, p < .02). In addition, cocaine users in both sites more often lived in a shelter or institution than women in the other groups. Therefore, both the stability of the living situation and the extent of isolation were greater among drug-using women.
Employment and income
Groups differed in the percentage working or in school during pregnancy (χ2(2) = 17.5, p < .001). Significantly fewer cocaine using women were employed or in school than soft drug users or abstainers.
There also was an overall difference in the main source of income during pregnancy (χ2(4) = 17.7, p < .01). The percentage of subjects in each group receiving public assistance differed (χ2(2) = 11.3, p < .01), as well as the percentage having an income source other than public assistance or salary (primarily disability insurance and family support; χ2(2) = 7.8, p < .03). Cocaine-using women were more likely than the others to be receiving public assistance and less likely to have another source of income. There was a difference in pattern of income between the two sites. In Philadelphia, the majority of all groups were receiving public assistance (no difference across groups), while in Trenton, significantly more cocaine-using women received public assistance, and a higher percentage of women in the other groups had other income sources (χ2(1) = 8.0, p < .01 comparing abstainers receiving public assistance in the two sites; χ2(1) = 7.1, p < .01 comparing soft drug users receiving public assistance in the two sites; χ2(1) = 5.2, p < .01 comparing abstainers with salaries in the two sites; χ2(1) = 3.4, p < .07 comparing soft drug users with other sources of income in the two sites).
Drug-using environment
There were significant differences in the extent to which the partners and friends of women in the different groups used illegal drugs (χ2(2) = 82.1, p < .001) and alcohol (χ2(2) = 18.4, p < .001), as well as having a history in their own families of drug (χ2(2) = 5.9, p < .05) and alcohol abuse (χ2(2) = 16.5, p < .001). In general, the worse the substance abuse, the higher these environmental risks. Cocaine-using women were significantly more likely than abstainers or soft drug users to have partners who used illegal drugs and alcohol. The soft drug users also were significantly more likely than abstainers to have peers who used illegal substances or alcohol. Cocaine users, as well as soft drug users, reported a family history of drug use more often than abstainers, while a family history of alcoholism was significantly more frequent among the cocaine users only.2
Controlling for age difference
As the number of women who used cocaine tended to be older than those who did not, there was a possibility that age, rather than drug use status, accounted for many of the differences in these lifestyle and demographic variables. To explore this potential confound, only the younger half of the sample (less than the median age of 24.5 years) was used for comparisons of these variables, There were 101 nondrug users, 45 cigarette/alcohol and/or marijuana users, and 16 cocaine users under 24.5 years of age. The direction of the relationships remained the same for all of the variables except having a family history of drug abuse. For that variable the differences among the groups were not significant. Similarly, on some of the variables, differences that were significant for the total sample were only marginally or nonsignificant in the analyses with the smaller number of subjects. The strongest relationships among the younger subjects were that cocaine users were more likely to live alone or in shelters/institutions during their pregnancies than either of the other groups, and their partners and friends were much more likely to use alcohol and drugs.
The number of previous live births was examined separately in relation to age. The correlation between these variables was .49 (p < .001). However, an analysis of covariance using the three drug groups as the independent variable and maternal age as the covariate indicated that there was still a significant effect of drug use on number of live births after controlling for age (F(2, 320) = 6.3, p < .01). Similarly, a point biserial correlation between maternal age and student status resulted in a significant, but moderate, correlation (r = −.22, p < .001).
DISCUSSION
These analyses support the conclusion that cocaine use among inner-city pregnant women, as for other populations, is associated with soft drug use, disrupted and unsupportive life circumstances, as well as a substance-using environment (16, 19–22). In this sample, the cocaine users were likely to be consuming alcohol, cigarettes, and to a lesser extent marijuana, in addition to cocaine. Pregnant women from the same population who did not use cocaine, however, were much less likely to use combinations of substances, and much more likely not to use any of the common legal substances known to be potentially harmful to the fetus.
Despite the demographic differences between the Trenton and Philadelphia sites, there were very few differences in drug use patterns. The only exception was the larger percentage of the non-cocaine-using sample, which consumed alcohol during pregnancy in Trenton. While the cities are somewhat different, especially in size, the inner-city neighborhood of northwestern Philadelphia may be very similar to the inner city of Trenton in demographic characteristics. In addition, the cities are geographically close, so it is not surprising that the drug use patterns are so similar. Nevertheless, there were a small number of differences in the patterns of demographic and lifestyle variables across the substance use groups between the two sites, which are discussed below.
Cocaine-using women in our sample tended to be older, consistent with reports of others (23). They also had significantly more previous children, but this was not entirely accounted for by their age. Cocaine use disinhibits sexual behavior and impairs judgment about unprotected sexual activity (19, 24). This may account for the greater number of pregnancies and births among cocaine-using women.
These cocaine-using pregnant women were at much greater psychosocial risk than nondrug-using women from the same communities. Their home situations seemed to be less stable, as evidenced by the finding that they moved significantly more often than nondrug users in the previous year. They had less support and were more socially isolated, evidenced by more than one-third of them living alone or in shelters/institutions, as opposed to with extended families, during their pregnancies. More than the other groups, at least in Trenton, the main source of income of cocaine-using women (80%) was public assistance. Cocaine users were less likely to be in school (only moderately related to age, r = −.22, p < .001) and were much more likely to be living in a drug- and alcohol-abusing environment. Interestingly, a larger number of cocaine users had family histories of alcoholism than drug abuse.
It is significant that women who did not use cocaine during their pregnancies, but did smoke cigarettes and/or use alcohol, showed an increased likelihood of most of the same disruptive lifestyle characteristics as the cocaine users. In fact, in Philadelphia, the soft drug users were as isolated in their living situations and as dependent on public assistance during pregnancy as the cocaine users.
These data are consistent with, but do not prove, the proposition that cigarette, alcohol, and marijuana users are more likely to go on to develop a cocaine habit (25). Our finding that younger women who are not yet using cocaine, but are using these soft drugs, are already living in less stable and less supportive environments suggests that there may be few social mechanisms in their lives counteracting the initiation of cocaine use. This group also is more likely to have had drugs and alcohol abuse in their families and to have friends who are substance users than the women who abstain from smoking and drinking during their pregnancies.
Whether any of these characteristics cause drug abuse, or are the result of it, is impossible to determine from these analyses. However, the findings in these samples confirm the multiple problems associated with drug use among young women of childbearing age in urban environments. Intervention directed at teenage women who smoke and drink, particularly if there is a history of substance abuse in their own families, and intervention that provides psychosocial support, might be the most efficient strategy for curbing exposure of countless fetuses to teratogenic substances. In addition, such interventions might help improve the postnatal environments into which these infants are born.
As with most studies of this kind, certain sampling biases were unavoidable. This is a self-selected sample; thus, conclusions about demographic and lifestyle differences may not be applicable to women who did not volunteer to participate in the study. However, this bias may have led to more conservative findings, as the women who did participate may have been the most organized and resilient. In addition, we have relied to a certain extent on the women’s reports of their substance use during pregnancy, as well as the demographic and lifestyle information. Support for the reliability of the current findings comes from their consistency with similar results of other studies. Future research with diverse samples will help determine to what extent these findings can be generalized.
Acknowledgments
This research was supported by the National Institute on Drug Abuse Grant R01 DA07109 to Michael Lewis.
Footnotes
The marijuana users are grouped with the cigarette and alcohol users in the analyses due to their small number. To ensure that they were not contributing inordinately to any findings for non-cocaine substance use, all analyses were repeated eliminating marijuana users from both the cocaine and soft drug-using groups.
In order to determine whether the elevated risk factors in the soft drug-using group were explained by the marijuana users, the same variables were compared for abstainers, cocaine users, and cigarette and/or alcohol users. All subjects who had used marijuana, whether in combination with cocaine or not, were eliminated. Only 10 women had used marijuana and not cocaine. The results remained substantially the same. The significance of only one difference changed when the marijuana users were eliminated. There was a slight increase in the percentage of alcohol and/or cigarette users who lived with extended families (51%) when those who had used marijuana were excluded, reducing the difference with abstainers (62%) to a nonsignificant level.
Contributor Information
Margaret Bendersky, Institute for the Study of Child Development, University of Medicine and Dentistry of New Jersey, Robert Wood Johnson Medical School, New Brunswick, New Jersey 08903-0019.
Steven Alessandri, Department of Child Psychiatry, Medical College of Pennsylvania, Philadelphia, Pennsylvania
Patricia Gilbert, Mercer Medical Center, Trenton, New Jersey
Michael Lewis, Institute for the Study of Child Development, New Brunswick, New Jersey 08903-0019..
References
- 1.Chasnoff I, Bussey M, Savitch R, et al. Chemical and laboratory observations: Perinatal cerebral infarction and maternal cocaine use. J Pediatr. 1986;108:456–459. doi: 10.1016/s0022-3476(86)80896-4. [DOI] [PubMed] [Google Scholar]
- 2.Moore T, Sorg J, Miller L, et al. Hemodynamic effects of intravenous cocaine on the pregnant ewe and fetus. Am J Obstet Gynecol. 1986;155:883–888. doi: 10.1016/s0002-9378(86)80044-8. [DOI] [PubMed] [Google Scholar]
- 3.Rosenak D, Diamant Y, Yaffe H, et al. Cocaine: Maternal use during pregnancy and its effects on the mother, the fetus, and the infant. Obstet Gynecol Survey. 1990;45:348–359. [PubMed] [Google Scholar]
- 4.Chasnoff I, Landress H, Barrett M. The prevalence of illicit drug or alcohol abuse during pregnancy and discrepancies in mandatory reporting in Pinellas County, Florida. N Engl J Med. 1990;322:102–106. doi: 10.1056/NEJM199004263221706. [DOI] [PubMed] [Google Scholar]
- 5.Chasnoff I. Drug use and women: Establishing a standard of care. Ann N Y, Acad, Sci. 1989;562:208–210. doi: 10.1111/j.1749-6632.1989.tb21019.x. [DOI] [PubMed] [Google Scholar]
- 6.Clayton R. Cocaine Use in the U.S.: In a Blizzard or Just Being Snowed (NIDA Research Monograph 65) National Institute on Drug Abuse; Rockville, Maryland: 1986. pp. 8–34. [PubMed] [Google Scholar]
- 7.Frank D, Zuckerman B, Amaro H, et al. Cocaine use during pregnancy: Prevalence and correlates. Pediatrics. 1988;82:888–895. [PubMed] [Google Scholar]
- 8.Greer J. The drug babies. Exceptional Children. 1990;56:382–384. doi: 10.1177/001440299005600501. [DOI] [PubMed] [Google Scholar]
- 9.Little B, Snell L, Palmore M, et al. Cocaine use in pregnant women in a large public hospital. Am J Perinat. 1988;5:206–207. doi: 10.1055/s-2007-999686. [DOI] [PubMed] [Google Scholar]
- 10.Hurt H, Brodsky N, Betancourt L, et al. Cocaine-exposed children: Follow-up through 30 months. Develop Behav Pediatr. 1995;16:29–35. [PubMed] [Google Scholar]
- 11.Lewis M, Bendersky M. Mothers, Babies and Cocaine: The Role of Toxins in Development. Erlbaum, Hillsdale; New Jersey: 1995. [Google Scholar]
- 12.Schutter L, Brinker R. Conjuring a new category of disability from prenatal cocaine exposure: Are the infants unique biological or care taking casualties? Topics in Early Childhood Special Educ. 1992;11:84–111. [Google Scholar]
- 13.Lester B, Corwin M, Sepkoski C, et al. Neurobehavioral syndromes in cocaine-exposed newborn infants. Child Develop. 1991;62:694–705. doi: 10.1111/j.1467-8624.1991.tb01563.x. [DOI] [PubMed] [Google Scholar]
- 14.Rodning C, Beckwith L, Howard J. Characteristics of attachment organization and play organization in prenatally drug-exposed toddlers. Develop Psychopathol. 1989;1:277–289. [Google Scholar]
- 15.Rodning C, Beckwith L, Howard J. Prenatal exposure to drugs: Behavioral distortions reflecting CNS impairment? Neurotoxicology. 1985;10:629–634. [PubMed] [Google Scholar]
- 16.Amaro H, Zuckerman B, Cabral H. Drug use among adolescent mothers: Profile of risk. Pediatrics. 1989;84:144–151. [PubMed] [Google Scholar]
- 17.Fried P, O'Connell C, Watkinson B. 60- and 72-month follow-up of children prenatally exposed to marijuana, cigarettes, and alcohol: Cognitive and language assessment. Develop, Behav, Pediatr. 1992;13:383–391. [PubMed] [Google Scholar]
- 18.Randall T. Cocaine, alcohol mix in body to form even longer lasting, more lethal drug. JAMA. 1992;267:1043–1044. [PubMed] [Google Scholar]
- 19.Kang SY, Magura S, Shapiro J. Correlates of cocaine/crack use among inner-city incarcerated adolescents. Am J Drug Alcohol Abuse. 1994;20:413–429. doi: 10.3109/00952999409109181. [DOI] [PubMed] [Google Scholar]
- 20.Kumpfer K. Special populations: Etiology and prevention of vulnerability to chemical dependency in children of substance abusers, in Youth at High Risk for Substance Abuse. In: Brown BS, Mills AR, editors. DHHS Publication ADM 87–1537), Alcohol, Drug Abuse and Mental Health Administration. US Government Printing Office; Washington, D.C.: 1987. [Google Scholar]
- 21.Kumpfer K, Turner C. The social ecology model of adolescent substance abuse: Implications for prevention. Int J Addict. 1990–1991;25:435–463. doi: 10.3109/10826089009105124. [DOI] [PubMed] [Google Scholar]
- 22.Lopez J, Redondo L, Martin A. Influence of family and peer group on the use of drugs by adolescents. Int J Addict. 1989;24:1065–1082. doi: 10.3109/10826088909047329. [DOI] [PubMed] [Google Scholar]
- 23.Woods NS, Behnke M, Eyler FD, Conlon M, Wobie K. In: Cocaine use among pregnant women: Socioeconomic, obstetrical and psychological issues, in Mothers, Babies and Cocaine: The Role of Toxins in Development. Lewis M, Bendersky M, editors. Erlbaum, Hillsdale; New Jersey: 1995. [Google Scholar]
- 24.Kandel D. Epidemiological and psychosocial perspectives on adolescent drug use. J Am Acad Child Psychiatry. 1982;21:328–347. doi: 10.1016/s0002-7138(09)60936-5. [DOI] [PubMed] [Google Scholar]
- 25.Kandel D, Yamaguchi K, Chen K. Stages of progression in drug involvement from adolescence to adulthood: Further evidence for the gateway theory. J Stud Alcohol. 1992;53:447–457. doi: 10.15288/jsa.1992.53.447. [DOI] [PubMed] [Google Scholar]