Abstract
Bedtime resistance, a common pediatric problem, that was displayed by 4 unrelated 3-year-old children was treated with the bedtime pass (i.e., provision of a small notecard exchangeable for one trip out of the bedroom after bedtime) plus extinction. Bedtime resistance was eliminated for all participants. Further, treatment did not produce extinction bursts, as is common when using extinction procedures alone. Component analysis with 1 participant suggested that use of both components of the intervention produced the best outcomes. Findings extend the literature on the treatment of pediatric bedtime resistance as well as the application of behavior analysis to clinical psychology and pediatric care.
Keywords: bedtime resistance, bedtime behavior problems, behavioral treatment, bedtime pass
Active bedtime resistance (i.e., calling out from or leaving one's room after bedtime) is one of the most common difficulties in young children, seen in approximately 20% to 25% of children 1 to 5 years of age (see Metzler & Mindell, 2004). According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR; American Psychiatric Association, 2000), bedtime resistance may be classified as dyssomnia not otherwise specified, and bedtime problems can be the fundamental component of behavior clusters that are classifiable with other diagnoses (e.g., oppositional defiant disorder, attention deficit hyperactivity disorder). Left untreated, bedtime problems can persist for years (Kataria, Swanson, & Trevathon, 1987). Further, pediatric sleep disturbances are related to various adverse outcomes (e.g., disturbed cognitive functioning, Steenari et al., 2003; increased behavior problems, Paavonen et al., 2002; poor parental satisfaction, Gelman & King, 2001). Thus, effective intervention is important.
Interventions for pediatric bedtime resistance typically are behavioral in nature, the most common being extinction (i.e., planned parental ignoring). Although it is effective, parental acceptability of extinction is often low (France, 1994; Friman et al., 1999), partly due to temporary increases in bedtime resistance often seen early in intervention (i.e., the extinction burst; see Blum & Friman, 2000). Alternatively, the bedtime pass (Friman et al.) involves (a) a small notecard exchangeable for one trip out of the bedroom after being put to bed and (b) extinction. Two male siblings, ages 3 and 10 years, were successfully treated with the bedtime pass, without observation of extinction bursts during initial intervention periods. Further, 20 parents rated the intervention as more acceptable than traditional extinction.
Additional research on the bedtime pass is warranted to address two primary issues. First, although Friman et al. (1999) suggested that their results supported 3 years of age as the lower limit for effective use of the bedtime pass, patterns of obtained results suggested caution in this statement. Specifically, the older sibling used the pass on 8 of the 13 opportunities, but the 3-year-old used it only twice. Further, suppression of bedtime resistance was not achieved during the initial treatment implementation with the younger sibling. Thus, improvements in the older sibling's behavior may have facilitated those of the younger child. Second, although Friman et al. speculated that use of the pass might mitigate the likelihood of an extinction burst whereas extinction is the active component for behavior change, they provided no evidence regarding the necessity of both components. This study attempts a systematic replication of Friman et al. by focusing on two variations: targeting a group composed solely of 3-year-olds and providing an initial attempt at a component analysis.
Method
Participants
Four typically developing 3-year-old Caucasian boys participated. Parents, who responded to posted flyers about the study, referred all participants. For all, parents were concerned about frequent calling out from or leaving the room after bedtime. Resistance was reportedly problematic due to high frequency, long duration, or both. According to parent ratings on the Eyberg Child Behavior Inventory (Eyberg & Pincus, 1999), the children fell into the normal or nonclinical range with regards to the presence of generalized disruptive behavior problems. All parents reported some response to bedtime resistance (e.g., catering to the child's request, scolding the child, allowing the child to stay up). Each child slept in his own bedroom.
Measurement and Research Design
Each night, the child's mother measured frequency of calling out from or leaving the bedroom after bedtime; the child's father collected interobserver data every 3rd to 5th night. Long and short cries were counted as one instance of calling out; leaving the room was counted when the child passed through the door of his bedroom (Friman et al., 1999). Use of the pass was also recorded during intervention phases; this was not counted as bedtime resistance (Friman et al.). Interobserver agreement, calculated by dividing the frequency of bedtime resistance indicated by the primary observer by that of the secondary observer, was 95% for Jim and 100% for Craig, Walter, and Greg. A nonconcurrent multiple baseline across participants with an ABAB withdrawal design (A = baseline; B = pass plus extinction) was used to investigate treatment effectiveness with 3 participants (Jim, Craig, and Walter). An ACABAB design was used with Greg. The C phase involved use of the pass while responding to bedtime resistance as usual (i.e., pass alone), and B involved the combined intervention (i.e., pass plus extinction).
Procedure
Parents had one meeting with the researcher, during which informed consent was obtained, and data collection and general intervention procedures were described (with a written description provided; copy available from the first author). Following the initial meeting, all contact between the investigator and parents occurred via telephone and e-mail. Parents reported on obtained data daily by either sending an e-mail to or leaving a voice mail message with the investigator.
During baseline, parents were instructed to respond to bedtime behavior problems in their usual fashion. After completing this phase, the investigator contacted parents via the telephone and reviewed the specific details regarding treatment. During intervention, the child was given a notecard exchangeable for one trip out of the bedroom for a short (i.e., less than 3 min), specific activity (e.g., use restroom, one more hug). After completing the action, the child surrendered the pass and was returned to bed. The parents of Jim, Craig, and Walter were instructed to return the child to his room without comment if he came out and to ignore calling out if either occurred after use of the pass. With Walter, there was an unplanned variation in treatment implementation during the second treatment phase (i.e., Nights 41 through 51) such that his parents allowed him to use the pass but failed to implement extinction. To investigate the effects of the pass with and without extinction, Greg's parents were initially told to continue to respond to bedtime resistance in their typical fashion. During later phases, they were instructed to use the pass plus extinction.
Results
Figure 1 shows nightly occurrence of bedtime resistance across experimental phases for each participant. High and variable rates of calling out or leaving the room were observed in baseline phases, and reduced rates were observed during intervention. These effects usually occurred rapidly. In addition, the reductions in bedtime resistance were achieved without being accompanied by extinction bursts that are often seen with extinction-based procedures. With Greg, resistance approximated baseline rates during initial use of the pass plus extinction; further, reduction of target behavior occurred less rapidly when the combined intervention was used compared to other participants. However, calling out or leaving the room never occurred more frequently during intervention than during baseline. Further, resistance approximated baseline rates on 1 night each for 2 participants (i.e., Night 19 for Jim and Night 64 for Walter), with parental report indicating that these spikes were accompanied by unusual events that probably influenced the results (i.e., complaints of illness from Jim, sister calling to Walter).
Figure 1. Nightly frequency of combined calling out from and leaving the room.
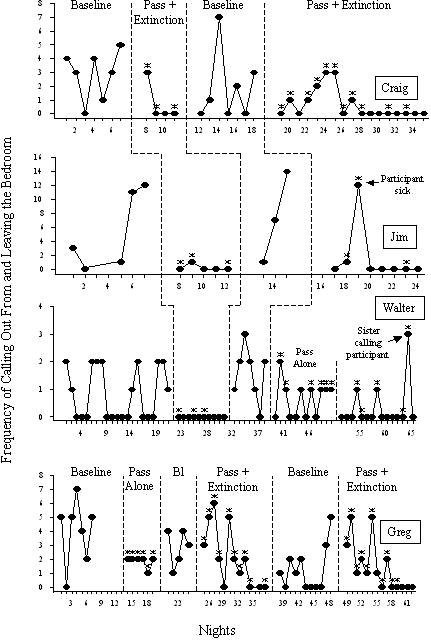
Data are presented to reflect the passage of time, and nights with missing data points represent lack of data collection by care providers. Asterisks indicate nights on which participants used the bedtime pass. BL = baseline.
Data from 2 participants offer tentative support for the benefit of both components of the bedtime pass. Unplanned use of the pass without extinction by Walter's parents resulted in bedtime resistance at rates similar to baseline (combined baseline M = 1.0, range, 0 to 3; unplanned use of pass alone M = 0.67, range, 0 to 2). When consistent application of extinction resumed on Night 52, resistance decreased (M = 0.29, range, 0 to 3). The planned component analysis conducted with Greg showed that use of the pass alone resulted in decreased frequency and variability of bedtime resistance (final 3 nights of initial baseline M = 3.67, range, 2 to 5; final 3 nights of pass alone M = 1.67, range, 1 to 2). However, use of both treatment components (pass plus extinction) resulted in elimination of resistance (final 3 nights of combined treatment M = 0).
Discussion
The results of this study extend the literature on the treatment of bedtime resistance in general and the use of the bedtime pass in particular. First, the results show that the pass effectively reduced bedtime resistance in 3-year-old children who were the only targets of the intervention (as distinct from Friman et al., 1999). These results help to establish that the intervention is effective with children of this age. Second, these results demonstrated that the bedtime pass reduced bedtime resistance without producing an extinction burst, an effect that could heighten treatment acceptability and thereby improve treatment adherence (France, Henderson, & Hudson, 1996; Rapoff, 1999; Rickert & Johnson, 1988). This is important given that inconsistent application of extinction encourages persistence of bedtime resistance and decreases responsiveness to future extinction attempts (Pritchard & Appelton, 1988). Third, the results of the component analyses indicated that both the pass and extinction were necessary to produce optimal results. Although both Walter and Greg used the pass more frequently during the pass-alone phases than in the pass plus extinction phases, elimination of resistance occurred only when the combined intervention was instituted. With Greg, reductions in bedtime resistance occurred more slowly when the combined intervention was implemented. The reason for this is unclear, although the possibility that the order in which treatment variations were presented affected data patterns cannot be ruled out.
It is important to speculate how the bedtime pass reduces bedtime resistance without producing an extinction burst. One possibility involves viewing the program as a form of differential reinforcement of alternative behavior (DRA; e.g., Vollmer & Iwata, 1992). DRA interventions often include both reinforcement for positive social behavior and extinction of problematic responses, and the combination has been shown to reduce the probability of extinction bursts (e.g., Bowman, Fisher, Thompson, & Piazza, 1997; Fisher, Kuhn, & Thompson, 1998). In the pass program, the pass is a communicative alternative to resistant behavior and its use results in satisfaction of one request, which is a potentially reinforcing event (i.e., it is differentially reinforced). Further support for the DRA hypothesis is found in research showing that reinforcement of positive social behavior may not result in elimination of targeted problem behavior if reinforcement is still available for the problem behavior (e.g., Piazza et al., 1999; Shirley, Iwata, Kahng, Mazaleski, & Lerman, 1997). A similar result was observed during the current component analysis. Another plausible explanation of how the pass produces its effects involves the concept of manding (Skinner, 1957). Previous research has shown that treatment of problem behavior with differential reinforcement and extinction using signals (e.g., tone, picture) denoting reinforcement of mands reduced problem behavior without producing extinction bursts (e.g., Fisher et al., 1998). In the pass program, it is possible that the pass served as a stimulus that was discriminative for reinforcement of at least one mand (e.g., request for a trip to the bathroom). Clearly these possibilities are speculative and are offered here to guide future research.
These results should be interpreted in light of several limitations. First, external validity of the combined bedtime pass intervention is limited because the component analysis was not conducted with each child. As a related issue, data on the component analysis with Greg are potentially confounded by the fact that experimental phases were not of similar lengths. Whether continued use of the pass alone would have resulted in further reductions of resistance remains unclear. Second, treatment fidelity was not systematically evaluated. The fact that Walter's parents failed to implement extinction procedures when instructed highlights this as a potentially important issue. Third, explanations from parents regarding apparent aberrant data (e.g., illness on a given night) were not collected systematically. It is unclear whether similar contextual variations existed at other points in the study but were not reported. Fourth, due to miscommunication, Greg's parents implemented the initial intervention after several nights of missed data collection (i.e., Nights 8 to 13) without obtaining additional baseline data. Fifth, this study offers only speculation regarding the link between the bedtime pass and other lines of behavior-analytic research (e.g., DRA, manding).
These limitations notwithstanding, the positive results here (and in Friman et al., 1999) warrant additional research. In addition to the suggestion above about mechanism, future research should address issues such as promotion of parental adherence to treatment procedures, child and family variables that affect intervention success, and technology transfer to applied settings (e.g., prescribed by pediatricians). Further, experimental designs that offer empirical analysis of speculations regarding why the intervention works are needed to solidify its theoretical basis. More systematic and comprehensive investigation of the relative importance of both treatment components (i.e., pass and extinction) is needed to further establish the external validity of the intervention. Finally, analysis of level of adherence to, and application of, the intervention is warranted, given other research that has shown that differential reinforcement procedures may be effective despite less than optimal implementation (Vollmer, Roane, Ringdahl, & Marcus, 1999). Given the extent of bedtime resistance exhibited by children in the United States (see Metzler & Mindell, 2004), additional research on the pass program may not only add to extant research on bedtime problems but also help to extend behavior analysis into mainstream clinical psychology and primary pediatric medical care.
Acknowledgments
I thank Nancy Farrell and Wendy DeCourcey for assistance with data collection and Cynthia Anderson and Douglas Woods for assistance with design.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., text rev.) Washington, DC: Author; 2000. [Google Scholar]
- Blum N, Friman P.C. Behavioral pediatrics: The confluence of applied behavior analysis and pediatric medicine. In: Carr J, Austin J, editors. Handbook of applied behavior analysis. Reno, NV: Context Press; 2000. pp. 161–185. [Google Scholar]
- Bowman L.G, Fisher W.W, Thompson R.H, Piazza C.C. On the relation of mands and the function of destructive behavior. Journal of Applied Behavior Analysis. 1997;30:251–265. doi: 10.1901/jaba.1997.30-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyberg S, Pincus D. Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Inventory: Professional manual. Lutz, FL: Psychological Assessment Resources, Inc; 1999. [Google Scholar]
- Fisher W.W, Kuhn D.E, Thompson R.H. Establishing discriminative control of responding using functional and alternative reinforcers during functional communication training. Journal of Applied Behavior Analysis. 1998;31:543–560. doi: 10.1901/jaba.1998.31-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- France K.G. Handling parents' concerns regarding behavioural treatment of infant sleep disturbance. Behavioural Change. 1994;11:101–109. [Google Scholar]
- France K.G, Henderson J.M.T, Hudson S.M. Fact, act, and tact: A three-stage approach to treating the sleep problems of infants and young children. Child and Adolescent Psychiatric Clinics of North America. 1996;5:581–599. [Google Scholar]
- Friman P.C, Hoff K.E, Schnoes C, Freeman K.A, Woods D.W, Blum N. The bedtime pass: An approach to bedtime crying and leaving the room. Archives of Pediatric and Adolescent Medicine. 1999;153:1027–1029. doi: 10.1001/archpedi.153.10.1027. [DOI] [PubMed] [Google Scholar]
- Gelman V.S, King N.J. Wellbeing of mothers with children exhibiting sleep disturbance. Australian Journal of Psychology. 2001;53:18–22. [Google Scholar]
- Kataria S, Swanson M.S, Trevathon G.E. Persistence of sleep disturbances in preschool children. Behavioral Pediatrics. 1987;110:642–646. doi: 10.1016/s0022-3476(87)80571-1. [DOI] [PubMed] [Google Scholar]
- Metzler L.J, Mindell J.A. Nonpharmacologic treatments for pediatric sleeplessness. Pediatric Clinics of North America. 2004;51:135–151. doi: 10.1016/s0031-3955(03)00178-0. [DOI] [PubMed] [Google Scholar]
- Paavonen E.J, Almqvist F, Tamminen T, Moilanen I, Piha J, Räsänen E, et al. Poor sleep and psychiatric symptoms at school: An epidemiological study. European Child & Adolescent Psychiatry. 2002;17:10–17. doi: 10.1007/s007870200002. [DOI] [PubMed] [Google Scholar]
- Piazza C.C, Bowman L.G, Contrucci S.A, Delia M.D, Adelinis J.D, Goh H.L. An evaluation of the properties of attention as reinforcement for destructive and appropriate behavior. Journal of Applied Behavior Analysis. 1999;32:437–449. doi: 10.1901/jaba.1999.32-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pritchard A, Appelton P. Management of sleep problems in pre-school children. Early Childhood Development and Care. 1988;34:227–240. [Google Scholar]
- Rapoff M.A. Adherence to pediatric medical regimens. New York: Kluwer Academic/Plenum; 1999. [Google Scholar]
- Rickert V.I, Johnson C.M. Reducing nocturnal awakening and crying episodes in infants and young children: A comparison between scheduled awakenings and systematic ignoring. Pediatrics. 1988;81:203–212. [PubMed] [Google Scholar]
- Shirley M.J, Iwata B.A, Kahng S, Mazaleski J.L, Lerman D.C. Does functional communication training compete with ongoing contingencies of reinforcement? An analysis during response acquisition and maintenance. Journal of Applied Behavior Analysis. 1997;30:93–104. doi: 10.1901/jaba.1997.30-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner B.F. Verbal behavior. Cambridge, MA: Prentice Hall; 1957. [Google Scholar]
- Steenari J.R, Vountela V, Paavonen E.J, Carlson S, Fjällberg M, Aronen E.T. Working memory and sleep in 6- to 13-year-old schoolchildren. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:85–92. doi: 10.1097/00004583-200301000-00014. [DOI] [PubMed] [Google Scholar]
- Vollmer T.R, Iwata B.A. Differential reinforcement as treatment for behavior disorders: Procedural and functional variations. Research in Developmental Disabilities. 1992;13:393–417. doi: 10.1016/0891-4222(92)90013-v. [DOI] [PubMed] [Google Scholar]
- Vollmer T.R, Roane H.S, Ringdahl J.E, Marcus B.A. Evaluating treatment challenges with differential reinforcement of alternative behavior. Journal of Applied Behavior Analysis. 1999;32:9–23. [Google Scholar]


